Published on
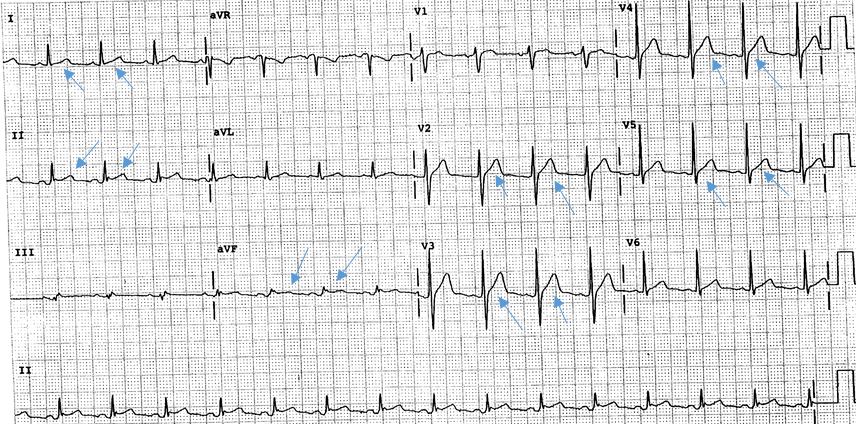
- Inferior STEMI
- Acute pericarditis
- Anterior STEMI
- Sinus bradycardia
- Ventricular tachycardia
Diagnosis
The ECG shows diffuse ST elevation secondary to acute pericarditis (answer B). Post ECG, the patient confirms he had a viral upper respiratory infection 2 weeks ago, with resolution of URI symptoms within the last few days.
Learnings
- ST elevation may be caused by an acute ischemia/infarction, but other causes include:
- Ventricular aneurysm
- Early repolarization
- Prinzmetal’s angina
- Pericarditis (diffuse ST segment elevation)
- How can ST elevation from acute pericarditis be differentiated from a STEMI? The answer is, the STEMI generally occurs from occlusion of a coronary artery (plaque rupture à platelet aggregation à coronary artery occlusion). STEMI will generally occur in an anatomic distribution, and not a generalized For example:
- Occlusion of the right coronary artery (RCA) will usually result in inferior ischemia, seen as ST elevation in the inferior leads (II, III, and aVF) and will often have reciprocal change
- Occlusion of the left anterior descending artery (LAD) will results in anterior ischemia see as ST elevation in the anterior leads V3 and V4
- Occlusion of the circumflex artery will result in lateral ischemia seen as ST elevation in the lateral leads I, aVL, V5 and V6
- Key point: with acute pericarditis, the ST elevation is generalized and does NOT follow an anatomic distribution
- Etiologies of acute pericarditis include:
- Idiopathic
- Infectious—usually viral, but may include bacterial or even tuberculosis
- Inflammatory—consider lupus, rheumatoid arthritis
- Other—drugs, radiation, sarcoidosis, trauma
- The classical exam finding is a cardiac “rub,” a rough-type rubbing/scratching sound, though (as in our patient), this is not always present
- ECHO may be performed to look for pericardial effusion/tamponade
- Management is with NSAIDS
Pearls for Initial Management and Considerations for Transfer
- Unstable vital signs
- Diagnostic uncertainty
- Inability to follow up or return with worsening symptoms
- Inability to definitively exclude STEMI/ACS
A 37-Year-Old Man with a Two-Day History of Chest Pain
1 2