Urgent message: Chest pain is both more common and, typically, less concerning in children than in adults. If anything, however, this underscores the importance of guarding against a false sense of safety in low-risk causes, and maintaining vigilance for life-threatening etiologies.
SABAH F. IQBAL, MD, FAAP and HANSEL OTERO, MD
The case: A 12-year-old healthy African-American boy presents to urgent care with 2 days of midsternal chest pain, which is worse when he’s taking big breaths. It is not changed by exercise or rest, and no medications have been taken for the pain. While he has had a mild cough with runny nose, he has had no fevers, shortness of breath, vomiting, or palpitations. His mother is concerned about a heart attack, as occurred in his father just a few months previous. On examination, the patient is well appearing and in no distress with a HR of 103, RR of 18, a BP of 110/73, and an oxygen saturation of 99% on room air. His examination is significant only for tenderness to palpation along the left sternal border.
Relative to adults, acute chest pain in children is very common and generally much less worrisome. Fewer than 2% of cases with pediatric chest pain have a cardiac origin, and chest pain is rarely the presenting complaint in an otherwise healthy child with acute cardiac illness.1 While pediatric chest pain is often benign, a systematic approach is necessary to exclude potentially serious causes.
HISTORY AND EXAM PEARLS
Musculoskeletal etiologies are the most common causes of pediatric chest pain; therefore, the presence of reproducible tenderness in the ribs or muscles is the best clinical indicator to suggest a benign cause (in the absence of other red flags). Muscular or bony tenderness can occur from the growing pediatric skeleton (costochondritis), from a muscle strain (eg, lifting weights), or from a coughing illness causing muscle strain or, rarely, a fractured rib.2 Chest pain can also be caused by coughing itself; the etiology of cough should be sought and simple upper respiratory infections should be differentiated from diseases of the lower airways and lung parenchyma.
A cardiac cause of chest pain is very unlikely if the child lacks a history of heart disease or cardiac surgery and denies palpitations, dizziness, dyspnea, cyanosis, syncope, and extremity edema. In a young child, palpitations are often described as a fast heartbeat or a racing heart, but may be described simply as chest pain. Both exercise-induced chest pain and dyspnea with exertion are uncommon in children, and these presentations always require further evaluation. Cardiac exam clues may be difficult to elicit in a young child, but attention to pertinent findings is important. A friction rub is suggestive of pericarditis; a murmur that gets louder with Valsalva maneuver (decreased venous return) is suggestive of a hypertrophic cardiomyopathy; hepatomegaly may be suggestive of depressed cardiac output. Patients with pericarditis or mediastinal masses often have chest pain that worsens when supine (restricted venous return) and improves when the child sits up or leans forward.
All cardiac exams should assess upper and lower pulses, extremity edema, and capillary refill. It is important to ask about family history of arrhythmias, heart disease at a young age, and sudden unexplained deaths (especially single car accidents) that may increase risk for underlying congenital heart disease. In adolescents, cardiac chest pain can occur from drugs of abuse, such as cocaine or heroin, or abusing medications, such as methamphetamines that cause significant tachycardia. Synthetic cannabinoids also can precipitate cardiac chest pain. A thorough history of medication use and drug abuse should be sought in all adolescent patients presenting with chest pain.
| Differential Diagnosis What’s common
What not to miss
What to think about
|
While wheezing is a fairly obvious cause of chest discomfort, some may have such severe bronchospasm that no breath sounds are diminished (known as the “silent chest”). Bronchodilator therapy will precipitate a wheeze in these children as the bronchospasm relaxes enough to allow air movement. Asymmetric wheezing in young children without a history of asthma should prompt concern for aspirated foreign body. Children with tachypnea, cough, or dyspnea with or without wheezing should have pulse oximetry testing that may signify poor air exchange or intrinsic lung disease.
Assessing a child’s general activity level is an important indicator to exclude a potentially serious cause. A child with chest pain who is very fatigued, for example, should be approached differently than a child who is well-appearing and active. Fatigue can be a sign of cardiopulmonary disease, infection, or depression.
Additional risk factors should be elicited when the cause of chest pain is not readily apparent. A pulmonary embolus, for example, is quite uncommon in pediatric patients but should be considered when risk factors are present, such as: underlying malignancy, nephrotic syndrome, obesity, prolonged immobilization, and adolescents taking birth control.
In the absence of obvious historical or exam indicators, attention to vital signs is imperative. Patients with tachypnea, tachycardia, hypoxemia, or hypertension without an obvious cause warrant further evaluation.
