Differential Diagnosis
- Wellens syndrome
- Hypokalemia
- Subarachnoid hemorrhage
- Persistent juvenile T-wave pattern
- Hypertrophic cardiomyopathy
Diagnosis
The diagnosis is hypertrophic cardiomyopathy. The ECG reveals sinus bradycardia with a rate of 54 beats per minute. There are impressive, symmetric T-wave inversions in the anterior precordial leads V1 through V4 and large QRS complexes in V1 through V3.
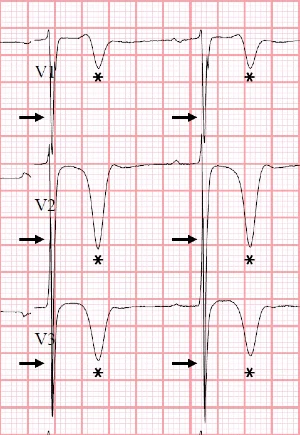
Hypertrophic cardiomyopathy (HCM) is the most common cause of sudden cardiac death in individuals under 40 years of age. Its prevalence is reported to range from 1:200 to 1:500.1 HCM can have a variable electrocardiographic appearance and it’s not uncommon to see repolarization abnormalities like the ones seen here (Figure 2).Common ECG findings include large QRS complexes of left ventricular hypertrophy, T wave inversions (especially in lateral leads), and narrow, “dagger” Q waves in the lateral leads (I, aVL, V5, V6).2,3 Symmetric T-wave inversions in the precordial leads is suggestive of apical HCM, although this patient had septal hypertrophy (Figure 3). Physical exam may show the classic finding of a harsh crescendo-decrescendo mid-systolic murmur best heard at the lower left sternal border, which becomes louder when ventricular volume is low (ie, with Valsalva maneuver or going from squatting to standing).
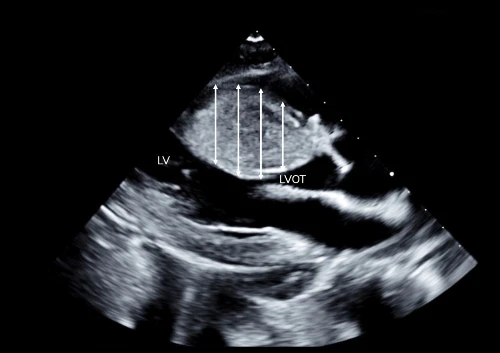
Hypertrophic cardiomyopathy is characterized predominantly by left ventricular hypertrophy in the absence of another explanatory cardiac, systemic, or metabolic disease state. Nearly any pattern of wall thickening can be present, with the anteroseptal most affected.2 Disease severity depends upon the exact location of the thickening, the amount of the thickening, and the degree of obstruction to left ventricular outflow that the thickening causes.
The most reported symptoms are related to left ventricular outflow obstruction and include dyspnea, fatigue, and exercise intolerance. Patients with hypertrophic cardiomyopathy are poorly tolerant of faster heart rates like those experience with atrial fibrillation, and, in the most severe cases, HCM can present with ventricular tachycardia or ventricular fibrillation leading to sudden cardiac death. For that reason, recommendations for exercise should be made carefully in conjunction with a cardiologist trained in the management of HCM. The application of contemporary cardiovascular therapies and interventions (eg, implantable cardiac defibrillators) has lowered hypertrophic cardiomyopathy mortality rates to <1.0%/year.2
If ECG findings suggestive of hypertrophic cardiomyopathy are incidentally discovered, outpatient follow-up is appropriate. However, if syncope or other symptoms suggesting a possible life-threatening dysrhythmia are present (ie, episodic palpitations, presyncope, etc.), transfer to a higher level of care is warranted. For this patient, the safest disposition is to transfer to a facility capable of cardiac imaging and cardiology consultation.
What to Look For
- Consider HCM in young patients presenting with exertional syncope
- ECG findings of HCM include large QRS complexes of left ventricular hypertrophy, T wave inversions, and narrow, “dagger” Q waves in the lateral leads
Pearls for Initial Management, Considerations for Transfer
- Patients with possible hypertrophic cardiomyopathy and syncope should be transferred to a cardiac-capable facility, as definitive treatment may consist of an implantable cardiac defibrillator, or surgical ablation/myectomy
- Limit tachycardia to allow left ventricular filling. Beta blockers or non-dihydropyridine calcium channel blockers may be warranted while arranging transfer.
References
- Semsarian C, Ingles J, Maron MS, Maron BJ. New perspectives on the prevalence of hypertrophic cardiomyopathy. J Am Coll Cardiol. 2015;65(12):1249-1254. doi:10.1016/J.JACC.2015.01.019
- Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2020;76(25):e159-e240. doi:10.1016/J.JACC.2020.08.045
- Wagner GS, Strauss DG. Marriott’s Practical Electrocardiography. 12th ed. Lippincott Williams & Wilkins; 2014.
Click Here to download the article PDF.

