Urgent message: Antibiotic resistance is a worldwide problem with a local solution—one that starts in your urgent care center. Focusing on responsible prescribing, in combination with staff and patient education, will start to curb overprescribing. Every appropriate prescription you write and every inappropriate prescription you opt not to write is a step in the right direction.
By 1980, scientists believed that roughly 3%-5% of Streptococcus pneumoniae were penicillin-resistant and by the turn of the century, approximately 34% of S pneumoniae were testing resistant to penicillin. Similar studies of other antibiotics and their corresponding bacteria have shown to follow an analogous resistance pattern.1 In the last 20 years, antibiotic resistance in bacteria strains such as Staphylococcus aureus, tuberculosis, and Clostridium difficile has become an increasingly concerning topic in the medical community.
Given its dramatic growth over the latter part of that period, urgent care is well positioned to both treat patients in need of antibiotics and to guard against further resistance.
Health Organization Threat List
The World Health Organization (WHO), in collaboration with the Centers for Disease Control and Prevention (CDC), has declared antibiotic resistance to be a growing global threat. As such, these organizations have increased their surveillance of mutating stains of pathogens and released a list of potentially dangerous antibiotic resistant infections.
The CDC has categorized certain drug-resistant strains as Urgent Threats, Serious Threats, and Concerning Threats. Health providers and urgent care centers should keep up to date on releases of new information regarding antibiotic resistance and ensure proper handling of patients with a potential infection of an antibiotic-resistant pathogen. Please refer to Tables 1, 2, and 3 for definitions of threat levels, diseases, and symptoms to look for.
| Table 1: Urgent Threats | ||
| Definition: Determined that the threat of infection has significant risk factors to potentially become a widespread contagion, and that active steps must be taken to limit transmission.2 | ||
| Disease | Symptoms | Risk Factors |
| Clostridium difficile (C diff) | Life-threatening diarrhea | Recent medical care and use of antibiotics |
| Carbapenem-resistant Enterobacteriaceae (CRE) | This threat includes species such as E coli and Klebsiella. Look for common symptoms of these infections such as diarrhea, fever, nausea, and redness, swelling and/or pain at a specific site. | Recent hospital stay, patients on ventilators, have catheters or long-term antibiotic usage |
| Neisseria gonorrhoeae | Mucus-like discharge from entail area, burning/painful urinations, painful swollen glands in throat (oral sex), or painful swollen testicles | Sexual active without use of a condom, multiple partners |
| Table 2: Serious Threats | ||
| Definition: Determined that the threat of infection is lowered due to many factors; however, will potentially continue to worsen; needs vigilant surveillance to prevent transmission2 | ||
| Disease | Symptoms | Risk Factors |
| Multidrug-resistant Acinetobacter | Pneumonia, wound infections, fever chill and cough. Typically seen as a nosocomial infection. Can lead to bacteremia, meningitis and UTIs | Recent surgery or hospital stay. Weakened immune systems, chronic lung disease and diabetes |
| Drug-resistant Campylobacter | Bloody stool/diarrhea, fever, abdominal cramps | Weakened immune system |
| Fluconazole-resistant Candida | Symptoms vary due to location—general itching, redness, swelling | Hospital stays, recent surgery |
| Extended-spectrum Enterobacteriaceae (ESBL) | Abdominal pain, diarrhea, fever and chills | Elderly, sick and recent hospital stay |
| Vancomycin-resistant Enterococcus (VRE) | UTI, sepsis, pelvic infection and endocarditis | Hospital stays, recent surgery, weakened immune system |
| Multidrug-resistant Pseudomonas aeruginosa | Sepsis, skin rash, and pneumonia | Weakened immune systems, individuals on a breathing apparatus |
| Drug-resistant non-typhoidal Salmonella | Nausea, vomiting, fever, diarrhea and abdominal pain | Handling/eating uncooked food and poor hygiene |
| Drug-resistant Salmonella serotype typhi | Fever, rash, dry cough and diarrhea. Severe symptoms include severe exhaustion, hallucinations and delirium | Contaminated food/water source |
| Drug-resistant Shigella | Fever, bloody stools/diarrhea, and abdominal pain | Young children and poor hygiene |
| Methicillin-resistant Staphylococcus aureus (MRSA) | Pneumonia, wound infection, sepsis | Recent hospitalization, recent surgery, catheter insertion, ventilation, and previous antibiotic use |
| Drug-resistant Streptococcus pneumoniae | Pneumonia, meningitis, and acute otitis media | Child care center visits, recent pneumonia with use of antibiotics |
| Drug-resistant tuberculosis | Weakness, weight loss fever and night sweats. May be accompanied by coughing, chest pain and coughing blood | Patients who have been put on a TB drug regimen, but not adhered to medication dosages |
| Table 3: Concerning Threats | ||
| Definition: The following bacteria are considered low level threats due to low incidence of antibiotic resistance, yet can still cause severe illness2 | ||
| Disease | Symptoms | Risk Factors |
| Vancomycin-resistant Staphylococcus aureus (VRSA) | Swelling, soreness, fever, chills, weakness and persistent cough | Recent surgery, catheterization or ventilation |
| Erythromycin-resistant Streptococcus Group A | Myositis, toxic shock, fever, sore throat, chills and ache | Residents of nursing homes, or underlying medical conditions |
| Erythromycin-resistant Streptococcus Group A | Infection of wounds, sepsis, meningitis and pneumonia | Pregnant women, elderly, underlying medical conditions |
Impact on Urgent Care Facilities
Weinick, et al estimate that 13.7% to 27.1% of all emergency department visits could be adequately handled at an urgent care facility.3 Given that there are approximately 7,100 urgent cares within the United States (with those numbers rising annually), seeing an average of 16,328 patients annually,4 urgent care centers are accessible enough to present an opportunity to improve availability of high-quality, lower cost healthcare unseen in previous decades.
