Urgent message: Superior mesenteric artery syndrome should be included in the differential diagnosis in children with abdominal pain and weight loss with rapid increase in linear growth.
Ralph Mohty, MS3, and Michael Esmay, MD
Introduction
Abdominal pain is one of the most common complaints in childhood. A minor self-limited condition such as constipation or viral gastroenteritis is usually the cause, but more serious conditions need further evaluation and management.1
Chronic abdominal pain is a term used to describe intermittent or constant abdominal pain (of functional or organic etiology) that has been present for at least 2 months.2
Numerous etiologies cause abdominal pain in older children and adolescents, but fewer cause intermittent abdominal pain associated with vomiting.1 Such conditions—among many—include gastroenteritis, intussusception, food poisoning, malrotation with midgut volvulus, incarcerated inguinal hernia, adhesions with intestinal/bowel obstruction, and superior mesenteric artery (SMA) syndrome.
Case Presentation
RB is a 12-year-old Caucasian female who presented to the urgent care (UC) for evaluation of abdominal pain associated with nausea and vomiting. Patient started to have abdominal pain 5 days prior to presenting to UC. Patient reported epigastric pain with occasional radiation to the back and to the left upper quadrant. Pain was worse when lying flat, and was relieved when she leaned forward or laid on her left side. It was also better when she drew up both knees. Parents reported that she had grown about 5 inches in the past year but that she had lost weight during the same time frame. The parents attributed the weight loss initially to their daughter being recently self-conscious of her body image and later because of the episodes of nausea and vomiting. She reported that her emesis is normally gastric contents but over the past couple of days had become more bilious and green in color. Patient denied any fever or chills. She also denied diarrhea, blood in the stools, urinary symptoms, upper respiratory symptoms, headaches, shortness of breath, vision changes, dysphagia, and extremity edema. Patient had no anorexia and indicated that she was hungry. She reported occasional constipation and that her last bowel was movement was 2 days prior to her urgent care visit.
Patient has had three similar prior episodes of abdominal pain and vomiting. Patient was evaluated once in the emergency department and had normal CBC, CMP, lipase, and amylase, as well as a normal abdominal U/S. Previous episodes lasted 2–4 days and resolved on their own. No definite diagnosis was given at the time of her initial evaluation.
The patient had recently started menarche, started spotting 2 days prior to her urgent care visit.
Patient’s surgical history included adenoidectomy at age 4. She was not receiving any medications, had no allergies, and had no significant family history except hypothyroidism in her father.
Physical Examination
On initial presentation, the patient’s vital signs were as follows:
- Height: 4 ft, 8 in (142 cm)
- Weight: 49.5 kg (109 lbs)
- Temperature: 98.3°F (36.8° C)
- Pulse: 85 beats/min
- Respiratory rate: 16 breaths/min
- Oxygen saturation: 98% on room air
Findings on physical examination: Thin female in no acute distress, alert and oriented
Eyes: Anicteric sclera.
Lungs: Clear to auscultation
Heart: Regular rate and rhythm
Abdominal exam: Soft and nondistended with tenderness in the left upper quadrant without rebound or guarding. No palpable masses and no scars seen
GU: No inguinal hernias
Extremities: No clubbing, cyanosis, or edema
Psych: Normal affect
Abdominal ultrasound: Normal
Urinalysis: Negative
Laboratory test results are shown in Table 1.
| Table 1. Laboratory test results | |
| Test | Value |
| WBC | 9.0K |
| Hematocrit | 46.8 |
| Hemoglobin | 15.5 |
| Platelets | 103K |
| Sodium | 136 |
| Potassium | 3.3 |
| Chloride | 89 |
| BUN | 31 |
| Creatinine | 1 |
| Bicarbonate | 31 |
| Total bilirubin | 0.9 |
| ALT | 17 |
| AST | 20 |
| Alkaline phosphatase | 209 |
| Lipase | 30 |
While at the urgent care, the patient had two episodes of bilious vomiting. In view of the recurrent episodes of abdominal pain associated with nausea and bilious vomiting, evaluation in the emergency room for etiologies like malrotation was necessary. The thin habitus and the increase in linear growth associated with weight loss were suspicious for SMA syndrome.
Patient was hospitalized and had an upper GI that did not show any evidence of malrotation or structural abnormality of the esophagus or stomach, with normal esophageal and gastric motility.
Pediatric surgery services were consulted and agreed that clinically patient had SMA syndrome. Their recommendation was for patient to attempt to gain weight; if unsuccessful, she would have a nasojejunal feeding tube for a few weeks. They expected SMA syndrome to resolve with recovery of the lost weight and compensatory weight gain to match increase in linear growth.
Diagnosis
Superior mesenteric artery (SMA) syndrome.
