Differential Diagnosis
- Normal sinus rhythm
- First degree atrioventricular block
- Second degree atrioventricular block, Mobitz I (Wenckebach)
- Second degree atrioventricular block, Mobitz II
- Third-degree atrioventricular block
Diagnosis
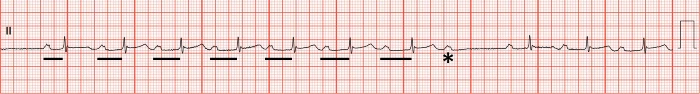
The diagnosis is second-degree atrioventricular block, Mobitz I (Wenckebach). Theventricular rate is 60 beats per minute, and the rhythm is irregular. The PR interval is prolonged and progressively lengthens until a P wave is “dropped,” or fails to conduct to the ventricular system, resulting in the absence of an associated QRS complex. There are 8 P waves for every 7 QRS complexes, representing 8:7 conduction (Figure 2).
Discussion
Atrioventricular conduction block refers to a set of disturbances in which conduction from the atria to the ventricles is delayed, intermittently blocked, or completely blocked—classified as first-, second-, and third-degree, respectively. Identifying the type of block has important prognostic implications. First-degree atrioventricular block, indicated by a prolonged PR interval (greater than 200 msec), usually suggests delayed conduction through the atrioventricular node and is generally considered to be benign when not associated with other conduction deficits.1 Third-degree atrioventricular block occurs when there is complete atrioventricular dissociation (ie, failure of conduction between the atria and the ventricles).2 Patients with third-degree block should be immediately referred to an emergency department (ED).
Second-degree atrioventricular block describes intermittent atrioventricular conduction and can be caused by conduction deficits in the atrioventricular node or distal. There are 2 types of second-degree atrioventricular block: Mobitz I (or Wenckebach conduction), and Mobitz II. Electrocardiographically, Mobitz I conduction is characterized by a progressively prolonging PR interval until conduction from the atria to the ventricle fails, resulting in a “dropped” beat (Figure 2). These blocks are often asymptomatic and can be seen in active, healthy patients without heart disease. It is usually caused by delayed conduction through the atrioventricular node and is unlikely to progress to complete heart block.2 Transfer to the ED is not indicated in patients with Mobitz I conduction when not accompanied by significant bradycardia or other conduction deficits (eg, bundle branch block); however, atrioventricular nodal blocking agents (eg, metoprolol) should be avoided in the setting of Mobitz I conduction.
Second-degree atrioventricular block, Mobitz II is characterized electrocardiographically by a constant PR interval with “dropped” beats that fail to conduct to the ventricular system. Mobitz II is caused by conduction disease distal to the atrioventricular node and is likely to progress to complete heart block. Patients with Mobitz II should be immediately referred to an electrophysiology-capable facility for pacemaker placement.2
What To Look For
- The presence of more P waves than QRS complexes should prompt consideration of atrioventricular block.
- Identifying the type of block has important prognostic implications.
- First-degree and second-degree Mobitz I block generally represent delayed conduction through the atrioventricular node and are not likely to progress to complete heart block.
- Second-degree Mobitz II and third-degree block (ie, complete heart block) indicate conduction disturbance distal to the atrioventricular node.
Pearls For Initial Management And Considerations For Transfer
- Patients second-degree Mobitz II or third-degree block warrant immediate transfer to an electrophysiology-capable facility.
- Patients with first-degree or second-degree Mobitz I block (in the absence of other conduction deficits or significant bradycardia) do not warrant transfer.
- Consider transcutaneous pacing and immediate transfer to an ED in patients with unstable bradycardia secondary to atrioventricular block.
References
- Costa D Da, Brady WJ, Edhouse J. Bradycardias and Atrioventricular conduction block. Br Med J. 2002;324(March):535-538.
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhyth. Circulation. 2019;140(8):e382-e482.\

Read More
- Urgent Care Evaluation Of Arrhythmias
- A 60-Year-Old Woman With Hypertension, Diabetes, And Sudden Fatigue And Weakness
