Differential Diagnosis
- Right bundle branch block (RBBB)
- ST-elevation myocardial infarction (STEMI)
- Brugada syndrome
- Hypokalemia
- Tricyclic antidepressant toxicity
Diagnosis
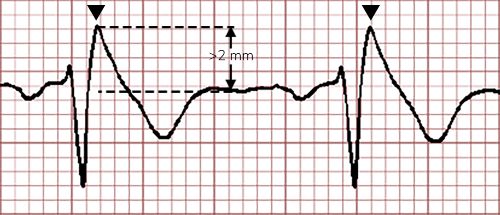
The correct diagnosis in this case is Brugada syndrome. The ECG reveals a normal sinus rhythm at a rate of 78 beats per minute, normal axis. The right-sided precordial leads (V1 and V2) have an rSR’ appearance and a coved ST segment with > 2 mm elevation followed by an inverted T wave.
Discussion
First described in 1992 under the original name of “right bundle branch block, persistent ST segment elevation and sudden death,”1 Brugada syndrome is a sodium channelopathy that can easily be misdiagnosed as a benign RBBB given the RSR’ appearance in V1 and V2. However, upon closer inspection, the ST segments have a peculiar, coved appearance with a J point/ST-segment elevation > 2 mm, not seen in RBBB. Additionally, the QRS complex is narrow (<120 msec), excluding RBBB. While there is ST-elevation in 2 contiguous leads, the absence of reciprocal ST-segment depressions in anatomically opposing leads (in this case, inferior leads II, III, and aVF) as well as the clinical context should prompt the clinician to consider alternative diagnoses. These findings describe a Type 1 Brugada pattern, which is now recognized as the only type to establish the diagnosis whether seen spontaneously or provoked by drug challenge (usually class I antiarrhythmics/Na+ blockade drugs).2,3
The ECG changes can be spontaneous or transiently provoked by fever or drugs3 and should prompt transfer to an electrophysiology-capable center, especially in the context of syncope.
One interesting presentation for Brugada is nocturnal agonal respirations. Sudden death after these frightening gasps have been reported in Southeast Asia, where it was previously described as sudden unexplained nocturnal death syndrome (SUNDS). This phenomenon was previously known in the Philippines as bangungut —“to rise and moan in sleep;” in Japan as pokkuri—“sudden and unexpectedly ceased phenomena;” and in Thailand as Lai Tai—“death during sleep.”4 This unique presentation of syncope, as in this case, should prompt consideration of Brugada syndrome.
Regarding the other diagnoses listed in the differential, hypokalemia is known to cause a prolonged repolarization phase, leading to a long QT interval, U waves, or a wavy appearance of the repolarization phase secondary to T-U fusion. A tricyclic antidepressant overdose is known to cause findings of sodium channel toxicity including QRS widening, a right axis deviation, and a tall terminal R in aVR. Neither of these diagnoses are consistent with the findings in this ECG.
What to Look For
- The type 1, or coved-type Brugada pattern consists of an rSR’ appearance in V1 and V2 combined with down-sloping ST-segment elevation (>2mm) followed by a negative T wave.
- When seen in the context of syncope, nocturnal agonal respirations, or a family history of sudden cardiac death, the diagnosis of Brugada syndrome is suggested and the patient is at risk for fatal ventricular dysrhythmias.
Pearls for Initial Management, Considerations For Transfer:
- The Brugada Pattern found on routine ECG in an asymptomatic patient does not necessarily warrant transfer, but a discussion for follow up with a cardiologist is prudent.
- If symptomatic, especially with syncope or abnormal breathing pattern, transfer to the emergency department with pacer pads in place.
References
- Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20(6):1391-1396. doi:10.1016/0735-1097(92)90253-J
- Sieira J, Brugada P. The definition of the Brugada syndrome. Eur Heart J. 2017;38(40):3029-3034. doi:10.1093/eurheartj/ehx490
- Marsman EMJ, Postema PG, Remme CA. Brugada syndrome: update and future perspectives. Heart. 2022;108(9):668-675. doi:10.1136/HEARTJNL-2020-318258
- Antzelevitch C, Brugada P, Brugada J, Brugada R, Towbin JA, Nademanee K. Brugada syndrome: 1992-2002: A historical perspective. J Am Coll Cardiol. 2003;41(10):1665-1671. doi:10.1016/S0735-1097(03)00310-3

