Urgent Message: Acute coronary syndromes (ACS), including ST-elevation myocardial infarction (STEMI), may present with predominant back pain or other non-chest-pain symptoms. Additionally, electrocardiogram findings in cases of coronary occlusion may not always meet STEMI criteria. It is important to include myocardial ischemia and ACS in the differential for back pain presentations, especially when the pain is not reproducible.
Sarah Mannon OMS-3; Lauren Schuermann OMS-3; Michael B. Weinstock, MD
Citation: Mannon S, Schuermann L, Weinstock M. Escalating Back Pain Leading to a Diagnosis of ST-Elevation Myocardial Infarction (STEMI) in Urgent Care: A Case Report. J Urgent Care Med. 2024; 18 (9): 50-54
Key Words: ST-elevation myocardial infarction, occlusive myocardial infarction, back pain, case report
Abstract
Introduction: ST-elevation myocardial infarction (STEMI) is a highly time sensitive diagnosis and can present with an array of symptoms. Patients with back pain may present to the urgent care (UC) for diagnosis and management without an understanding among clinicians that acute coronary syndrome (ACS) is in the differential.
Clinical Presentation: A 66-year-old man presented to the UC with complaints of increasing back pain over the previous month. Notably, the pain was worse with exertion and relieved with rest.
Physical Exam: The patient was alert and oriented. Lungs were clear with equal breath sounds, and regular heart rate and rhythm. Abdomen was soft and nontender without a pulsatile abdominal mass. Extremities had no pain or swelling. On palpation, mild cervical (C4-C7) trapezius and lumbar (L1-L4) paraspinal tenderness were noted bilaterally. Tenderness was not reproduced with range of motion.
Case Resolution: An electrocardiogram (ECG) was performed that revealed a STEMI and the patient was transported to the local emergency department (ED) where percutaneous coronary intervention (PCI) was successful in opening the culprit vessel.
Conclusion: Patients may present in UC settings with ACS, including STEMI, but may not have typical symptoms such as chest pain. Neck or back pain that is worse with exertion should clue clinicians into the possibility of myocardial ischemia as a potential etiology.
Introduction
ACS defines a group of disorders, including unstable angina, non-ST elevation myocardial infarction (NSTEMI), and STEMI, involving acute ischemia due to coronary arterial obstruction.1 A STEMI occurs when acute occlusion of 1 or more coronary arteries is sufficient to cause transmural myocardial ischemia, resulting in myocardia necrosis if unaddressed.2 STEMI is defined as ACS with characteristic electrocardiogram (ECG) changes of ST-elevations in more than one contiguous leads or new bundle branch block with ischemic repolarization patterns.2 The most suggestive symptoms of ACS include chest pain (especially with radiation), dyspnea, diaphoresis, and vomiting.3 However, previous studies have found that upper back pain and fatigue are also commonly reported symptoms related to ACS.4 Up to 30% of patients do not present with or experience chest pain.4,5 The objective of this case report is to shed light on an unusual presentation of STEMI to ensure that clinicians include this diagnosis in their differential.
Clinical Presentation
A 66-year-old male presented to the UC via private vehicle with a chief complaint of increased upper back and neck pain. His past medical history was significant for chronic back pain, basilar skull fracture, and prior lumbar spinal fracture. The patient did not take any daily medications. The patient was a smoker but denied alcohol or illicit drug use and lived at home with his wife.
The patient had acute on chronic neck and back pain for the last 4-6 weeks. He stated that it started with back discomfort every few days and had now progressed to severe back pain at least every day for 20-30 minutes. The patient’s pain was not reproducible by any specific range of motion and there was no mechanism for musculoskeletal strain. For a few days prior to presentation, his back pain had been accompanied by cyclical bilateral upper extremity numbness. He reported rest as a relieving symptom. Over the last few weeks, he had been seen multiple times by a chiropractor who had made musculoskeletal adjustments with no relief. His wife and daughter were present for the encounter and the wife stated on the morning of the presentation he appeared uncomfortable and unable to walk around due to back pain, which lasted 20-30 minutes. At the time of the encounter, the patient denied chest pain, difficulty breathing, abdominal pain, nausea, vomiting, trauma, and bowel or urinary incontinence.