DIAGNOSIS AND MANAGEMENT
Musculoskeletal
Costochondritis
Costochondritis is related to growth spurts and is commonly seen in adolescents, reflecting times of most rapid growth. The hallmark of costochondritis is the presence of reproducible chest pain, most often along the sternal border. Patients with costochondritis have no signs of cardiac compromise and should deny dyspnea, dizziness, syncope, and palpitations. Reassurance should be given to the parent, with nonsteroidal anti-inflammatory medications and heat packs for pain relief.
Muscle Strain/Chest Wall Pain
Chest pain from muscle strain or chest trauma is most common in adolescents who participate in weight-lifting or gymnastics. Pain is very localized and reproducible. In the case of trauma, there may be localized swelling or erythema. Imaging is rarely necessary, unless there is indication of deeper injury, such as shortness of breath, which may indicate a pulmonary contusion in the presence of significant blunt trauma. Rest, reassurance, and nonsteroidal anti-inflammatory medications are therapeutic.1 Muscular chest pain commonly occurs in young children with upper respiratory infections where frequent coughing causes straining of extrinsic muscles.
Precordial Catch
Precordial catch, also known as Texidor’s twinge, is a sharp, brief (a few seconds only) pain at the left lower sternal border or the apex. Etiology is unknown, but has been related to poor posture. Again, rest and reassurance are the most important therapeutic measures.1
PULMONARY
Wheezing
Pulmonary disease accounts for approximately 2%─11% of chest pain in children,1 most frequently from wheezing and bronchospasm. Chest radiographs are not routinely necessary in patients with wheezing and chest pain unless the wheezing is focal and does not vary after bronchodilator therapy (or cough). If wheezing is the cause of chest pain, the symptoms should resolve with bronchodilator therapy and corticosteroids. Persistent chest discomfort may require further investigation.
Pneumonia
Children with pneumonia can be diagnosed clinically or radiographically. Children typically cannot expectorate mucus until at least 8 years of age, therefore clinical signs of pneumonia may include vomiting and abdominal pain, in addition to more typical symptoms of fever, cough, malaise, and tachypnea. While a chest radiograph may show an area of consolidation, radiographic findings often lag behind clinical findings, so a normal chest radiograph is common in the setting of early clinical pneumonia. Narrow-spectrum antibiotics (eg, amoxicillin) should be initiated for routine community-acquired pneumonia. Patients with pneumonia complicated by hypoxemia, pleural effusions, or signs of empyema likely will require additional care past the scope of an urgent care center.
Pulmonary Embolus (PE)
Patients with PE generally present with dyspnea, pleurisy, and chest pain. An ECG may show right heart strain pattern (S1Q3T3) or other signs of right heart overload (ST-T wave changes); however, ECG findings are neither sensitive nor specific. Adolescents with dyspnea or tachypnea who have risk factors or ECG findings and no other obvious cause should be referred to a higher level of care for more comprehensive diagnostic testing and management
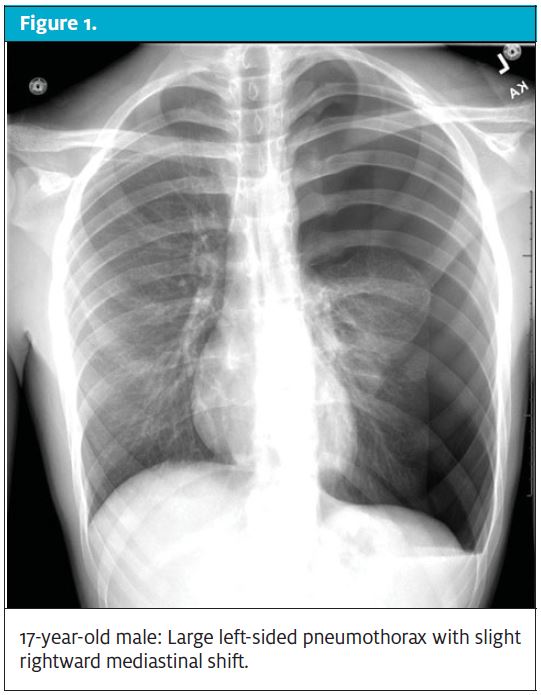
Pneumothorax
Pneumothoraces can be spontaneous or secondary to pulmonary disease, such as asthma or cystic fibrosis. In pediatrics, both spontaneous and secondary pneumothoraces occur mostly in adolescent males. Spontaneous pneumothorax is more common in those with thin, tall bodies. While a spontaneous pneumothorax can occur at rest, more often it occurs after a brief increase in intrathoracic pressure with forceful coughing or sudden weight-lifting.3 Management of pneumothoraces depends on the relative volume and the physiologic status of the patient. Patients with small pneumothoraces who are comfortable may need only oxygen therapy via non-rebreather mask. Patients who have larger pneumothoraces and/or significant discomfort require referral/transport for tube thoracostomy.
