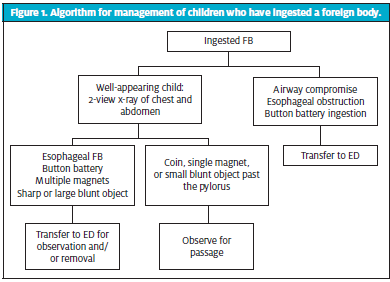
Urgent message: Less than one out of a hundred cases of children ingesting foreign bodies requires surgical intervention. Identifying which children that could apply to, which need endoscopic removal, and those who can wait for spontaneous passage is an essential role for the urgent care provider.
Herlene Chatha, MD and Hansel Otero, MD
The case: An otherwise healthy 2-year-old boy is brought to your urgent care center by his parents, who are concerned that he may have swallowed one or more coins. Approximately 30 minutes ago, the child’s mother heard him gagging and when she found him he was crying and holding his neck. He reports that he swallowed money he found on the floor. On arrival, he is quiet and tearful, in no distress, but points to his throat.
Each year in the United States there are more than 100,000 cases of foreign body ingestions reported, with over 80% of them in children.1 Most of these occur in children under the age of 5, and many are unwitnessed by a caregiver, making it difficult to obtain an accurate history. Whereas intentional ingestions are much more common in adult patients, the vast majority of cases in the pediatric population are unintentional ingestions of common household objects. Coins are the most common of these, accounting for up to two-thirds of ingested foreign bodies identified in children under the age of 10.2
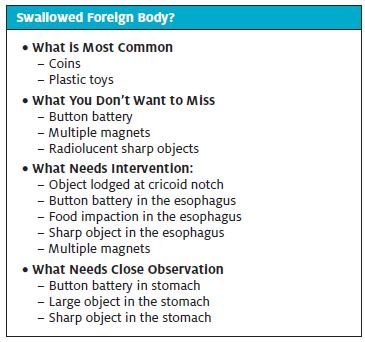
Once in the gastrointestinal tract, most foreign bodies will pass spontaneously and without incident. However, certain objects carry a much higher risk of complications if not removed in a timely fashion. Endoscopic removal is required in up to 20% of cases in which foreign bodies have been ingested by pediatric patients, while surgical intervention is required in <1%.3 Appropriate management of foreign body ingestions relies on accurate identification and localization of the object or objects ingested. This article will review the approach to evaluation, management, and disposition of a pediatric patient who presents to an urgent care facility with a known or suspected foreign body ingestion.
Evaluation
The majority of children who have swallowed a foreign body are relatively asymptomatic, so special attention is required for concerning symptoms and for those objects that carry the risk of potential complications.
The initial evaluation should assess for signs of airway compromise or esophageal obstruction, as well as for the ingestion of specific objects that would require emergent care. Stridor or wheezing may indicate a tracheal foreign body or tracheal compression caused by an object lodged in the esophagus. The inability to handle secretions suggests a near or complete esophageal obstruction. Severe neck pain, swelling, or crepitus in the neck may signal perforation of the esophagus by a sharp object.
In the absence of these acute symptoms, immediate attention should be given to accurately identifying the object in question. Button batteries are of particular concern and can be emergent if lodged in the esophagus, even without signs of distress. Since the majority of children with a suspected foreign body ingestion are asymptomatic at presentation, every effort should be made to obtain an accurate history as to the timing, quantity, and type of object believed to be ingested. The remainder of the physical exam should focus on signs of intestinal obstruction or perforation, such as abdominal distention, guarding, and tenderness.
Initial diagnostic evaluation for patients with a suspected radio-opaque foreign body ingestion consists of simple radiographs. The traditional approach is to obtain a complete foreign body series, including biplane radiographs (anteroposterior and lateral) of the neck, chest, and abdomen.4 A stepwise approach is reasonable if there is low suspicion for a poly-ingestion and the initial radiograph yields enough diagnostic information for appropriate management (eg, a coin that has passed the pylorus and is in the intestine).