Physical Exam
- Blood pressure: 131/94
- Pulse: 91
- Temperature: 36.4oC
- Respiration: 12
- SpO2: 100%
On the physical exam, the patient was in no acute distress resting on the gurney. Normal cardiac and lung sounds were present on auscultation. Abdomen was soft and nontender without pulsatile abdominal mass. Cranial nerves II-XII were grossly intact with DTR +2, no sensory deficits, and motor strength 5/5 in flexion and extension of forearm. On palpation, mild cervical (C4-C7) trapezius and lumbar (L1-L4) paraspinal tenderness were noted bilaterally. Tenderness was not reproduced with range of motion. Extremities did not reveal any pain or swelling.
Problem List and Differential Diagnosis
The patient’s problem list included exertional upper back pain, fatigue, and bilateral arm numbness. A differential diagnosis for such a presentation includes musculoskeletal etiologies including spinal disc pathology with radiculopathy or myelopathy, thoracic aortic dissection, abdominal aortic aneurysm, pathologic rib or spinal fracture, pulmonary embolism, pneumothorax, and ACS, among other etiologies.
Case Continuation and Timeline
After initially evaluating the patient, the UC clinician ordered an ECG in consideration of cardiac etiologies and a chest x-ray (CXR) considering the possibilities of pneumothorax, pneumonia, cardiomyogenic cause, and aortic dissection. The CXR did not show any concerning abnormality, but the ECG revealed ST elevations in the anterior leads concerning for STEMI in the context of his symptoms (Figure 1). The patient was given 325 mg of aspirin and transferred to the emergency department (ED) by ambulance.
Diagnostic Assessment and Case Conclusion: ED Course In the ED, a repeat ECG on arrival revealed continued ST elevation in leads I and V2-V5 as well as T-wave inversion in aVL (reciprocal change). His initial troponin was significantly elevated at 3.04 ng/mL. He emergently underwent percutaneous coronary intervention with placement of 2 drug-eluting stents in the left anterior descending coronary artery with no complications and was discharged after an uneventful hospital stay.
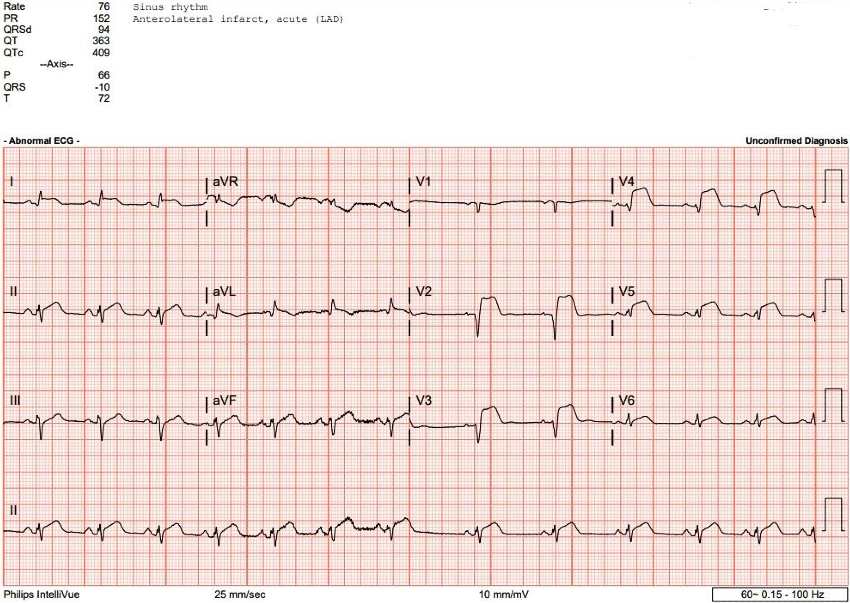
ECG shows abnormal findings including anterior ST elevation (arrows) and reciprocal changes in lead aVL
Discussion
STEMI is a common, life-threatening occurrence in the United States with approximately 750,00 cases diagnosed annually.6,7 Despite the symptoms most suggestive of STEMI being chest pain with radiation, dyspnea, diaphoresis, and vomiting, many patients present without these most specific features.3,8 A retrospective study of 721 cases of ACS showed that 53% of patients presented with chest pain, 17% with shortness of breath, 7% with cardiac arrest, 4% with dizziness/weakness/syncope, 2% with abdominal pain, and 17% with another presentation.9 In this group of patients, those at highest risk for an alternate set of symptoms, were those over 84 years old.9
Another study conducted on hospitalized patients with ACS showed that women were more likely to present without chest pain and had higher mortality rates within the same age group.10 The sex differences in clinical presentation without chest pain and mortality were shown to increase with increasing age.10
