Differential Diagnosis
- Complete heart block
- Failure-to-sense
- Failure-to-pace
- Failure-to-capture
- Oversensing
Diagnosis
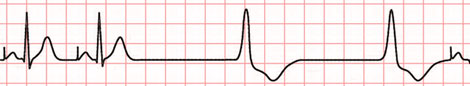
The diagnosis for this patient is failure-to-sense. The ECG reveals sinus tachycardia with a rate of 100 beats per minute. There are several pacemaker spikes occurring within the QRS complexes (vertical green bars), indicating failure-to-sense (Figure 1). This case was caused by a mechanically dislodged pacemaker. The patient was transferred to a capable facility, and the pacemaker was revised.
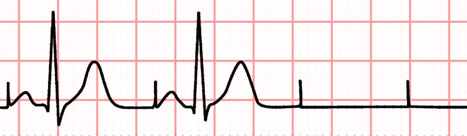
Failure-to-sense occurs when the pacemaker fails to sense native cardiac activity, which leads to asynchronous pacing. Pacing spikes can be seen just after the onset of the QRS complexes (Figure 2). It can be caused by a lead insulation break, new intrinsic bundle branch blocks, electrolyte abnormalities, and Class IC antiarrhythmics.1,2

Failure-to-pace occurs when the paced stimulus is not generated when expected. Pacemaker spikes are decreased or absent (Figure 3). It is usually caused by oversensing but can also be caused by lead fracture or insulation defect. Oversensing occurs when pacemaker activity is inhibited by inappropriately recognized non-cardiac activity (ie, skeletal muscle).1,2 A pacemaker magnet placed over the pacemaker site on the chest wall will enable asynchronous pacing—a mode that paces without sensing—and can be a stabilizing temporary treatment.
Failure-to-capture occurs when the delivery of a pacing stimulus does not lead to myocardial depolarization (Figure 4). This can be caused by mechanical lead displacement or fracture, electrolyte abnormalities, and ischemia or infarction.1,2
Complete heart block occurs when normal conduction between the atria and ventricles is disrupted, leading to atrioventricular dissociation (ie, the atria and ventricles act independently). Since every QRS complex is preceded by a P wave, the rhythm is sinus.
Patients diagnosed with pacemaker malfunctions should be transferred via ambulance to a hospital with an electrophysiologist on call.
What to Look For
Pacemaker malfunctions include failure-to-sense, failure-to-pace, and failure-to-capture. Look for pacemaker spikes in spurious locations. Pacemaker failures can be caused by mechanical lead disruption, electrolyte abnormalities, ischemia, or antiarrhythmics.
Pearls For Initial Management; Considerations For Transfer
- Patients with pacemaker failures should be immediately transferred to a center with an electrophysiologist on call
- A magnet placed on the chest wall over the pacemaker site will enable asynchronous mode and can be a helpful temporizing measure when oversensing occurs
References
- Mulpuru SK, Madhavan M, McLeod CJ, Cha YM, Friedman PA. Cardiac Pacemakers: Function, Troubleshooting, and Management: Part 1 of a 2-Part Series. J Am Coll Cardiol. 2017;69(2):189-210. doi:10.1016/j.jacc.2016.10.061
- Berberian JG, Levine BJ, Brady WJ. EMRA EKG Guide. 1st ed. Emergency Medicine Residents’ Association; 2017.
