Urgent Message: There are an estimated 250,000 visits annually associated with pediatric headaches in the United States, 84% of which are not treated according to best evidence-based practice (EBP). The development of an EBP headache and migraine pathway in a pediatric urgent care improved access to evidence-based guidelines and increased clinician confidence and knowledge regarding the diagnosis and management of headaches in children.
Sarah J. Nembu, DNP, APRN, FNP-C, CPNP-AC; Melissa R. Penkalski, DNP, APRN, CPNP-PC, AE-C
Citation: Nembu SJ, Penkalski MR. Development and Implementation of a Headache and Migraine Pathway in Pediatric Urgent Care: A Quality Improvement Initiative. J Urgent Care Med. 2024; 19(1):39-45
Abstract
Introduction: Fewer than 20% of pediatric patients presenting with headache or migraine are appropriately diagnosed or treated. In this study, a pathway to bring evidence-based practices into a pediatric urgent care (PUC) clinic was developed determine if it would increase appropriate treatment of headaches and migraine presentations and improve provider confidence and knowledge.
Methods: The effectiveness of the intervention was evaluated by 2 methods. First, a pre- and post-intervention electronic health record (EHR) data analysis of total patient encounters during a 6-month period was performed to determine practice trends and outcomes. Additionally, an anonymous pre- and post-intervention survey was administered to physicians, nurse practitioners (NP), and physician assistant/associates (PA) to assess clinicians’ level of confidence, perceived barriers, and knowledge about pediatric headaches. The pathway was presented to clinicians in a PUC monthly educational meeting. The presentation, which included explanation of the pathway, was also made available on the hospital intranet for clinicians to access after the meeting.
Results: Results included data analyzed from over 90,000 patient encounters. A total of 43 clinicians completed the survey. One percent of all patient encounters that were analyzed included a diagnosis of headache and/or migraine. In the post-intervention survey, clinicians reported a 10-20% increase in knowledge and 40% increase in confidence. Management practices of headache and/or migraine presentations, however, were unchanged after the intervention.
Conclusions: In this PUC educational intervention study, implementation of a headache/migraine provider pathway was associated with an increase in provider knowledge and confidence. While there was no significant change in diagnosis and management practice, the clinicians in the study practice setting were more adherent than comparable centers on average before the intervention. Implementation of a similar pathway in PUC settings may improve clinician confidence and knowledge of evidence-based care for pediatric headaches.
Introduction
There are an estimated 250,000 visits annually associated with pediatric headaches in the U.S. In 84% of cases, patients are not prescribed (or recommended) evidence-based medications.[1] The prevalence of headaches and migraines in the pediatric population is estimated at 50% and 9.1%, respectively; half of children with recurrent headaches will continue to have migraines as adults.[2]
Oskoui et al. established clinical guidelines for the treatment of acute migraines in children and adolescents.[3] This guideline was jointly developed by the American Academy of Neurology Institute (AANI) and the American Headache Society (AHS). It was adopted and accepted by the American Academy of Pediatrics (AAP),[4] American Academy of Neurology (AAN),[5] as well as the Child Neurology Society (CNS).3 The guidelines include how to accurately assess and diagnosis headaches and migraines in children, recommendations for abortive medications, treatment of associated symptoms, and education for headache prevention and home management.
The first step in headache management in children involves arriving at an accurate diagnosis. Having a solid basis for understanding of headache syndromes and their diagnostic criteria in children and adolescents is key to appropriate headache management. According to a retrospective chart review by Minen et al., of the 93.6% of pediatric patients who presented with headache—including 78.25% with a self-reported history of headache or migraine prior to presentation—only 12.3% received the most evidenced-based treatment.[6] There is extensive evidence on headache management ranging from expert opinion to systematic reviews,3 yet it is clear that many clinicians are not adopting guideline-based practices.
Headaches in children are expressed differently among various age groups, developmental stages, and cultures. Clinicians must understand these differences in pain presentations based on these factors. Children may describe pain from headaches as stabbing, squeezing, throbbing, or some form of dizziness, and 40% of all headache complaints affect uncertain locations of the head.[7] The International Headache Society (IHS) defines migraine without aura in children (age 18 and under) as at least 5 headaches over the past year lasting 2-72 hours in duration (if left untreated) with 2 of 4 additional features: 1.) pulsatile quality; 2.) unilateral, bilateral, or frontal; 3.) worsening with activity or limiting activity; 4.) moderate to severe in intensity AND are associated with either nausea, vomiting, photophobia, or phonophobia.[8] Migraine with aura comprises approximately 20% of migraines among children and is defined as having at least 2 attacks meeting the following criteria.