A lateral radiograph of the neck/chest is suggested to confirm the absence of a tracheal foreign body when a presumed esophageal foreign body is visualized on the AP view. Additional views are important for recognition of discrete objects in a suspected poly-ingestion, particularly for objects with the potential to cause complications, such as multiple magnets. In addition to plain radiographs, any patient with high suspicion for ingestion of a radiolucent foreign body or with concern for intestinal obstruction may require referral for further imaging, such as a CT scan.4
Management
Referral to an emergency department is indicated for any symptomatic patient, especially those with:
- signs of airway compromise (eg, stridor, wheezing)
- signs of esophageal obstruction (inability to swallow or handle secretions)
- concern for intestinal obstruction (abdominal pain or distention, vomiting, fever)
- concern for an esophageal button battery
The patient with potential for airway obstruction or esophageal erosion requires immediate ambulance transport for emergent airway management and endoscopic removal of the ingested foreign body.
In an asymptomatic patient, management depends on the type and location of the specific object ingested. Radio-opaque foreign bodies found in the esophagus, especially those lodged at the cricoid notch, should be referred for endoscopic removal,5 although certain objects in the distal esophagus can often be observed to assess for safe passage into the stomach. With the exception of certain high-risk ingestions, most foreign bodies that have already passed through to the stomach may be allowed to pass through the intestines spontaneously. A small number of high-risk patients will require transfer to an ED for continued monitoring, or will need close outpatient follow-up. Further management based on the specific type of foreign body is detailed below:
- Coins: Most coins will pass through the gastrointestinal tract without causing any complications. Up to 30 % of coins lodged in the esophagus will pass into the stomach spontaneously, more commonly in asymptomatic older children and for coins found in the distal esophagus on initial radiograph.6 Any child with an esophageal coin should be referred to a setting with pediatric endoscopy capabilities. For distal esophageal coins, endoscopy may only be necessary if the coin is in an unchanged position on repeat radiographs or if the history suggests the coin was ingested >24 hours prior to presentation.5
If the coin has passed through the esophagus into the stomach, the patient may be followed at home with monitoring of stools and follow-up with their primary physician to discuss repeat radiographs should the coin fail to pass in 1-2 weeks.4 Parents must be instructed to recognize the signs of intestinal obstruction (eg, abdominal pain, vomiting).
- Batteries: Disk (button) batteries are similar to coins in that they are small and shiny, making them particularly appealing to young children. The use of larger and more powerful lithium batteries in many common household products has been linked to the increase in serious complications reported from ingested button batteries over the past two decades.7 Batteries lodged in the esophagus are a true medical emergency because conduction of electrical current can cause liquefaction and necrosis of the esophageal mucosa, leading to ulceration and perforation in as little as 8 hours following ingestion.5 Any battery in the esophagus warrants emergent endoscopic removal.
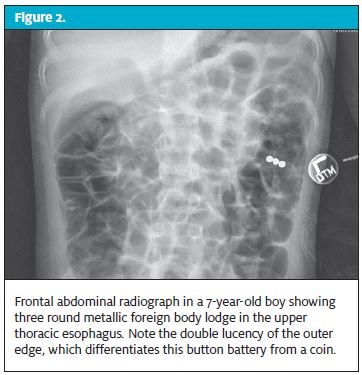
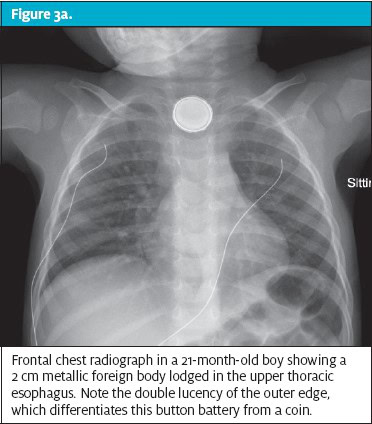
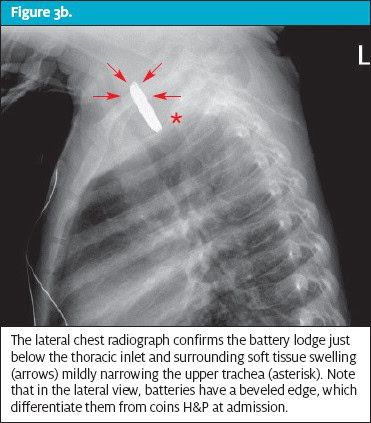
Close inspection of radiographs is needed to definitively distinguish esophageal coins from disk batteries. A “double-halo” sign on the anteroposterior view and a “step-off” sign on the lateral view are characteristic of disk batteries. It may be difficult to distinguish stacked coins from disk batteries on plain radiographs; the absence of a reliable history, the approach to management should assume a disk battery ingestion.
