Differential Diagnosis
- Diffuse subendocardial ischemia
- Left ventricular hypertrophy (LVH)
- ST-elevation myocardial infarction (STEMI)
- Non-ST-elevation myocardial infarction (NSTEMI)
- Wellens syndrome
Diagnosis
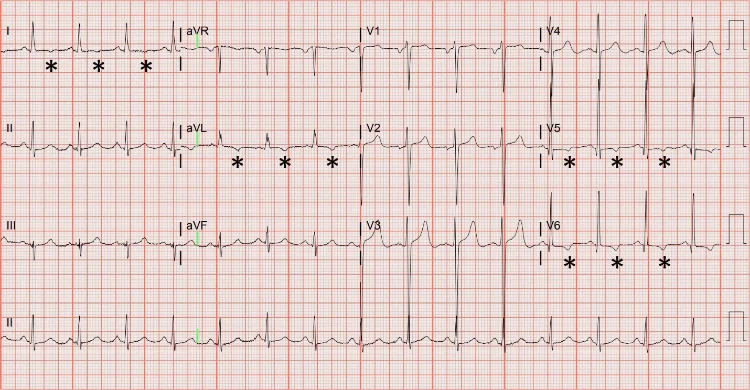
The correct diagnosis in this case is left ventricular hypertrophy. The ECG reveals a sinus rhythm with a rate of 91 beats per minute, large amplitude QRS complexes, and T-wave inversions primarily in the lateral leads (I, aVL, V5, V6). The morphology and distribution of the T-wave inversions are particularly important to note as this distinction can help differentiate chronic, stable changes from acute changes that require more immediate attention.
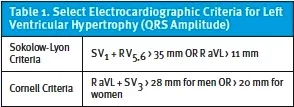
Several electrocardiographic criteria exist for left ventricular hypertrophy, and none of them are particularly sensitive (~50%), but they are quite specific (85-90%).1 Two of the more commonly cited criteria are shown in Table 1.
Repolarization abnormalities are commonly associated with left ventricular hypertrophy, namely asymmetric T-wave inversions and ST-depressions that predominate in the lateral leads—the so-called “strain” pattern, as with this ECG. It is not uncommon to see discordant ST changes associated with LVH, meaning ST changes in the opposite direction as the QRS complex. Notice that ST-depressions are seen in leads with up-going QRS complexes (I, II, aVL, V5, V6), and ST-elevations are seen in leads with down-going QRS complexes (V1, V2, V3). While multilead ST-depression and aVR ST-elevation has been described as a pattern strongly associated with left main or triple vessel disease (i.e. diffuse subendocardial ischemia), it is also commonly seen with LVH.2
T-wave inversions can also indicate acute ischemia, but the T-wave inversions of acute ischemia tend to be symmetric. When deep and symmetric T-waves are seen in the anterior precordial leads while the patient is chest-pain free, it may indicate critical stenosis of the left anterior descending artery—Wellens syndrome.3,4
Although there are ST-elevations in V1 through V3, they do not represent STEMI. ST-elevations associated with STEMI are often straight or convex upward in appearance (ie, “tombstone” morphology). If the patient were having an acute myocardial infarction, a more acute presentation would be expected, as opposed to 1 month of progressive dyspnea. Most importantly, comparison to a prior ECG is quite helpful, if available. This patient was transferred to an emergency department and ultimately diagnosed with severe aortic stenosis.
What to Look For
- Electrocardiographic findings of LVH include large-amplitude QRS complexes.
- LVH can have associated repolarizations abnormalities including ST-depressions and asymmetric T-wave inversions in the lateral leads (I, aVL, V5, V6).
- Compare to prior ECGs when available.
Pearls For Initial Management, Considerations For Transfer
- If the patient is acutely symptomatic with either chest pain, shortness of breath, or with unstable vital signs (ie, hypoxia) then immediate referral to the emergency department is indicated.
- If ECG reveals classic LVH findings but is not acutely symptomatic, the patient likely needs their blood pressure controlled as hypertension is the most likely culprit; however, acute control is not necessary.
References
- Wagner GS, Macfarlane P, Wellens H, et al. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram. Part V: Electrocardiogram Changes Associated With Cardiac Chamber Hypertrophy. Circulation. 2009;53(11):1003-1011. doi:10.1016/j.jacc.2008.12.016
- Knotts RJ, Wilson JM, Kim E, Huang HD, Birnbaum Y. Diffuse ST depression with ST elevation in aVR: Is this pattern specific for global ischemia due to left main coronary artery disease? J Electrocardiol. 2013;46(3):240-248. doi:10.1016/j.jelectrocard.2012.12.016
- Zwaan D, Biir FWHM, Wellens HJJ. Characteristic electrocardiogric pattern indicating a critical stenosis high in left anteior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4):730-736.
- Kontos MC, de Lemos JA, Deitelzweig SB, et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80(20):1925-1960. doi:10.1016/J.JACC.2022.08.750
Download the article PDF for 57-Year-Old With Progressive Dyspnea: JUCM May 2024: Clinical Challenges