- One or more fully reversible aura symptoms (eg, visual, sensory, speech/language, motor, brainstem and retinal) AND
- At least 3 of the following: 1.) at least 1 aura spreading gradually over 5 minutes or more; 2.) symptoms occur in succession; 3.) each individual aura is 5-60 minutes in duration; 4.) at least 1 aura is unilateral; and/or 5.) aura is followed within 60 minutes by headache.8
Management
Approximately 75% of children have experienced a significant headache before the age of 15 years of age.[9] Despite the existence of evidence-based guidelines for management, guideline discordant treatment is common, and analgesia is often insufficient.9 For acute headache treatment, the guidelines established by Oskoui et al. in 20193 suggest management with simple analgesics (non-steroidal anti-inflammatory drugs [NSAIDs] or acetaminophen) as first line.[10],[11] In refractory headaches, the addition of antiemetics (eg, ondansetron or promethazine) followed by triptans is recommended; the guidelines also emphasize the importance of early treatment.[12] A systematic review of emergency department (ED) treatment for pediatric headaches showed treatments like NSAIDs and dopamine receptors antagonists (eg, prochlorperazine) were effective abortive treatments in the acute setting.[13] In a 2016 systematic review, ibuprofen was found to be most effective at a dose of 10 mg/kg and superior to acetaminophen and placebo. In the same review, acetaminophen was found to be superior to placebo.1 Based on data used to investigate NSAID use in one retrospective study, NSAIDs were considered the first line therapy for acute moderate intensity headache and triptans as the first line for high-intensity migraine attacks.[14] In children with a diagnosis of migraine, several triptans are approved by the Food and Drug Administration (FDA) for use in pediatric headache. Rizatriptan is approved for children 6-17 years of age and almotriptan, zolmitriptan nasal spray, and sumatriptan/naproxen are approved in ages 12-17 years.[15] In a qualitative systematic review conducted by Patniyot and Gelfand, sumatriptan nasal spray was the recommended treatment of adolescent migraines.1
Abortive therapies, which are central for the treatment of pediatric headaches, do not include opioids. Opioids, which can result in rebound headaches, are not recommended in any headache guidelines, yet continue to be utilized in acute care settings for children with severe headaches.13 A 2019 study found that up to 1 in 6 children with severe headaches were prescribed an opioid for headache and/or migraine.15
Unlike opioids, there is support in the literature for the use of dopamine receptor antagonists (DRAs) as abortive therapies for pediatric migraines, as these agents have been shown to improve pain and reduce nausea. Commonly available DRAs include medications such as promethazine and metoclopramide.1 In a 2020 inpatient study, Troy and Yonker found no difference between ondansetron and promethazine in children with migraine.[16] While not a DRA, 1 study showed that ondansetron had fewer side effects than DRAs and comparable efficacy for controlling nausea.[17] Antihistamines, specifically diphenhydramine, have been shown to reduce extrapyramidal effects that can occur with parenteral use of DRAs.16 The addition of anti-histamine may also improve relief of headache, but is also associated with increased risk of sedation.5,8
Evidence-based practice (EBP) refers to application of the highest quality evidence to inform clinical practice. The purpose of this quality improvement (QI) project was to develop and disseminate an evidence-based pediatric headache and migraine pathway to make EBP guidelines more readily accessible to clinicians in our institution and improve their confidence in caring for children presenting to PUC centers with headache.
Methods
The QI project was completed in an outpatient PUC setting in Fort Worth, Texas. The project institution’s UC centers are hospital-owned outpatient services and are comprised of 7 physical locations in the area with a combined annual volume of 150,000 patients. These clinics are staffed by over 80 physicians, NPs, and PAs. The clinician group is comprised of approximately 30% board certified pediatricians and 70% combined advanced practiced providers (APPs). This study was determined not to constitute human subject research by the Cook Children’s Health Care System Institutional Review Board (IRB), along with the Missouri State University IRB, and need for review was waived. There were 2 arms to this project: evaluation of changes in clinician practice patterns; and evaluation of clinician perspectives regarding evaluation and management of pediatric migraines.
