Differential Diagnosis
- Puncture wound
- Retained organic material foreign body
- Contusion
- Abscess
- Cellulitis
- Osteomyelitis
- Plantar fasciitis
Diagnosis
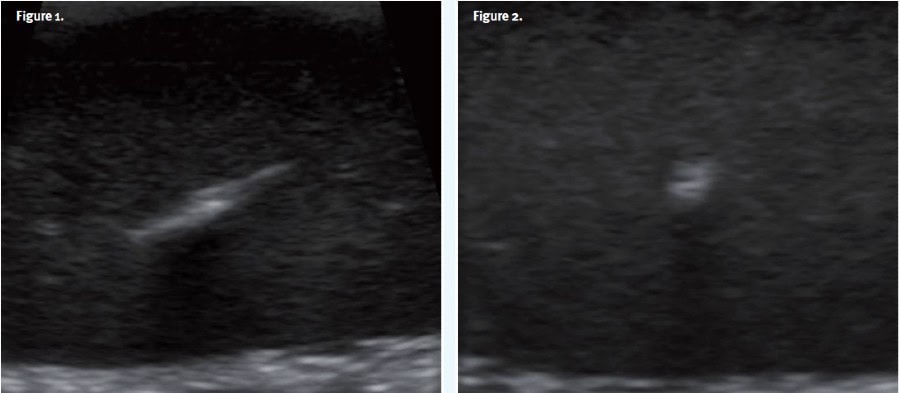
The correct diagnosis in this case is a retained wooden splinter in the plantar soft tissues. While the physical exam and XR are non-diagnostic, the POCUS exam reveals a hyperechoic (white) structure in the plantar soft tissues with posterior shadowing (black), consistent with a wooden foreign body; this was confirmed after removal in urgent care. The shape of the object is linear, as evidenced by the punctate appearance in one plane and linear appearance in the other. A slight surrounding hypoechoic (light gray) halo was also observed, indicative of inflammatory changes. No fluid collection was identified, indicating that no abscess was present.
Discussion
Retained wooden splinters are commonly missed on initial evaluation due to their radiolucency and nonspecific associated symptoms. XR has limited sensitivity for detecting radiolucent foreign bodies (eg, wood and plastic) with sensitivities reported as low as 5-20%.1-3 Ultrasound offers a significant advantage in identifying radiolucent materials, with sensitivities ranging from 78-100% for wood.1-4 On ultrasound, wooden foreign bodies appear as hyperechoic structures with posterior acoustic shadowing. A hypoechoic halo is seen when the foreign body has been retained for over 24 hours, indicating inflammation.5 Visualization in multiple planes can help determine the shape of the object. The water bath technique can improve visualization of small foreign bodies in small or superficial structures, such as digits and hands.6
Additional advantages of POCUS for evaluating soft tissues for retained foreign bodies include its ability to assess for associated abscess formation, and the function of Color Mode to identify superficial vasculature structures. Furthermore, POCUS can provide real-time guidance during the foreign body extraction process, which can enhance precision and reduce the risk of discomfort and complications.
Despite its utility, POCUS does have limitations: Sensitivity will be reduced in the hands of inexperienced operators; acoustic artifacts such as gas shadows from infections or overlying tissues can obscure visualization; and differentiation between foreign bodies and other hyperechoic structures, like calcifications, may be challenging. Despite these limitations, when used in conjunction with clinical context and proper technique, ultrasound can be a valuable tool for assisting in identification and removal of soft tissue foreign bodies.
What to Look For
- Retained foreign bodies often present with localized pain, swelling, and erythema. A visible puncture wound may not always be present.
- On ultrasound, wooden foreign bodies appear as hyperechoic structures with posterior acoustic shadowing.
- Look for an associated anechoic (black) fluid collection which may represent an abscess.
- Measure the size and depth of the foreign body to guide removal.
Pearls for Urgent Care Management
- Employ POCUS to detect radiolucent foreign bodies. Familiarity with sonographic characteristics of various foreign body materials can enhance diagnostic accuracy.
- Promptly remove foreign bodies once identified (under ultrasound guidance when feasible) to prevent complications such as deep space infection/osteomyelitis, granuloma formation, and chronic pain.
- Ensure tetanus vaccination status is up-to-date and consider antibiotics when signs of infection are present.
- Urgent referral to a podiatrist is indicated for cases with deep (eg, embedded near tendons, joints, or neurovascular structures) or complex foreign bodies (eg, irregularly shaped or multiple fragments) , failed removal attempts, or in high-risk patients and those with severe pain/functional impairment.
References:
- Grocutt, H. et al. Ultrasound compared with projection radiography for the detection of soft tissue foreign bodies – A technical note. Radiography, Volume 29, Issue 6, 1007 – 1010
- American College of Emergency Physicians (ACEP). Sonoguide: Foreign Body Localization. ACEP Emergency Ultrasound Section. Updated 2023. Available at: https://www.acep.org/sonoguide/procedures/foreign-bodies/. Accessed November 28, 2024.
- Turkcuer I, Atilla R, Topacoglu H, Yanturali S, Kiyan S, Kabakci N, Bozkurt S, Cevik AA. Do we really need plain and soft-tissue radiographies to detect radiolucent foreign bodies in the ED? Am J Emerg Med. 2006 Nov;24(7):763-8.
- Rockett MS, Gentile SC, Gudas CJ, Brage ME, Zygmunt KH. The use of ultrasonography for the detection of retained wooden foreign bodies in the foot. J Foot Ankle Surg. 1995 Sep-Oct;34(5):478-84; discussion 510-1
- Lewis D, Jivraj A, Atkinson P, Jarman R. My patient is injured: identifying foreign bodies with ultrasound. Ultrasound. 2015 Aug;23(3):174-80. doi: 10.1177/1742271X15579950. Epub 2015 Mar 26.
- Shelhoss SC, Burgin CM. Maximizing Foreign Body Detection by Ultrasound With the Water Bath Technique Coupled With the Focal Zone Advantage: A Technical Report. Cureus. 2022 Nov 16;14(11):e31577.
Download the Article PDF: 57-Year-Old with Left Foot Pain