The presence of a battery in the stomach does not preclude esophageal damage,7 and retained batteries in the stomach can cause ongoing mucosal damage from direct pressure necrosis or leaking of caustic materials.3 Ingestions of larger batteries, especially in a younger child, pose a greater risk for gastric outlet or intestinal obstruction, and these patients should be referred for close observation and possible endoscopic removal if the battery fails to pass through the stomach in 48 hours.3
In the older asymptomatic child with a gastric battery <15 mm in size, close observation at home by a reliable caregiver may be an acceptable option. Stools should be inspected to confirm passage of the battery, and repeat x-rays may be indicated if the battery fails to pass within 1-2 weeks.8 Caregiver education should be provided, focusing on the signs of intestinal obstruction and perforation. Follow-up with the primary care provider is important to coordinate this ongoing care and to assure safe passage.
- Magnets: High-powered magnets composed of neodymium (also called rare earth magnets) are commonly found in many household appliances and toys. While most cases of unintentional magnet ingestions occur in small children, accidental ingestion has also been reported in adolescents using magnets to mimic piercings of the tongue and lips.5 Any child with a suspected magnet ingestion should have biplane radiographs of the neck, chest, and abdomen. Multiple magnets may stack together and mimic a single magnet on x-ray; at least two views are needed to accurately determine the number of magnets present.
Ingestion of multiple magnets or co-ingestion of a single magnet with a metallic object carries a high risk for complications because the attraction across adjacent bowel loops can result in pressure necrosis of the bowel wall, volvulus, obstruction, formation of a fistula, perforation, or infection.9
Patients with multiple discrete magnets apparent on radiographs warrant referral to a pediatric specialty center to consider available options for removal, including endoscopy or exploratory laparotomy. A single magnet identified in the esophagus or stomach is typically managed with observation alone unless the child has other risk factors warranting endoscopic removal. Subsequent imaging to follow progress of the magnet through the gastrointestinal tract should consist of biplane radiographs to ensure the absence of additional magnets that may not have been identified initially.10 Follow-up care with the primary care physician should be arranged prior to discharge, and both patients and caregivers should be instructed to avoid contact with any external magnets or metallic objects until passage of the ingested magnet has been confirmed.
- Sharp objects: Pointed objects such as pins, needles, fish bones, and toothpicks pose a high risk for perforation if lodged in the esophagus, and a high risk of complications as they pass through the gastrointestinal tract. Any patient with a sharp foreign body visualized in the esophagus on x-ray should be referred immediately to a pediatric specialty center. Many sharp objects, such as fish bones and toothpicks, are unlikely to be visualized on plain x-ray, and a high suspicion for ingestion of a sharp object warrants immediate referral for endoscopy. Once a sharp object has passed through the pylorus, discussion with a pediatric specialist is warranted to determine the need for immediate referral vs close follow-up.
- Large blunt objects: Objects larger than 5 cm have a high likelihood of impaction either at the level of the gastric outlet, duodenal sweep, or ileocecal valve.5 Any child with concern for intestinal obstruction or those found to have a large foreign body in the stomach should be referred to an appropriate facility for urgent removal. A large object that has passed into the small intestine may be managed by serial radiographs to follow its progression. Patients being discharged with close follow-up should receive anticipatory guidance on the signs of intestinal obstruction and perforation.
- Esophageal food impaction: Though food debris is the most common esophageal foreign body reported in adults, it is uncommon in children in the absence of underlying esophageal pathology.5 Food impaction usually presents as acute dysphagia while eating. These patients should be referred to an appropriate facility for a barium swallow esophogram and endoscopic removal of the impacted food, if indicated.
- Superabsorbent materials: Items such as disposable diapers and feminine hygiene products pose a high risk for obstruction if ingested, with the capacity to expand up to 30 to 60 times their original size as they pass through the gastrointestinal tract.5 Radiographs are of little use in identifying these objects because they are radiolucent. Any patient with a suspicion for ingestion of these substances should be referred for possible exploratory endoscopy, direct observation, and surgical consultation as needed.