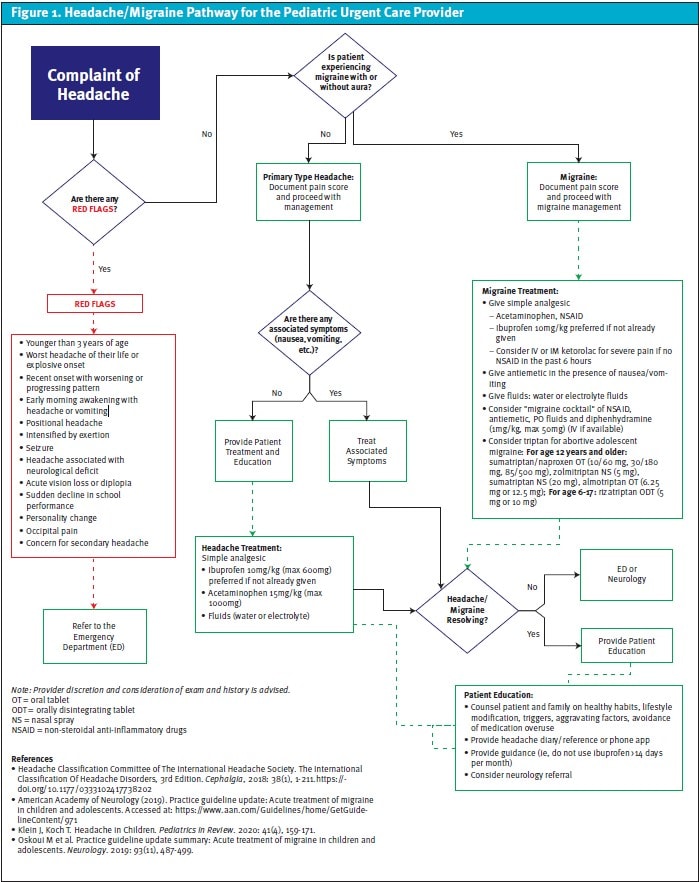
The authors completed a literature review and developed a pathway (Figure 1) by synthesizing the pre-existing guidelines established by AANI and AHS (adopted by CNS3, AAP4, and AAN5). The organization-specific pediatric headache and migraine pathway was developed to simplify access to EBP guidelines, including diagnostic criteria and management recommendations for children presenting with acute headache or migraine. After pathway development, the project leader presented the pathway and reviewed the most current evidence on the topic with the PUC clinicians in the group. The pathway itself was printed and posted in several PUC center physical locations and made available on the hospital intranet and via email. Clinicians were given the opportunity to complete a pre-intervention survey to evaluate their current practices. After 3 months, a post-intervention survey was administered to evaluate for satisfaction with the pathway and assess for change in confidence, knowledge, and guideline adherence.
To evaluate for changes in clinician practice in response to the intervention, patient data were retrospectively extracted in the 3 months prior to project implementation and then again during the 3 months post implementation. Data were extracted from EPIC, the organization’s electronic medical record (EMR, utilizing diagnosis codes for headache and migraine. The diagnoses search included any ICD-10 code subset of Headache R51* and Migraine G43*. Additional subsearch criteria were applied to the encounters to examine which of the medications available in clinic were administered (eg, acetaminophen, ibuprofen, ketorolac, diphenhydramine, fentanyl, hydrocodone, midazolam, and/or ondansetron) and prescribed for home use (eg, triptans).
To evaluate for changes in clinician perspectives, a 5-point Likert scale survey was administered pre- and post-intervention. Items included existing knowledge of EBP guidelines for diagnosis and management of pediatric headache and migraine, confidence in the ability to diagnose and educate families on the plan of care, use of society guidelines for medication management, documentation of pain scores, and recommendation for the patient to keep a headache log. An additional 7-question section of the survey listed symptoms and asked providers to select the appropriate diagnosis as “Headache,” “Migraine without aura,” “Migraine with aura,” “Headaches and Migraines,” “None,” and “Unsure.” In the post-intervention survey, access to the pathway was available if desired. Descriptive statistics (frequencies and percentages) were used to evaluate attitudes, beliefs and symptom responses. Statistical Package For Social Sciences (V. 25) was used to perform Wilcoxon signed rank test for ordinal data and the exact sign test for nominal data (involving dependent groups) to determine statistical significance (ie, p <0.05) between pre- and postsurvey items.