Now consider that the Centers for Disease Control and Prevention estimates 33% of antibiotic prescriptions are unnecessary.5 The spread of “superbugs” such as MRSA and colistin-resistant E coli is rapidly becoming a major problem in the healthcare fields. Nosocomial outbreaks of these strains in healthcare facilities put many lives at risk and can lead to serious complications such as organ failure, sepsis, and death. While research is crucial to producing ways to eliminate these strains, the first line of defense lies at the point of care, vis-à-vis greatly reducing the volume of antibiotic prescriptions given to patients.
Ways Urgent Cares Can Mitigate Antibiotic Resistance
Providing educational resources for the staff of your facility, as well as your incoming patients, is the best way to reduce the pressure to prescribe antibiotics. There are many ways to provide education to staff and patients; basic guidelines are listed below:
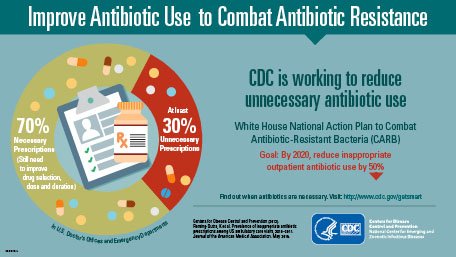
- Health fliers to disclose the risk of antibiotic resistance: The CDC provides several easy-to-read bulletins and fliers which can be distributed to patients and displayed within the office (Figures 1 and 2).
Figure 1.
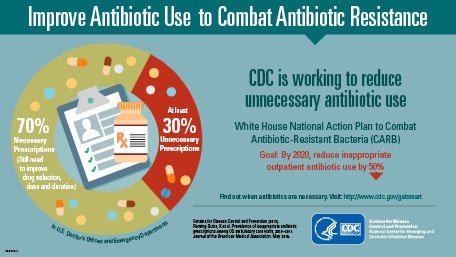
Figure 2.
- Taking time to explain the difference between viral and bacterial infections: Many patients do not understand the difference between viral infections and bacterial infections. Providers and staff taking the time to talk to the patients about the differences and the basic foundations of how antibiotics work can bridge the knowledge gap and reassure patients about your recommended treatment. Provide take-home packets that provide basic antibiotic guidelines.
- Urge patients to complete the full course of antibiotic treatment (not stopping once they feel better) and to follow CDC Antibiotics Usage Guidelines.
- Conduct workshops for employees to teach and update staff on current antibiotic resistance trends and risk factors to look for: Provide frequent staff workshops to provide education on the current CDC and WHO guidelines for antibiotic resistance. Discuss ways to talk to patients about antibiotic usage and importance of following these guidelines. Your staff will be your first line of defense in providing patients with outstanding care and practical postcare instructions.
Visit the Antibiotic Resistance Lab Network
The CDC launched the Antibiotic Resistance Lab Network to provide national coordination among state labs to detect and combat antibiotic resistance. This network is to be utilized as support in case of suspected antibiotics resistant outbreaks within your urgent care facility. Providers should assess the prescription of antibiotics on a facility-wide and case-by-case basis to determine which patients truly need an antibiotic prescription. Education of both staff and patients can deter the unnecessary prescription of antibiotics and reduce the potential of antibiotic resistance. Urgent care managers should review and conduct regular informational meetings and provide fact sheets for employees to assist in patient care when antibiotics are unnecessary. Each facility should provide informational material to patients, on the suggested treatment plan and the reasoning for or against the prescription of antibiotics. Urgent care centers and their providers are at the forefront of efforts to mitigate antibiotic resistance, and are crucial in the prevention and containment of widespread antibiotic resistant strains.
References
- Falagas ME, Kasiakou SK. Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections.Clin Infect Dis. 2006;40(9):1333-1341.
- Centers for Disease Control and Prevention. Antibiotic/Antimicrobial Resistance. Biggest threats. Available at: https://www.cdc.gov/drugresistance/biggest_threats.html. Accessed September 13, 2016.
- Weinick RM, Burns RM, Mehrotra A. How many emergency department visits could be managed at urgent care centers and retail clinics?Health Aff (Millwood). 2010;29(9):1630-1636.
- Urgent Care Association. 2010 Urgent Care Benchmarking Survey Results: Visits. February 2011. Available at: www.ucaoa.org.
- Centers for Disease Control and Prevention. CDC: 1 in 3 antibiotic prescriptions unnecessary. CDC Newsroom. May 3, 2016. Available at: http://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html. Accessed September 12, 2016.
Charis Royal, Researcher, University of Arizona College of Medicine – Phoenix