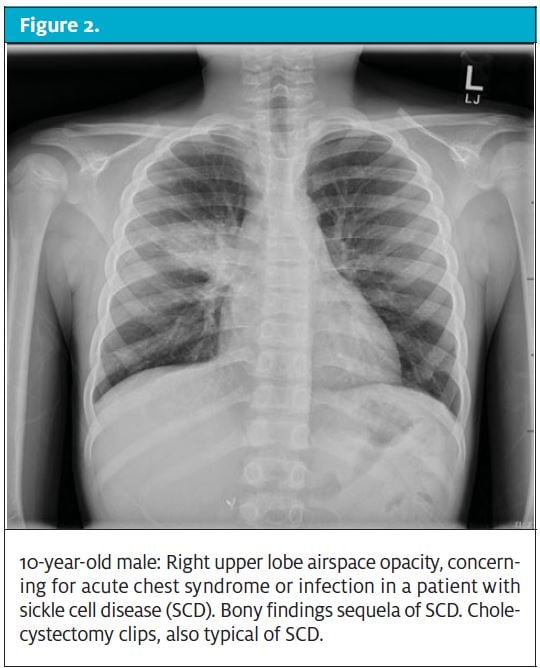
Acute Chest Syndrome (ACS)
In patients with sickle cell disease, chest pain should prompt an immediate evaluation for ACS. ACS is the sickling of red blood cells within the pulmonary vasculature, resulting in vaso-occlusion, ischemia, and injury to the endothelium. ACS is the leading cause of death in patients with sickle cell disease.4 The diagnosis is made by the presence of a new infiltrate on chest radiography, plus one of the following: fever, tachypnea, chest pain, or hypoxemia. Pulmonary infection, inflammation, and bronchospasm can precipitate ACE. Vaso-occlusive crisis in the chest wall leading to hypoventilation can also result in ACS. Hypoventilation from narcotic administration or from pain can also result in the development of ACS. ACS is most commonly seen in children with Hgb SS ages 2-4 years old.5 ACS also more commonly occurs in children with a history of asthma.6
When a child with sickle cell disease presents with chest pain, vital signs should be closely assessed for fever, hypoxia, and tachypnea. A low blood pressure is especially concerning for sepsis. Chest radiographs will show a new pulmonary infiltrate. Of note, children with sickle cell disease may have cardiomegaly at baseline, as a result of chronic anemia and a high-output state. Treatment consists of hydration, pain control, antimicrobials, and correction of any underlying anemia (if significant). While the role of corticosteroids is important in patients with coexisting asthma, there is some reluctance in use with sickle cell chest pain because of some data demonstrating more frequent readmissions, longer hospital length-of-stay, stroke, and renal infarction.
GASTROINTESTINAL TRACT
Gastroesophageal Reflux
Ten percent of pediatric patients with chest pain will have gastroesophageal reflux. Chest pain as a presenting sign of gastroesophageal reflux is most common in older children and adolescents.7 Gastroesophageal reflux is most often described as a substernal “burning” and can be treated with dietary modification and medications, such as H2 blockers, antacids, and proton-pump inhibitors.8 Patients with esophagitis chest pain can be trialed with a dose of “magic mouthwash” (lidocaine diphenhydramine-Mg/Al hydroxide), which can be both diagnostic and therapeutic if it relieves the pain.
Esophageal Foreign Body (FB)
Foreign bodies such as hot dogs, nuts, round candies, coins, and other similar sized objects can cause partial esophageal obstruction, mostly in toddlers. Patients may present with drooling, tripoding, difficulty breathing, pain with swallowing, or chest discomfort. Management depends on the object, duration of symptoms, and anatomic location, but most obstructing esophageal foreign bodies will require further management in an ED.
CARDIAC
Pericarditis
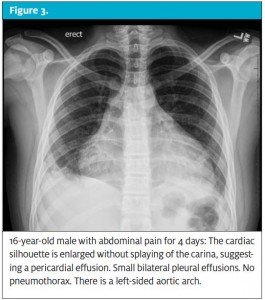
Pericarditis is an effusion around the pericardium, which often presents with a stabbing/sharp pain in the center of the chest along with tachycardia, palpitations, and a narrowed pulse pressure. An EKG may show diffuse ST elevation early in the course of the disease, T wave inversions later on, and low voltages throughout. A chest radiograph may show an enlarged cardiac silhouette. Pericarditis in children is most commonly secondary to enteroviral infection, Lyme disease, or rheumatologic disease but, regardless of etiology, requires prompt transport for evaluation by a pediatric cardiologist.
