Urgent message: Creating and cultivating cohesive, goal-oriented, and patient-focused urgent care teams starts with visible front-line leaders who emphasize a strong service culture, open communication, personal accountability, and management transparency.
ALAN A. AYERS, MBA, MAcc Practice Velocity
Introduction
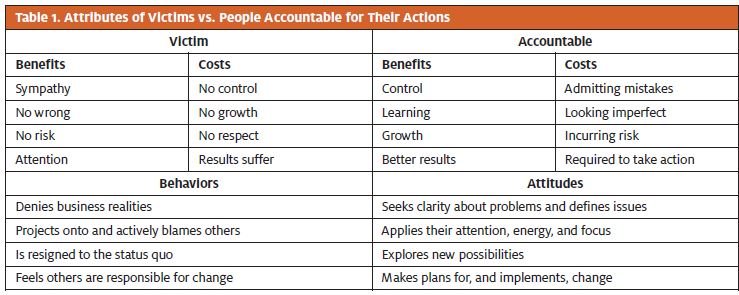
The stress, resentment, and dissatisfaction that one experiences being part of a disconnected and ineffective team are not easily forgotten. Common sense may lead one to believe that the safest path is to ignore the team’s dysfunction and consider it just a part of the job. After all, suggesting that there is room for improvement would just make things worse, and besides, would anyone listen? Over time, team members who realize they cannot influence the direction of the organization start to identify as victims. But this attitude of resignation only makes things worse, especially for the patients for whom the team is responsible. Table 1 shows the behaviors, attitudes, benefits, and costs associated with being a victim as opposed to being accountable.
Playing the Role of Victim Has Benefits
The role of victim can be played with little or no effort. Victims never risk anything, they never do any wrong, and best of all, they get a lot of attention and sympathy without ever working for it. The eternal problem with victims is their effortless contributions to a team’s ineffectiveness. Without the desire to have any control whatsoever over their circumstances, victims will not be held accountable for their own actions, because someone else is always to blame. With these defense mechanisms in place, an organization of victims has no chance for the kind of growth that occurs by learning from one’s mistakes. Instead, a victim’s mastery of denial and projection protects them from acknowledging the weaknesses and failures at the root of the team’s ineffectiveness. Table 2 lists can versus can’t attitudes—victims embrace the can’t, whereas the accountable seek out the can.
| Table 2. Sample of Can Versus Can’t Attitudes |
| Can’t Attitudes (I Can’t!) |
| We’ve never done it before It’s too complicated It will never work There is not enough time We already tried it It’s a waste of time We don’t have the experience They’ll take care of it It’s good enough They’re a bottleneck It’ll never fly We don’t have enough training It’s not going to be any better It can’t be done No one communicates Isn’t it time to go home I don’t have any idea Let someone else deal with it We’re always changing direction I never receive feedback It’s too radical a change It takes too long for approval They won’t buy it It’s not my job |
| Can Attitudes (I Can!) |
| We have the opportunity to be first Let’s look at it from a different angle Let’s give it a try We will reevaluate some priorities We learned from the experience Think of the possibilities Let’s network with those who do I’d like to follow it through with you There is always room for improvement I’ll get them involved earlier We’ll never know if we don’t try I’ll teach myself or ask for a mentor We’ll try it one more time It will be a challenge Let’s open the channels Days go so quickly around here I’ll come up with some alternative I’m ready to learn something new We’re in touch with our customers I’ll ask my manager for feedback Let’s take a chance We’ll walk through the system We’ll do a better job educating them I’ll be glad to take the responsibility |
Accountable Teams Start with Commitment to a Goal
Effective teams seldom occur spontaneously. Rather, creation of a successful and effective team involves a great deal of work, planning, and a strong sense of commitment from each team member. Effective teamwork occurs when team members are working together toward the same clearly identified goal. In the case of urgent care, this goal should entail serving patients in a courteous, professional, and efficient manner. Team members should be respectful of each other’s opinions and suggestions, and everyone should understand the value of giving due consideration to the ideas that arise from each other’s life experiences. A team that puts forth a unified effort to reach common goals is compensated with a more satisfying work experience and greater productivity.