Certain cardiology experts have highlighted problems with current nomenclature for various forms of ACS, including STEMI and NSTEMI, and have suggested that a more clinically relevant means of classification would be to divide ACS based on the pathophysiological nature of the event rather than ECG patterns.11
For example, a recent study by Meyer et al reviewed 467 patients with “high risk” ACS presentations. Of the patients included, 108 had occlusion myocardial infarction (OMI) on angiography. Among patients with OMI on angiography, 40% of the ECGs did not demonstrate ST-segment elevation, underscoring the peril in relying on electrocardiographic criteria alone. This also suggests that a large portion of OMI patients will not receive appropriate emergent revascularization.12 Recent studies have shown that up to 25% of patients diagnosed with NSTEMI have had an acute coronary occlusion.13, 14 ST-depression or hyperacute T-waves can be early ECG changes suggesting impending OMI.15 Prudent practice for UC clinicians, therefore, would be to refer any patients with exertional pain symptoms or other concerning symptoms for ACS and new or dynamic ST-segment ECG changes to a PCI-capable ED immediately.
The American College of Cardiology and American Heart Association guidelines for the management of acute myocardial infarction have established the gold standard of door-to-balloon time of 90 minutes for primary PCI.16 Aspirin therapy is also a cornerstone in the immediate treatment of STEMI. A study completed by the Second International Study of Infarct Survival demonstrated that 162.5 mg aspirin given immediately with or without fibrinolytic therapy for STEMI reduced 5-week vascular mortality by 23%.17,18 Therefore, it is important for UC clinicians to be aware of the timely actions that are necessary in insuring patients with concerning presentations for OMI be managed and transferred to an ED where definitive care is possible. Patients with ischemic symptoms should always be urgently transported to the ED by 911 emergency medical service (EMS) along with stabilizing care such as oxygen and automated external defibrillator pads. A study showed that more than 1 in 20 patients with STEMI present prehospital with sudden cardiac arrest after EMS arrival, and another study showed that 1 in 300 patients not transported by EMS with just possible ischemic symptoms suffered cardiac arrest en route.19,20
Ethics Statement
Informed consent for publication of this case was not able to be obtained as the patient did not return any communication. The details and demographics of the case have been altered slightly to protect the patient’s privacy.
Takeaway Points for Urgent Care Clinicians
- Elderly patients and female patients are more likely to present with atypical symptoms of ACS.
- Patients experiencing ACS can present with a wide variety of symptoms beyond chest pain, including dyspnea, cardiac arrest, dizziness/weakness/syncope, abdominal pain, neck pain, and back pain.
- Exertional symptoms including pain, nausea, dyspnea, and fatigue, should prompt an ECG.
- Patients can have acute coronary occlusion or OMI, commonly without ECG findings that meet criteria for STEMI. Therefore, any concerning new or dynamic ST-segment changes on ECG should prompt immediate ED referral.
Manuscript submitted March 10, 2024; accepted June 4, 2024.