RESULTS
A total of 90,314 patient encounters were reviewed for inclusion among all 7 PUC centers. Pre-implementation data from the 3 months prior to implementation included 52,553 patient encounters. Among these, 513 met inclusion criteria diagnoses of headache, and 39 were included based on a diagnosis of migraine. During the 3-month post-implementation period, 40,781 encounters were reviewed, 326 met inclusion criteria based on diagnoses of headache, and 28 were included based on a diagnosis of migraine. Included encounters represent approximately 0.1% of all patient encounters during both time periods.
Headache management with acetaminophen, ibuprofen and/or ketorolac was provided in the PUC center 44% of the time in the pre-implementation period and 36% of the time post-intervention period. Migraine was treated with these same medications 64% of the time in both groups. No opioids were administered in the PUC center or prescribed for any patient encounter during either time period. Complementary therapies (ondansetron and/or DRA +/- diphenhydramine) discussed in the guidelines were used in 18% of the time pre-implementation encounters and 13% post-intervention for headache. The treatment of associated symptoms of migraine was completed 62% in the pre-implementation period and among 75% of patients post-intervention.
There were approximately 80 clinicians practicing in the UC centers during the project implementation period. A total of 43 of 80 clinicians completed the pre-survey and 33 of 80 clinicians completed the post-survey for a response rate of 41.3%. Of the respondents, 24% were physicians/pediatricians, and 76% were APPs. Also, 30% of clinicians reported <5 years of clinical experience.
On both pre- and post-surveys, 100% of providers reported they believed they use EBP, and 98% of clinicians reported that they intended to utilize the pathway. Pathways for the management of various diseases are available to providers on an as needed basis but were previously underassessed. A Wilcoxon signed rank test indicated there was a statistically significant increase (Z= -2.33; p= 0.02) in reported knowledge of simply accessing the pathway located on the intranet or through email and printed copy—from 71.2% to 93.9%. Pre-intervention, 39.6% of clinicians stated they “often” or “always” document pain scores. In the post-intervention survey, a statistically significant increase was noted in the proportion of clinicians who stated that they “often” or “always” document pain scores with 63.3% of respondents selecting these options (Wilcoxon Signed-Ranks Test, Z= -2.31; p= 0.021).
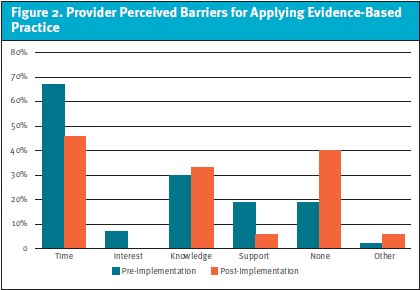
Perceived barriers to applying EBP also decreased. Time factors as an issue decreased from 67.4% to 45.5% (p>0.05), lacking interest in applying EBP decreased from 7% to 0% (p>0.05), and lacking support in applying EBP decreased from 18.6% to 6.1% (p>0.05). Overall, the proportion of providers reporting no perceived barriers to applying EBP decreased by 21% (p>0.05) from the pre- to post-intervention surveys. (Figure 2)
The pre- and post-intervention surveys asked providers to rank how confident they were in their ability to diagnose headache and migraine and their ability to reference professional society guidelines for pediatric headache management. While there were no significant differences pre- and post-intervention, there was elimination of the providers’ response of “Never” regarding these 2 areas in the post-survey.
