Published on
Differential Diagnosis
- Ventricular ectopy/pacing/pre-excitation
- Acute/chronic lung disease
- Bifascicular block
- Hyperkalemia
Diagnosis
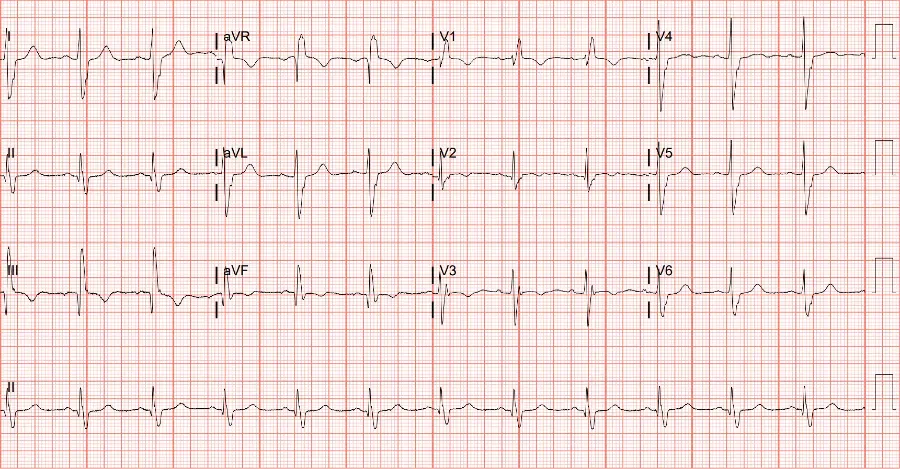
Bifascicular block (right bundle branch block + left posterior fascicular block) is the correct diagnosis in this case. The patient’s ECG shows a normal sinus rhythm with a rate of 72 beats per minute. There is rightward axis deviation (QRS is positive in lead aVF and negative in lead I) with normal PR and QT intervals and a widened QRS (>120msec). There is no evidence of acute ischemia.
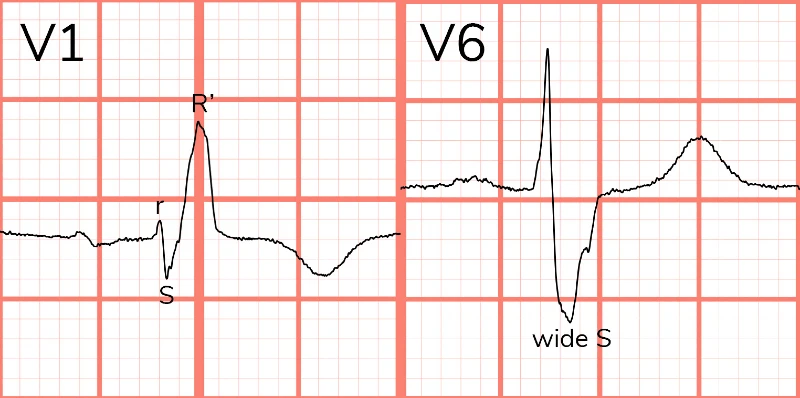
When investigating the etiology of the widened QRS, note the rSR’ in the anterior precordial leads (V1, V2) and deep S-wave in the lateral leads (I, V5, V6). These findings suggest the presence of a right bundle branch block (RBBB) (Figure 2). A RBBB, however, is not expected to alter the axis. Causes of right axis deviation include: 1) lateral MI; 2) ventricular ectopy; 3) pre-excitation; 4) hyperkalemia; 5) acute or chronic lung disease; and 6) left posterior fascicular block. In this ECG, lack of findings to corroborate the other etiologies points toward another source of conduction disease—left posterior fascicular block.1
Normal conduction travels through the atrioventricular node, into the common bundle, and then divides into the left and right bundles. The left bundle is subdivided into anterior and posterior fascicles. Disruption of both fascicles produces a left bundle branch block (LBBB), but it is possible for a single fascicle to fail. A “bifascicular block” occurs when conduction fails in 2 out of 3 fascicles (RBBB + either LAFB or LPFB). Ventricular conduction is then reliant on the single remnant fascicle.
Left anterior fascicular blocks lead to leftward axis deviation while left posterior fascicular blocks lead to rightward/downward depolarization and subsequent right axis deviation (Figure 3).2
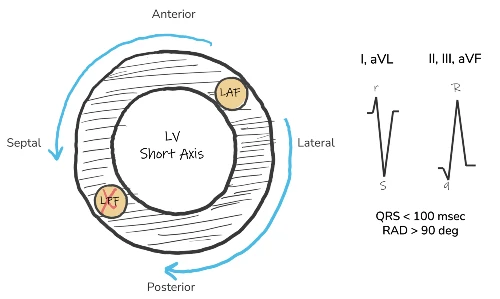
Our patient’s ECG suggests bifascicular disease: Right bundle branch block (ie, RSR’ in V1 and deep S-wave in I, V6) and a left posterior fascicular block (ie, right axis deviation, rS in leads I and aVL, qR in leads II, III, and aVF). It is important to note that while a left bundle branch block involves two fascicles, the term “bifascicular block” is reserved for the combination of a RBBB + either LAFB or LPFB.1
The significance of a bifascicular block depends on the clinical context. If this is an incidental finding, it is appropriate for outpatient follow up. These diseased conduction pathways are often due to underlying structural heart disease. Patients with ECG evidence of conduction disease should be viewed with a low threshold for evaluation or transfer. ECG evidence of a bifascicular block and history of syncope or palpitations is concerning for progression to intermittent complete heart block.3
The patient was ultimately discharged home with nasal saline for epistaxis and PCP/cardiology follow-up. No further emergent workup was indicated due to the lack of high-risk symptoms.
What to Look For
- The combination of a right bundle branch block with axis deviation suggests the presence of a concomitant fascicular block (either left anterior or posterior fascicular block).
- To diagnose a left posterior fascicular block, look for right axis deviation unexplained by an alternative diagnosis
Pearls for Management, Considerations for Transfer
- Incidental bifascicular blocks call for no further evaluation or therapy.
- Symptomatic patients (chest pain, syncope, palpitations) should be transferred for further workup and monitoring.
References
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm. Circulation. 2019;140(8):e382-e482. doi:10.1161/CIR.0000000000000628
- Cooper B, Giordano J, Fadial T, Reynolds C. ECG Stampede: Workbook. 1st ed. Null Publishing Group; 2024.
- Cooper BL, Giordano JA, Fadial TT, Reynolds CE. ECG Stampede: A Case-Based Curriculum in Electrocardiography Triage. 1st ed. (Cooper BL, ed.). Null Publishing Group; 2021.

Download the Article PDF: 74-Year-Old With Lightheadedness