References
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. PMID: 25260718 pubmed.ncbi.nlm.nih.gov/25260718/
- Stengaard C, Sørensen JT, Rasmussen MB, Bøtker MT, Pedersen CK, Terkelsen CJ. Prehospital diagnosis of patients with acute myocardial infarction. Diagn Berl Ger. 2016;3(4):155-166. doi:10.1515/dx-2016-0021
- Lu L, Liu M, Sun R, Zheng Y, Zhang P. Myocardial Infarction: Symptoms and Treatments. Cell Biochem Biophys. 2015;72(3):865-867. doi:10.1007/s12013-015-0553-4
- DeVon HA, Mirzaei S, Zègre‐Hemsey J. Typical and Atypical Symptoms of Acute Coronary Syndrome: Time to Retire the Terms? J Am Heart Assoc. 2020;9(7):e015539. doi:10.1161/JAHA.119.015539
- DeVon HA, Burke LA, Vuckovic KM, et al. Symptoms Suggestive of Acute Coronary Syndrome: When Is Sex Important? J Cardiovasc Nurs. 2017;32(4):383. doi:10.1097/JCN.0000000000000351
- Abe T, Olanipekun T, Adedinsewo D, et al. Trends and Outcomes of ST‐Segment–Elevation Myocardial Infarction Among Young Women in the United States. J Am Heart Assoc. 2023;12(5):e026811. doi:10.1161/JAHA.122.026811
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics—2016 Update. Circulation. 2016;133(4):e38-e360. doi:10.1161/CIR.0000000000000350
- 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department. doi:10.1016/j.jacc.2022.08.750
- Gupta M, Tabas JA, Kohn MA. Presenting complaint among patients with myocardial infarction who present to an urban, public hospital emergency department. Ann Emerg Med. 2002;40(2):180-186. doi:10.1067/mem.2002.126396
- Canto JG, Rogers WJ, Goldberg RJ, et al. Association of Age and Sex With Myocardial Infarction Symptom Presentation and In-Hospital Mortality. JAMA. 2012;307(8):813-822. doi:10.1001/jama.2012.199
- Sankardas MA, Ramakumar V, Farooqui FA. Of Occlusions, Inclusions, and Exclusions: Time to Reclassify Infarctions? Circulation. 2021;144(5):333-335. doi:10.1161/CIRCULATIONAHA.121.055827
- Meyers HP, Bracey A, Lee D, et al. Comparison of the ST-Elevation Myocardial Infarction (STEMI) vs. NSTEMI and Occlusion MI (OMI) vs. NOMI Paradigms of Acute MI. J Emerg Med. 2021;60(3):273-284. doi:10.1016/j.jemermed.2020.10.026
- Koyama Y, Hansen PS, Hanratty CG, Nelson GIC, Rasmussen HH. Prevalence of coronary occlusion and outcome of an immediate invasive strategy in suspected acute myocardial infarction with and without ST-segment elevation. Am J Cardiol. 2002;90(6):579-584. doi:10.1016/s0002-9149(02)02559-6
- Khan AR, Golwala H, Tripathi A, et al. Impact of total occlusion of culprit artery in acute non-ST elevation myocardial infarction: a systematic review and meta-analysis. Eur Heart J. 2017;38(41):3082-3089. doi:10.1093/eurheartj/ehx418
- Smith SW, Meyers HP. Hyperacute T-waves Can Be a Useful Sign of Occlusion Myocardial Infarction if Appropriately Defined. Ann Emerg Med. 2023;82(2):203-206. doi:10.1016/j.annemergmed.2023.01.011
- Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004;44(3):E1-E211. doi:10.1016/j.jacc.2004.07.014
- Initial Aspirin Dose and Outcome Among ST-Elevation Myocardial Infarction Patients Treated With Fibrinolytic Therapy. Circulation. December 17, 2007. Accessed May 24, 2024. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.729558
- Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet Lond Engl. 1988;2(8607):349-360.
- Karam N, Bataille S, Marijon E, et al. Incidence, Mortality, and Outcome-Predictors of Sudden Cardiac Arrest Complicating Myocardial Infarction Prior to Hospital Admission. Circ Cardiovasc Interv. 2019;12(1):e007081. doi:10.1161/CIRCINTERVENTIONS.118.007081
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2013 Dec 24;128(25):e481]. Circulation. 2013;127(4):e362-e425. doi:10.1161/CIR.0b013e3182742cf6
Download the article PDF: Escalating Back Pain Leading to a Diagnosis of ST-Elevation Myocardial Infarction (STEMI) in Urgent Care: A Case Report