Discussion
Superior mesenteric artery syndrome (also known as cast syndrome, Wilkie’s syndrome, mesenteric root syndrome, chronic duodenal ileus, and intermittent arterio-mesenteric occlusion) is an uncommon but well-recognized clinical entity characterized by compression of the transverse portion of the duodenum between the aorta and the superior mesenteric artery.3 It is a well-known complication of scoliosis surgery, anorexia, and trauma. Its diagnosis is frequently one of exclusion. Highest index of suspicion in an urgent care setting applies to patients following spinal fusion who present within the first week after surgery with vomiting and abdominal pain.4
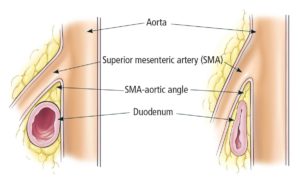
The superior mesenteric artery usually forms an angle of approximately 45⁰ with the abdominal aorta. The transverse part of the duodenum crosses caudal to the origin of the superior mesenteric artery, coursing between the superior mesenteric artery and aorta. Retroperitoneal fat and lymphatic tissue normally serve as a cushion for the duodenum, protecting it from compression by the SMA. Any factor that sharply narrows the aortomesenteric angle to approximately 6-25⁰ can cause entrapment and compression of that part of the duodenum as it passes between the superior mesenteric artery and aorta, resulting in SMA syndrome (Figure 1).
Incidence of SMA is unknown, but up to 0.78% of the findings from upper GI studies support a diagnosis of SMA syndrome. More females are affected by SMA syndrome; two thirds of the cases involve women. It usually occurs in older children and adolescents—75% of the cases occurred in patients 10‒30 years of age.5
Delay in the diagnosis of SMA syndrome can result in malnutrition, dehydration, electrolyte abnormalities, gastric pneumatosis and portal venous gas, formation of an obstructing duodenal bezoar, hypovolemia secondary to massive GI hemorrhage and even death secondary to gastric perforation.6–8
Typically, three quarters of the cases are treated medically, while the rest require surgical treatment. Medical treatment is attempted first, except when upon presentation emergency surgery is deemed necessary. A 6-week trial of medical treatment is recommended in pediatric patients.9 Medical treatment is aimed at weight gain and interventions to resolve the underlying conditions and may involve proper nutrition with replacement of fluid and electrolytes by a jejunal tube or nasogastric tube or PICC line, placement in the prone or lateral decubitus position, inserting a nasogastric tube for gastric and duodenal decompression, and starting promotility medication like metoclopromide. Symptoms usually improve after restoration of weight. If medical treatment fails, then surgical intervention is required.
Common operation for SMA syndrome is duodenojejunostomy. Other operations like gastrojejunostomy, anterior transposition of the third portion of the duodenum, intestinal derotation, division of the ligament of Treitz, and transposition of the SMA are less common.10
Prompt recognition of SMA syndrome and treatment after other serious conditions like malrotation are ruled out is of utmost important to avoid fatal catabolysis, dehydration, hypovolemic shock, upper GI bleeding, and cardiovascular collapse. If there is no delay in diagnosis and treatment, then the expected outcome for SMA syndrome treatment is generally considered to be excellent.
Citation: Mohty R, Esmay MR. Intermittent abdominal pain and vomiting in a teenager: one more urgent cause to consider. J Urgent Care Med. September 2017. Available at: https://www.jucm.com/intermittent-abdominal-pain-vomiting-teenager-one-urgent-cause-consider/.
References
- D’Agostino Common abdominal emergencies in children. Emerg Med Clin North Am. 2002;20(1):139-153.
- Kelly D, Bremner R, Hartley J, Flynn D. The Child with Abdominal Pain. In: Kelly D, Bremner R, Hartley J, Flynn D, eds. Practical Approach to Paediatric Gastroenterology, Hepatology and Nutrition. Oxford, UK: John Wiley & Sons, Ltd; 2014.
- Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527-1537.
- Altiok H, Lubicky JP, DeWald CJ, Herman JE. The superior mesenteric artery syndrome in patients with spinal deformity. Spine. 2005;30(19):2164-2170.
- Baltazar V, Dunn J, Floresguerra C. Superior mesenteric syndrome: an uncommon cause of intestinal obstruction. South Med J. 2000;93(6):606-608.
- Gerasimidis T, George F. Superior mesenteric artery syndrome. Wilkie syndrome. Dig Surg. 2009;26(3):213-214.
- Lim JE, Duke GL, Eachampati SR. Superior mesenteric artery syndrome presenting with acute massive gastric dilatation, gastric wall pneumatosis and portal venous gas. Surgery. 2003;134(5):840-843.
- Fuhrman MA, Felig DM, Tanchel ME. Superior mesenteric artery syndrome with obstructing duodenal bezoar. Gastrointest Ends. 200357(3):387.
- Ko KH, Tsai SH, Yu CY, et al. Unusual complication of superior mesenteric artery syndrome: spontaneous upper gastrointestinal bleeding with hypovolemic shock. J Chin Med Assoc. 2009;72(1):45-47.
- Biank V, Werlin, S. (2006). Superior mesenteric artery syndrome in children: a 20-year experience. J Pediatr Gastroenterol Nutr. 2016 Jun 8. [Epub ahead of print] No abstract available. PMID: 27280749 42(5):522-525.