- Esophageal radiolucent objects: Any partially obstructing esophageal foreign body should be considered for removal, especially if it has been lodged in the esophagus for >24 hours. With the exception of batteries and magnets, small blunt objects that pass through to the stomach usually progress without any complications. Parents should be instructed to examine the stool for passage, and subsequent radiographs can be obtained if needed. If an object fails to progress over a period of 4 weeks, or the child develops symptoms of concern (eg, abdominal pain, vomiting, gastrointestinal bleeding) surgical intervention for removal may be indicated.4
Case Resolution
Biplane radiographs of this 2-year-old patient show a round object lodged in the upper esophagus. A “double-halo” sign can be seen on the anteroposterior view, and there is a visible “‘step-off” sign on the lateral view that are characteristic of a disk battery. It is common for children to mistake button batteries for coins, and in this case the battery had been dislodged from the hearing aid of a visiting grandparent. The patient was sent by EMS to the nearest hospital, where an airway specialty team escorted the patient to the operating room where the battery was endoscopically removed under anesthesia.
Summary
The majority of foreign body ingestions occur in children under the age of 3 years, making it difficult to obtain an accurate history. Once ingested, most objects pass through the gastrointestinal tract without incident, though the potential for serious complications does exist, particularly with certain objects and in certain locations. Successful management of suspected pediatric foreign body ingestions in an urgent care setting depends on a timely and accurate recognition of high-risk ingestions. Rapid referral for removal of an ingested foreign body is indicated in the following situations:
- Signs of airway compromise (wheezing, stridor)
- Signs of esophageal obstruction (inability to handle oral secretions)
- A disk battery lodged in the esophagus
- Ingestion of a large, high-powered magnet or multiple magnets
- A sharp or large (>5 cm long or >2 cm wide) object in the esophagus or stomach
- Concern for intestinal obstruction or perforation (abdominal pain, vomiting)
For asymptomatic patients with low-risk ingestions, discharge is recommended with coordinated follow-up care and anticipatory guidance for signs of complications.
Citation: Chatha H, Otero H. Approach to ingested foreign bodies in children. J Urgent Care Med. December 2017. Available at: https://www.jucm.com/approach-ingested-foreign-bodies-children/.
References
- Wylie R. Foreign bodies in the gastrointestinal tract. Curr Opin Pediatr. 2006;18(5):563-564.
- Roura J, Morello A, Comas J, et al. Esophageal foreign bodies in adults. ORL J Otorhinolaryngol Relat Spec. 1990; 52(1):51-56.
- Antoniou D, Christopoulos-Geroulanos G. Management of foreign body ingestion and food bolus impaction in children: a retrospective analysis of 675 cases. Turk J Pediatr. 2011;53(4):381-387.
- Eisen G, Baron T, Dominitz J, et al. Guideline for the management of ingested foreign bodies. Gastrointestinal Endoscopy. 2002; 55(7):802-806.
- Kramer RE, Lerner DG, Kin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN endoscopy committee. J Pediatr Gastroenterol Nutr. 2015; 60(4):562-574.
- Soprano JV, Fleisher GR, Mandl KD. The spontaneous passage of esophageal coins in children. JAMA Pediatr. 1999; 153(10):1073-1076.
- Leinwand K, Brumbaugh D, Kramer R. Button battery ingestion in children: a paradigm for management of severe pediatric foreign body ingestions. Gastrointest Endosc Clin North Am. 2016; 26(1):99-118.
- Lee J, Lee J, Shim J, et al. Foreign body ingestion in children: should button batteries in the stomach be urgently removed? Pediatr Gastroenterol Hepatol Nutr. 2016;19(1):20-28.
- Si X, Du B, Huang L. Multiple magnetic foreign bodies causing severe digestive tract injuries in a child. Case Rep Gastroenterol. 2016;10(3):720-727.
- Pederiva F, Daniela C, Scarpa M, et al. An asymptomatic multiple magnet ingestion with transmesenteric entero-enteric fistula. APSP J Case Rep. 2014;5(2):16.