With this thought in mind, it’s important to understand that conflicts can erupt even in the most cohesive teams whose members usually work together in relative peace and harmony. An effective team leader prepares for the inevitable skirmish in advance by having a structured conflict-resolution plan in place. Once a conflict is satisfactorily resolved, team members should take advantage of the learning and growth opportunity gained by looking at a problem from a different perspective. This idea of conflict being advantageous in certain situations embraces the concept of cognitive diversity in relation to the effectiveness of a team. Teams consist of people with different talents, levels of ability, and knowledge. If all team members think about the same problem in the same way, it is extremely difficult to come up with a new or inventive approach to resolve problems. Thus, having differing experiences and perspectives will add flavor to the mix of ideas. When a problem is identified and placed in the “I can’t” column under the category of “We’ve never done that before,” members of an effective team will see the chance to use their “I can” attitude and say, “We have the opportunity to be first.”
An effective team is flexible, making every effort to adapt to new circumstances. Members are confident their team leader or manager supports them in the same way as their teammates. A manager must provide leadership for the group, but an effective leader should know just how much or how little management is necessary to inspire maximum productivity from the team. The effective leader recognizes the need for clearly defined tasks and responsibilities but also knows that strict adherence to pigeon-holed job descriptions limits employees’ ability to reach their full potential. Team members are willing to take on responsibilities beyond their job descriptions, often see that as a learning opportunity. On the best teams, all members feel accountable for their actions in their own jobs and share a sense of ownership in achieving overall goals.
Effective Leaders Encourage Open Communication
Open communication is a vital characteristic of an effective team. Employees believe that their leader is approachable, values their ideas, and listens to their input. In turn, successful leaders show appreciation for team members and give frequent feedback in acknowledgment of their efforts and achievements. Communication between team members is necessary, and interactions are frequent in a successful team. Data and information about the practice’s strategies, tactical plans, and real-time performance are readily shared. The most effective teams are willing to approach problems in new ways, and they are open to considering the innovative or out-of-the box solutions offered by their teammates.
Although there is no one-size-fits-all approach to the creation of an effective team, the following attributes are offered as general guidelines. A plan to cultivate these attributes should be made only after careful consideration of all known factors that contribute to the unique circumstances of the team, as well as consideration of the individual members’ strengths.
Attribute 1: A Strong Service Culture
An effective team will create and sustain a strong service culture. More specifically this involves focusing on capturing repeat visits from loyal patients. Urgent care is in the patient satisfaction business, because centers are successful only insofar as patients return for future medical needs and tell others to do likewise. Thus, strength of a center’s relationship with patients can be measured by reach and loyalty. Reach refers to the number unique patients the center serves, and loyalty refers to the proportion of a patient’s total care that is through the facility or health system.1 The first step in creating an effective team entails hiring and training people who can effectively build relationships with patients.
Attribute 2: Managers Lead from the Front, Not the Top Having managers who lead from the front, rather than the top, is another attribute necessary for creating a successful and effective team. In many cases this can be accomplished by the leader’s first taking on the toughest tasks to show that they can be done.2 Many real leaders3 do not believe in asking their team to do anything they themselves would not do. It’s one thing to tell people what to do, but it is an entirely different thing for the leader to actually show or demonstrate what needs to be accomplished. Managers at all levels should understand all systems and processes in the center. Such familiarity demonstrates to team members that all jobs contribute to the overall goal and that the appropriate response to facing a problem is to jump in and devise a solution. Leading by example builds teams of individuals who can function independently when the need arises.
Active management entails changing the outcome of business situations before the end of the day. Much like a snowball rolling down a hill, issues can grow out of proportion when left unchecked. Leading from the front, an effective manager will not allow a situation to grow so large that it becomes unmanageable. Rather, the manager will intervene at the first signs something is amiss.
Some leaders monitor and share key performance metrics via a dashboard or scorecard approach.4 To be effective, each team member must understand the numbers that drive the business. Using graphic illustrations to show how a team is performing relative to its goals, the leader and team members can understand what is currently happening within the business and intervene early when issues appear, to make sure that day-to-day operations stay on track.
Attribute 3: Culture of Transparency
Building an effective medical team requires creation of a culture of transparency. Transparency can be defined as “a lack of hidden agendas or conditions, accompanied by the availability of full information required for collaboration, cooperation, and collective decision making.”5 A transparent culture can help team members feel safe discussing problems affecting patient care, such as HIPAA (Health Insurance Portability and Accountability Act) guidelines, malpractice risks, payor and Medicare compliance, patient safety, and clinical quality guidelines. Rather than hide or ignore problems within the practice, committed team members engage incident-reporting processes early and take part in devising solutions. They realize that there will be no retaliation for sincerely raising issues that could affect patient safety and quality of care. Rather, they understand the dire risks to patients and the practice of ignoring or hiding problems.
