Published on
Differential Diagnosis
- Ventricular tachycardia
- Supraventricular tachycardia with aberrancy
- Antidromic atrioventricular reentrant tachycardia
- Sodium channel toxicity
- Hyperkalemia
Diagnosis
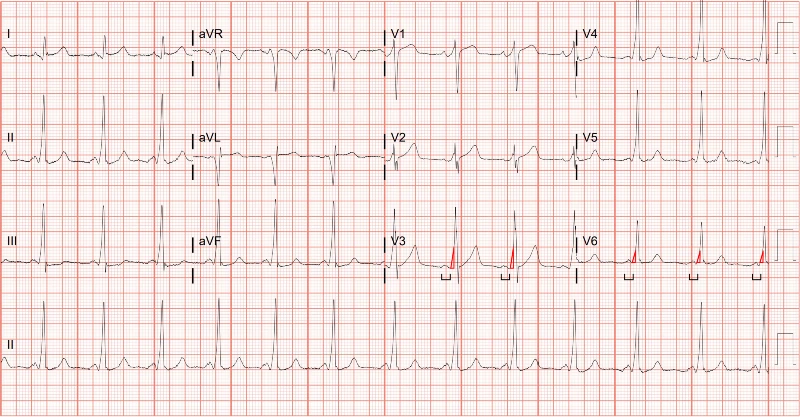
The diagnosis in this case is antidromic atrioventricular reentrant tachycardia (AVRT). The ECG reveals a fast rate of 156 beats per minute, with P waves difficult to appreciate. There is a left axis deviation and a wide QRS complex. Appreciable ST segment changes are difficult to see with this fast rate.
The differential for regular wide complex tachycardia includes:
- Ventricular tachycardia
- Supraventricular tachycardia with aberrancy
- Antidromic atrioventricular reentrant tachycardia
- Toxicologic/metabolic disturbances.1
Eighty percent of wide complex tachycardia is ventricular tachycardia. Several algorithms have been developed to differentiate ventricular tachycardia from other causes of wide complex tachycardia; however, their use in the clinical setting has shown low reproducibility, and it is safest to presume ventricular tachycardia in the absence of compelling information to suggest otherwise.2–6
The wide complex tachycardia in Figure 1 looks like ventricular tachycardia and should be treated as such. This patient was transferred to an emergency department, where the patient was electrically cardioverted. The post conversion ECG demonstrated ventricular pre-excitation evidenced by the short PR interval and slurred upstroke (ie, delta wave, Figure 2). The arrhythmia was confirmed to be antidromic AVRT. Figure 2 shows a sinus rhythm with delta waves seen near the onset of the QRS complexes. The patient’s symptoms improved, and he was admitted for a cardiac ablation.
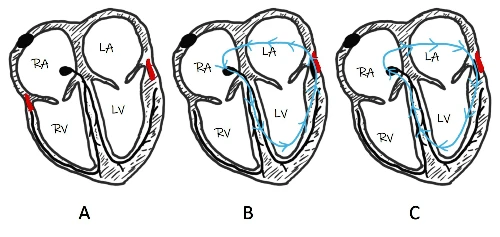
Pre-excitation happens when the ventricle begins to depolarize earlier than normal. This happens when an accessory pathway between the atria and the ventricles (often referred to as the bundle of Kent) conducts a signal to the ventricles slightly before the normal conduction system can.7 When the accessory pathway pre-excites the ventricles, the ECG will show characteristic features: a shortened PR interval and delta waves. When dysrhythmias occur involving the accessory pathway, it is referred to as the Wolf-Parkinson-White syndrome. Antidromic AVRT is a macro reentrant circuit in which the signal travels anterograde through accessory pathway and retrograde through the atrioventricular node (Figure 3). It can be treated with procainamide or electrical cardioversion.
What to Look For
- 80% of wide complex tachycardia is ventricular tachycardia
- Always obtain a post-conversion ECG and look for evidence of pre-excitation
- Pre-excitation on the resting ECG is demonstrated by a short PR interval and a slurred upstroke of the QRS complex (eg, delta wave)
Pearls for Initial Management, Considerations for Transfer
- Treatment options for most cases of wide complex tachycardia include electrical cardioversion and procainamide
- All wide complex tachycardias should be immediately transferred to an emergency department
- Since most regular, wide complex tachycardia is ventricular tachycardia, decompensation into cardiac arrest can happen quickly and unpredictably, so get the automated defibrillator and have it ready and next to the patient while awaiting emergency medical services
References
- Brady WJ, Mattu A, Tabas J, Ferguson JD. The differential diagnosis of wide QRS complex tachycardia. Am J Emerg Med. 2017;35(10):1525-1529. doi:10.1016/J.AJEM.2017.07.056
- zelényi Z, Duray G, Katona G, et al. Comparison of the “real-life” diagnostic value of two recently published electrocardiogram methods for the differential diagnosis of wide QRS complex tachycardias. Academic Emergency Medicine. 2013;20(11):1121-1130. doi:10.1111/acem.12247
- Baxi RP, Hart KW, Vereckei A, et al. Vereckei criteria as a diagnostic tool amongst emergency medicine residents to distinguish between ventricular tachycardia and supra-ventricular tachycardia with aberrancy. J Cardiol. 2012;59(3):307-312. doi:10.1016/j.jjcc.2011.11.007
- Kaiser E, Darrieux FCC, Barbosa SA, et al. Differential diagnosis of wide QRS tachycardias: comparison of two electrocardiographic algorithms. Europace. 2015;17(9):1422-1427. doi:10.1093/EUROPACE/EUU354
- Herbert ME, Votey SR, Morgan MT, Cameron P, Dziukas L. Failure to agree on the electrocardiographic diagnosis of ventricular tachycardia. Ann Emerg Med. 1996;27(1):35-38. doi:10.1016/S0196-0644(96)70293-7
- Jastrzebski M, Kukla P, Czarnecka D, Kawecka-Jaszcz K. Comparison of five electrocardiographic methods for differentiation of wide QRS-complex tachycardias. Europace. 2012;14(8):1165-1171. doi:10.1093/EUROPACE/EUS015
- Moore EN, Spear JF, Boineau JP. Recent Electrophysiologic Studies on the Wolff-Parkinson-White Syndrome. New England Journal of Medicine. 1973;289(18):956-963. doi:10.1056/nejm197311012891808

Download the Article PDF: 59-Year-Old With History Of Hypertension
