Differential Diagnosis
- Complete heart block
- Digoxin toxicity
- Myxedema coma
- Hypothermia
- Beta blocker or calcium channel blocker toxicity
Diagnosis
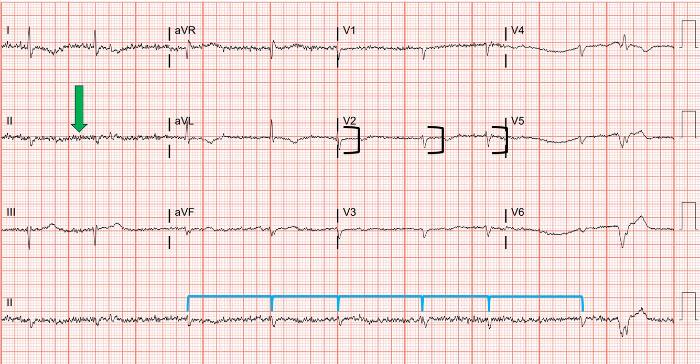
The diagnosis is myxedema coma. The ECG reveals an irregularly irregular bradycardia with a rate of approximately 50 beats per minute and low voltage. Atrial activity shows fine fibrillations without discernible P waves consistent with atrial fibrillation.
Discussion
Atrial fibrillation is a condition where disorganized fibrillatory waves in the atria cause a lack of visible P waves on the surface ECG.1 Only some signals are allowed through the atrioventricular (AV) node, which leads to an irregularly irregular ventricular rhythm (Figure 2). While atrial fibrillation typically involves ventricular rates >100 beats per minute, slow ventricular response describes ventricular rates <60 beats per minute.2 The ECG in this case also has low voltage. Low voltage is defined as QRS amplitudes <5 mm in the limb leads or <10 mm in the precordial leads.3 In this case, the patient had a QRS amplitude of <10 mm in all precordial leads.
When slow atrial fibrillation is encountered, the urgent care provider must consider a broad differential including, but not limited to, the 5 conditions listed above. The pathophysiology commonly involves slowed conduction through the atrioventricular node by a variety of causes, many of which can be ruled out with a comprehensive history and physical examination including medication use. Other conditions, such as hypothyroidism, require additional testing. The combination of low voltage and bradycardia is particularly concerning for hypothyroidism/myxedema.4
Thyroid hormones have multiple cardiac effects at the cellular level, including regulating the amount of beta-1 adrenergic receptors.5 The sum of these effects leads to decreased rate and contractility. Hypothyroidism may also contribute to the presence of atrial fibrillation through the remodeling and fibrosis of the heart and its conduction system, leading to impaired atrial conduction.6
Hypothyroidism can cause low voltage through two mechanisms: the direct effects of hormonal deficiency on the generation of cardiac action potentials and the presence of a pericardial effusion (seen in up to one third of patients with hypothyroidism).4,7 Patients with large effusions due to hypothyroidism will characteristically lack a compensatory tachycardic response, and will be bradycardic or normocardic.8,9
Digoxin toxicity can present with many different ECG manifestations including premature ventricular complexes, ventricular tachycardia, atrial fibrillation, and atrioventricular blocks.1 Digoxin and other medication toxicities (eg, beta blockers or calcium channel blockers) can cause slow atrial fibrillation but are not associated with low amplitude. Complete heart block can occur in the setting of atrial fibrillation, but the rhythm is expected to be regular. Hypothermia can also cause slow atrial fibrillation, but that was also not the case here.
What to Look For
- Slow atrial fibrillation is typically caused by slowed conduction through the atrioventricular node, which can be from a variety of different causes such as medications, ischemia, and myxedema
- Consider all causes of slow atrial fibrillation to avoid missing dangerous diagnoses, including performing a thorough medication reconciliation
Pearls for Initial Management, Considerations for Transfer
- Patients with severe hypothyroidism will require transfer to a higher level of care
- Hemodynamic instability could be caused by cardiac tamponade in patients with hypothyroidism, in which case fluid administration while preparing for immediate transfer is indicated
References
- Stouffer, George A. Practical ECG Interpretation Clues to Heart Disease in Young Adults. Chichester, West Sussex, UK ; Wiley-Blackwell, 2009. Print.
- Ha SH, Jeong S, Park JY, Yang SY, Cha MJ, Cho MS, Chang JY, Kang DW, Kwon SU, Kim BJ. Association Between Slow Ventricular Response and Severe Stroke in Atrial Fibrillation-Related Cardioembolic Stroke. J Stroke. 2023 Sep;25(3):421-424. doi: 10.5853/jos.2023.01753. Epub 2023 Sep 26. PMID: 37813674; PMCID: PMC10574304.
- Madias JE. Low QRS voltage and its causes. J Electrocardiol. 2008;41(6):498-500. doi:10.1016/j.jelectrocard.2008.06.021
- Danzi S, Klein I. Thyroid disease and the cardiovascular system. Endocrinol Metab Clin North Am. 2014;43(2):517-528. doi:10.1016/j.ecl.2014.02.005
- Yamakawa H, Kato TS, Noh JY, Yuasa S, Kawamura A, Fukuda K, Aizawa Y. Thyroid Hormone Plays an Important Role in Cardiac Function: From Bench to Bedside. Front Physiol. 2021 Oct 18;12:606931. doi: 10.3389/fphys.2021.606931. PMID: 34733168; PMCID: PMC8558494.
- Takawale A, Aguilar M, Bouchrit Y, Hiram R. Mechanisms and Management of Thyroid Disease and Atrial Fibrillation: Impact of Atrial Electrical Remodeling and Cardiac Fibrosis. Cells. 2022 Dec 14;11(24):4047. doi: 10.3390/cells11244047. PMID: 36552815; PMCID: PMC9777224.
- Tajiri J, Morita M, Higashi K, Sato T, Fujii H, Nakamura N. The cause of low voltage QRS complex in primary hypothyroidism pericardial effusion or thyroid hormone deficiency? Jpn Heart J. 1985;26(4):539-547. doi:10.1536/ihj.26.539
- Wang JL, Hsieh MJ, Lee CH, et al. Hypothyroid cardiac tamponade: Clinical features, electrocardiography, pericardial fluid and management. American Journal of the Medical Sciences. 2010;340(4):276-281. doi:10.1097/MAJ.0b013e3181e664c6
- Cooper BL, Ducach GJ, Fadial TT. Low and Slow. Ann Emerg Med. 2021;77(6):601-603. doi:10.1016/J.ANNEMERGMED.2020.12.010
- Wei Mak W, Nurazni Raja Azwan R, Badrulnizam Long Bidin M. Severe hypothyroidism presenting with supraventricular tachycardia. Med J Malasia. 2018;73(5):349-350.
Download the Article PDF: 70-Year-Old With Fatigue and Edema