Attribute 4: Culture of Accountability
A culture of accountability that starts at the top is the final attribute necessary for building an effective medical team. Health-care providers have used performance management systems and quality-improvement methods in an attempt to improve the quality and outcomes of health-care services, but they had little success until there was a change in organizational culture to complement the tools and processes used to improve quality.6
If an organization wishes to continuously learn and use evidence-based practices, it must create a sense of accountability within employees. Instead of shifting from one flavor of the month to the next, accountability ensures the permanence of performance management and continuous improvement by holding people to their commitments on a daily basis.6
To create a culture of accountability, it is important to reinforce that not only will the quality of patient care improve but also the quality of work will improve organization-wide. If employees associate the development of a culture of accountability with being reprimanded, it is unlikely that they will accept the new direction. Instead, what is required is a complete and total focus on emphasizing that this change will improve health-care quality and employee satisfaction.
Accountability is very similar to stewardship in health administration because it demonstrates responsibility to the patient population that the organization serves. As with stewardship, accountability aims to ensure careful and responsible management of human, physical, and financial resources. A culture of accountability contains a set of common elements wherein6
- The common belief is continuous learning and improvement at the individual, unit or department, and organizational levels
- Decisions regarding care and direction are guided by evidence-based protocols and clinical practice guidelines but not by individual preference
- Performance measurement is an essential element in assessing outcomes and guiding improvement initiatives
- Reporting errors is encouraged and is not punished
- There is collaboration and coordination among and between all levels of the organization and across all specialties.
It would be a mistake to think that leadership is primarily an administrative function because in a healthcare setting, most protocols are a combination of both administrative and clinical processes. The implication of this is that in addition to a chief executive officer, the change process must involve a team of leaders and individual managers to help inspire change across business and clinical functions. As an example of accountability beginning at the top, a physician champion must help to motivate others in order to gain physician buy-in.6
The ultimate goal of creating a culture of accountability is to create a continuously learning organization, which promotes the acquisition and use of new knowledge as a strategy for coping with change and also recognizes the critical need to empower workforces to learn and participate in continuous improvement.
Conclusion
Effective teams do not evolve by chance. In urgent care, they start with a strong emphasis on serving patients, are driven by leaders who engage the front line in a common goal, and function in a framework of transparency and accountability. With the 20/20 vision that hindsight gives, a wise person chooses to learn from the dysfunctional team-member experience and seeks ways to build more effective teams moving forward. They might even apply the knowledge they gained in those difficult times when confronted with a “can’t” attitude of “It’ll never fly” and change it to “We’ll never know if we don’t try.” Although a positive attitude alone will not accomplish a task, it makes the rest of the job much easier.
References
- Kasinadhuni M. What’s better: 4,000 new patients or 1,000 repeat customers? The Advisory Board Company [website]. Washington DC: The Advisory Board Company. © 2014 [cited 2016 September 13]. Available from: https://www.advisory.com/Research/Market-Innovation-Center/the-growth-channel/2014/12/patient-share-one-time-customers-orrepeat-patients
- Cammuta T. Leading the way or leadership from behind? About Leaders. © 2013 April 24 [cited 2016 September 13]. Available from: http://aboutleaders.com/leading-the-wayor-leadership-from behind/#gs.IrwfkzA
- Jackson T. Leadership: the discipline of doing [blog post]. About Leaders. © 2013 April 10 [cited 2016 September 13]. Available from: http://aboutleaders.com/leadership-thediscipline-of-doing/#gs.V5AAxNc
- Wise L. A closer look at scorecards and dashboards. Dashboard Insight. © 2010 [cited 2016 September 13]. Accessed from: http://www.dashboardinsight.com/articles/digitaldashboards/ fundamentals/a-closer-look-at-scorecards-and-dashboards.aspx
- Transparency [word definition]. BusinessDictionary.com. [Cited 2016 September 13.] Washington DC: WebFinance, Inc. Available from: http://www.businessdictionary.com/definition/transparency.html
- O’Hagan J, Persaud D. Creating a culture of accountability in health care. Health Care Manager. 2009;28:124–133. Available from: http://www.nursingcenter.com/static? pageid=935642