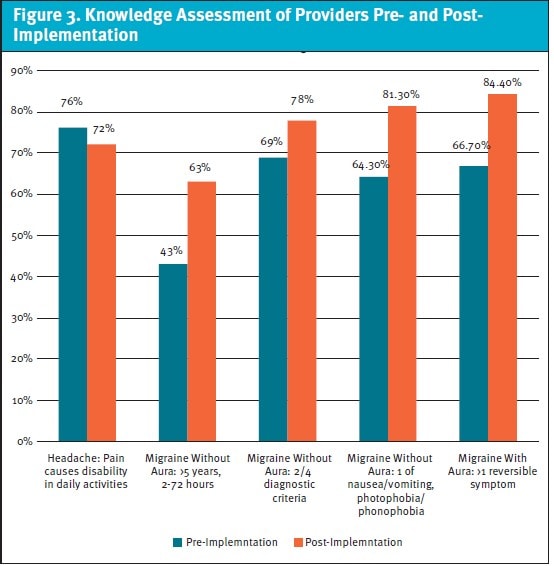
An assessment of clinician knowledge was performed by matching the correct diagnosis with various symptoms/presentations of headache and migraine with and without aura, and statistical significance was assessed using an exact sign test for nominal data. There was an increase in migraine without aura diagnosis post-implementation with an increase from 43% to 63% of clinicians correctly identifying the criteria (eg, more than 5 headaches per year lasting 2-72 hours [p= 0.002]). There was also an increase from 69% to 78% of clinicians correctly identifying 2 of 4 criteria required for diagnosis of headache/migraine (p= 0.001). An increase was noted from 64% to 81% of clinicians identifying the significance of nausea, vomiting, photophobia/phonophobia as diagnostic criteria for migraine (p= 0.002). Clinicians correctly identifying the criteria for diagnosis of migraine with aura increased from 67% to 84%, however, this was not statistically significant (p>0.05). (Figure 3)
Discussion
Accurate diagnosis of the type of headache syndrome and appropriate management in children can present a challenge in the UC setting due to lack of prior patient relationship and time constraints. Prior to this project, it was unclear how much provider knowledge and/or confidence surrounding EBP guidelines for the treatment of pediatric headaches may have affected appropriateness of care for children presenting to our UC centers with acute headaches. We found that this provider group appropriately treated headaches between 36% and 44% of the time, which is far above the national average for guideline adherence of 14%.1 This may be due to the practice environment since the project was conducted in a pediatric specialized network of UC centers. Given this level of clinician performance prior to project implementation, facilitating further improvements presented a challenge. Although the proportion of patient encounters where the treatment was appropriate did not change during the project, clinicians’ level of confidence and knowledge increased during project implementation.
In the post-assessment survey, clinicians who participated showed an improvement in their ability to accurately diagnosis migraine headaches. A greater proportion of clinicians reported confidence and ability to educate families after the project. The finding of an increase in knowledge and confidence among clinicians in evaluation and management of pediatric headaches after the project implementation suggests that the initiative may have influenced patient care and outcomes, although these were not directly assessed in this project.
Limitations
The findings of this project are limited in several ways. Data were extracted over less than a 1-year period. Given high seasonal variation in PUC presentations, it is likely that there was some heterogeneity in headache presentations between the pre- and post-implementation (eg, flu season versus summertime with higher rates of minor trauma). The survey response rate of clinicians was approximately 40%, therefore, we are unable to assess how this project may have influenced the majority of the clinicians who did not participate. It is possible, even likely, that there may be important differences in practice patterns between the clinicians who did and did not participate. As with any survey-based project, it is also uncertain to what extent clinicians reported honestly and engaged fully with the survey questions.
While the project screened over 90,000 patient encounters, the number of encounters meeting inclusion criteria was relatively small, particularly among patients diagnosed with migraine (n<50 for both periods). Additionally, given the retrospective nature of the project, chart inclusion capture was limited to patients given an encounter diagnosis of headache and/or migraine, not exclusive of overlap of additional illnesses or diagnoses. These entries can be recorded by clinical staff as a symptom and not a diagnosis, which can lead to erroneously included cases. Conversely, cases where headache and/or migraine may have been treated without updating the final diagnosis in the encounter would not have been included.
The study only looked at clinic-administered medications when assessing EBP guideline concordant care. Home medications are often given prior to arrival and, therefore, would not have been captured by our chart review methodology. Patients may also present with complaints of a headache or migraine that had since resolved and have a pain score of zero at the time of assessment. Such presentations would also not necessitate intervention on the part of clinician, but they would appear as not EBP guideline concordant care based on the project’s methodology. Finally, this was conducted in a pediatric-specialized UC center, and it is unclear to what extent the findings may be generalizable to non-specialized UC practice settings.
Conclusion
Education and dispersion of an EBP headache and migraine pathway in our pediatric UC centers facilitated access to society guidelines for the diagnosis and management of children presenting with acute headaches. Clinicians’ confidence and knowledge regarding appropriate care for pediatric headaches improved after implementing the interventions of this quality project as did familiarity with diagnosis criteria and appropriate management. The pathway we developed to support this quality improvement was well received by clinicians, and the pathway has been permanently added to our organization’s clinical references.
The authors would like to thank Mary Cazzell, PhD, RN, of Cook Children’s Medical Center for her tremendous assistance, support, and guidance throughout this project.
Manuscript submitted December 31, 2023, accepted August 28, 2024.
Author Affiliations: Sarah J. Nembu, DPN, APRN, FNP-C, CPNP-AC, Cook Children’s Provider Network. Melissa R. Penkalski, DNP, APRN, CPNP-PC, AE-C, Missouri State University.
