Published on
Differential Diagnosis
- Atrioventricular nodal reentrant tachycardia
- Sinus tachycardia
- Atrial tachycardia
- Atrial flutter
Diagnosis
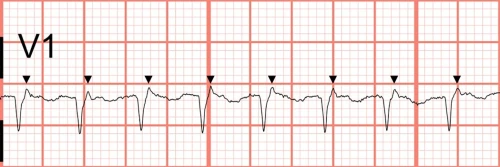
The diagnosis in this case is atrioventricular nodal reentrant tachycardia. The rate is tachycardic at 200 beats per minute with a narrow QRS and a regular rhythm. P waves cannot be clearly delineated; however, retrograde P’ waves can be seen immediately following the QRS complexes in V1, where they create a pseudo-R appearance (Figure 2).
Discussion
The differential for narrow complex regular tachycardia includes sinus tachycardia, atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia, atrial flutter, and atrial tachycardia. P waves can aid the diagnosis but are often obscured by the preceding P waves at faster rates. If P waves are present in a sawtooth pattern (especially in the inferior leads), atrial flutter is likely (2:1 conduction usually has a ventricular response rate around 150). AVNRT is a micro-reentrant circuit within the atrioventricular node that typically has a rate between 140 and 220 beats per minute. While most cases of AVNRT do not have visible P waves, up to one-third of AVNRT cases will have retrograde P’ waves immediately following the QRS complex, giving the appearance of a “pseudo-S wave” in the inferior limb leads, or a “pseudo-R wave” in V1 (Figure 1).1–3 The presence of tachycardia beyond the maximum expected heart rate (220 minus the age), and lack of R-R variation also favor AVNRT.
Treatment of AVNRT includes atrioventricular nodal blocking agents (eg, adenosine, diltiazem, metoprolol, amiodarone) or maneuvers to increase vagal tone.3 Vagal maneuvers are techniques to increase the parasympathetic tone and can be helpful for treating certain arrythmias; examples include the Valsalva maneuver, carotid massage, and gagging or vomiting. The modified Valsalva technique includes a passive leg raise after the Valsalva strain and is reported to be nearly 50% effective.4 While cardioversion is recommended for unstable patients, this equipment is rarely available in Urgent Care, so 911 activation is indicated. Having an automated external defibrillator (AED) near the patient while awaiting ambulance transport is appropriate, however, applying the pads is not indicated unless the patient loses consciousness. This patient’s rhythm converted to sinus after administration of adenosine.
Atrioventricular reentrant tachycardia involves an accessory pathway, the stigmata of which can be seen on the resting ECG (ie, delta wave and shortened PR interval). Atrial tachycardia involves an ectopic focus that delivers impulses typically at a rate of 150 to 250 beats per minute.5 With atrial tachycardia, the P wave axis will be abnormal (usually down in aVR and up in lead II indicating non-sinus activity).
What to Look For
- AVNRT is narrow, fast, and regular
- Rates typically exceed the maximum expected heart rate (220 minus the age)
- One-third of cases will have retrograde P’ waves immediately following the QRS complexes in V1 or lead II
Pearls for Initial Management, Considerations for Transfer
- When AVNRT is suspected, attempt bedside vagal maneuvers first
- If vagal maneuvers are unsuccessful, medications can be attempted if available; otherwise, transfer to a capable facility
- If unstable, immediate electrical cardioversion is indicated
References
- Katritsis DG, Camm AJ. Atrioventricular nodal reentrant tachycardia. Circulation. 2010;122(8):831-840. doi:10.1161/CIRCULATIONAHA.110.936591
- Whinnett ZI, Sohaib SMA, Davies DW. Diagnosis and management of supraventricular tachycardia. Bmj. 2012;345(dec11 1):e7769-e7769. doi:10.1136/bmj.e7769
- Link MS. Evaluation and Initial Treatment of Supraventricular Tachycardia. New England Journal of Medicine. 2012;367(15):1438-1448. doi:10.1056/NEJMcp1111259
- Appelboam A, Reuben A, Mann C, et al. Postural modifi cation to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias ( REVERT ): a randomized controlled trial. :1747-1753. doi:10.1016/S0140-6736(15)61485-4
- Mattu A, Tabas J, Brady W. Electrocardiography in Emergency, Acute, and Critical Care. 2nd ed. The American College of Emergency Physicians; 2019.

