Published on
The patient is a 37-year-old man who reports a two-day history of chest pain. It worsens with exertion, and when he lays back; it improves when he’s sitting or leaning forward. He denies any diaphoresis, radiation, or back pain. No pleuritic aspect.
During the exam, he is alert and oriented, and in no distress. In addition, you find:
- Lungs: Clear to auscultation bilaterally
- Cardiovascular: Regular rate and rhythm without murmur, rub, or gallop
- Abdomen: Soft and nontender without rigidity, rebound, or guarding. No pulsatile abdominal mass
- Extremities: No pain or swelling of the lower extremities; pulses are 2+ and equal in all 4 extremities
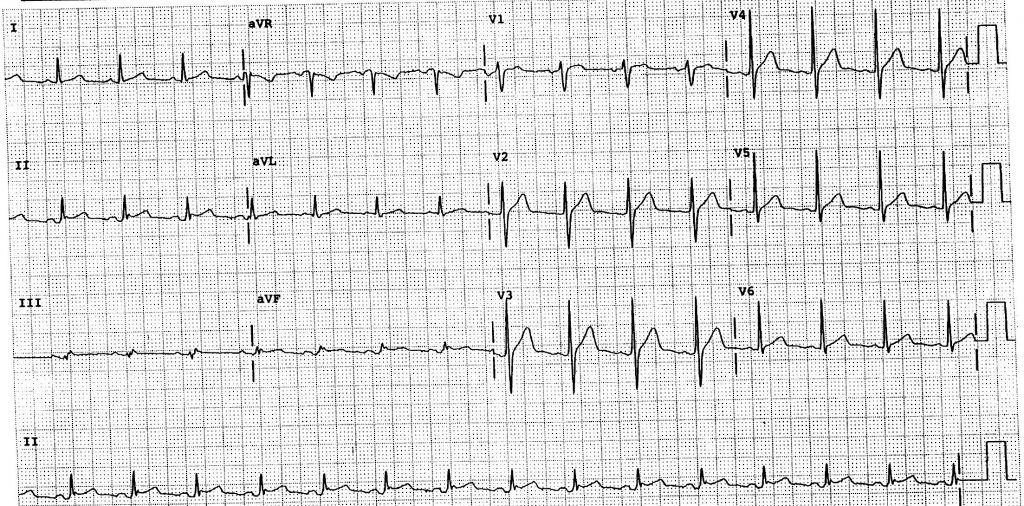
View the ECG (Figure 1) and consider what your diagnosis and next steps would be. Resolution of the case is described on the next page.
| 66 years | |
| PR | 149 |
| QRSD | 90 |
| QT | 310 |
| QTc | 379 |
| Axes | |
| P | 60 |
| QRS | 42 |
| T | 35 |
A 37-Year-Old Man with a Two-Day History of Chest Pain
1 2