- [1]. Patniyot IR, Gelfand AA. Acute treatment therapies for pediatric migraine: A qualitative systematic review. Headache: The Journal of Head & Face Pain, 2016;56(1):49-70. doi: https://doi.org/10.1111/head.12746
- [2]. Yamanaka G, Morichi S, Suzuki S, et al. A review on the triggers of pediatric migraine with the aim of improving headache education. J Clin Medicine, 2020;9(11):3717. https://www.doi.org/10.3390/jcm9113717
- [3]. Oskoui M, Pringsheim T, Holler-Managan Y, et al. Practice guideline update summary: Acute treatment of migraine in children and adolescents. Neurology, 2019;93(11): 487-499. https://doi.org/10.1212/WNL.0000000000008095
- [4. American Academy of Pediatrics. Acute treatment of migraine in children and adolescents: Statement of endorsement. Pediatrics, 2019; 144(5). https://doi.org/10.1542/peds.2019-2762
- [5]. American Academy of Neurology. Practice guideline update: Acute treatment of migraine in children and adolescents. 2019; Accessed April 7, 2023. https://www.aan.com/Guidelines/home/GetGuidelineContent/971.
- [6]. Minen MT, Zhou K, Miller L. A brief look at urgent care visits for migraine: The care received and ideas to guide migraine care in this proliferating medical setting. Headache, 2019;60(3): 542-552. https://doi.org/10.1111/head.13717
- [7]. Kang BS, Lee J, Choi JH, Kwon JW, Kang JW. Clinical manifestations of headache in children younger than 7 years. Korean Journal of Pediatrics, 2018;61(11): 355-361. https://doi.org/10.3345/kjp.2018.06331
- [8]. Klein J, Koch T. Headache in Children. Pediatrics in Review, 2020;41(4):159-171.
- [9]. Rossi R, Versace A, Lauria B, et al. Headache in the pediatric emergency department: A 5-year retrospective study. Cephalalgia, 2018;38(11):1765-1772. https://doi.org/10.1177/0333102417748907
- [10]. Marseglia GL, Alessio M, Da Dalt L, Giuliano M, Ravelli A, Marchisio P. Acute pain management in children: a survey of Italian pediatricians. Italian Journal of Pediatrics, 2019;45(1):1–12. https://doi.org/10.1186/s13052-019-0754-3
- [11]. Petrelli T, Farrokhyar F, McGrathP, et al. The use of ibuprofen and acetaminophen for acute headache in the postconcussive youth: A pilot study. Paediatrics & Child Health, 2017;22(1):2–6. https://doi.org/10.1093/pch/pxw011
- [12]. Thomas L, Strauss LD. Pediatric migraine treatment options and further evaluation. First Contact Headache In Primary Care: American Headache Society. 2021; Accessed April 7, 2023. https://americanheadachesociety.org/wp-content/uploads/2021/03/AHS-First-Contact-Pediatric-Migraine-Write-Up.pdf
- [13]. Sheridan DC, Dhatt S, Narayan K, Lin A, Fu R., Meckler GD. Effectiveness of emergency department treatment of pediatric headache in relation to rebound headache. Pediatric Emergency Care, 2020;36(12):720-725. https://doi.org/10.1097/pec.0000000000002027
- [14]. Affaitati G, Martelletti P, Lopopolo M, et al. Use of nonsteroidal anti-inflammatory drugs for symptomatic treatment of episodic headache. Pain Practice: The Official Journal of World Institute of Pain, 2017;17(3):392–401.
- [15]. Seng EK, Gelfand AA, Nicholson RA. Assessing evidence-based medicine and opioid/barbiturate as first-line acute treatment of pediatric migraine and primary headache: A retrospective observational study of health systems data. Cephalgia, 2019;29(8):1000-1009. https://doi.org/10.1177/0333102419833080
- [16]. Troy E, Yonker M. ED and inpatient management of headaches in children and adolescents. Curr Neurol Neurosci Rep., 2020;20:15-5. doi: https://doi.org/10.1007/s11910-020-01035-5
- [17]. Talai A, Heilbrunn B. Ondansetron for acute migraine treatment in the pediatric emergency department. Pediatric Neurology, 2020;103:52-56.
Download the article PDF: Develop and Implementation of a Headache and Migraine Pathway in Pediatric Urgent Care