Myocarditis
Myocarditis is a rare, but potentially fatal, disease often caused by enteroviral infections. Chest pain is not a common complaint in myocarditis; however, it can be part of a clinical spectrum that may include tachypnea, tachycardia, abdominal pain, and lethargy. ECG may show a wide range of abnormalities, including ST wave abnormalities, low voltages, and QT prolongation.9 Radiograph of the chest often shows an enlarged cardiac silhouette. Myocarditis can worsen quickly, therefore immediate transport to a specialty center is indicated if there is concern for a myocardial infection or state of depressed cardiac output.
Myocardial Infarction (MI)
MI in children is exceedingly rare, with an incidence of 6.6 events per 1 million patient-years,10 most commonly following cardiac illness such as Kawasaki disease or myocarditis. MI can be related to anatomic abnormalities, such as anomalous coronary artery, aortic stenosis, or hypertrophic cardiomyopathy. These cases most commonly present in the preadolescent to adolescent years. The child’s chest pain will be exertional, therefore chest pain that is precipitated or worsens with exercise should prompt an ECG evaluation for signs of myocardial injury, as well as dysrhythmia.10,11 MI can occur after drug use, most commonly after cocaine, amphetamines, bath salts, or synthetic cannabinoids. Signs of MI in pediatric patients should prompt referral to a specialty center where a pediatric cardiologist can evaluate for structural abnormalities and perform a cardiac catheterization if necessary.
OTHER
Psychogenic Causes
Up to 9% of all patients presenting with chest pain will have a psychogenic etiology.7 This is more common in adolescents than in children, and is often precipitated by a stressful event.12 Many of these children will have underlying anxiety or depression.13 Simply discussing the stressful event or situation can help with the sensation of pain.
MANAGEMENT PEARLS
|
Case conclusion: The patient’s chest pain improved with ibuprofen, and his vital signs remained normal. He had a normal level of activity in the office and an unremarkable physical examination. His history was absent for red flags to suggest cardiac disease, foreign body aspiration, or other potential morbidities. No diagnostic testing was performed. He was discharged home with a diagnosis of chest wall pain and upper respiratory infection on NSAIDs, warm packs to the chest, and rest.
Citation: Iqbal SF, Otero HJ. Approach to the child with chest pain. J Urgent Care Med. October 2017. Available at: https://www.jucm.com/approach-child-chest-pain/.
References
- Reddy SRV, Singh HR. Chest pain in children and adolescents. Ped in Rev. 2010;31(1):e1-e9.
- Prasad S, Baur L. Fracture of the first rib as a consequence of pertussis infection. J Paedtr Child Health. 2001;37(1):91-93.
- Dotson K, Johnson LH. Pediatric spontaneous pneumothorax. Ped Emerg Care. 2012;28(7):715-720.
- Friedman KG, Alexander ME. Chest pain and syncope in children: a practical approach to the diagnosis of cardiac disease. J Pediatr. 2013;163(3):896-901.
- Canter SE, Simpson KE. Diagnosis and treatment of myocarditis in children in the current era. 2014;129(1):115-128.
- Lane JR, Ben-Sacher G. Myocardial infarction in healthy adolescents. Pediatrics. 2007;120(4):938-943.
- Thull-Freedman J. Evaluation of chest pain in the pediatric patient. Med Clin N Am. 2010;94(2):327-347.
- Neff J, Anderson M, Stephenson T, et al. REDUCE-PCP study: radiographs in the emergency department utilization criteria evaluation-pediatric chest pain. Pediatr Emerg Care. 2012;28(7) 715-720.
- Angoff GH, Kane DA, Giddins N, et al. Regional implementation of a pediatric cardiology chest pain giudeline using SCAMPs methodology. Pediatrics. 2013;132(4):1010-1017.
- Paul R, Minniti CP, Nouriae M et al. Clinical correlates of acute pulmonary events in children and adolescents with sickle cell disease. Eur J Haematol. 2013;91(1):62-68.
- Castro O, Brambilla DJ, Thorington B, et al. The acute chest syndrome in sickle cell disease: incidence and risk factors: The Cooperative Study of Sickle Cell Disease. Blood. 1994;84(2):643-649.
- Vichinsky EP, Neumayr LD, Earles AN, et al. Causes and outcomes of acute chest syndrome in sickle cell disease: National acute chest syndrome study group. New Engl J Med. 2000;(25):1855-1866.
- Sherman PM, Hassall E, Fagundes-Neto U, et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am J Gastroenterol. 2009;104(5):11278-11295.
- Selbst SM. Approach to the child with chest pain. Pediatr Clin North Am. 2010;57(6):1221-1234.
- McDonnell CJ, White KS, Grady RM. Noncardiac chest pain in children and adolescents: a biopsychosocial conceptualization. Child Psychiatry Hum Dev. 2012;43(1):1–26.