Published on
Urgent message: While it makes business sense for the minority of urgent care facilities that do contract with and bill insurance as a primary care practice, the majority contract and bill as urgent care, given higher reimbursement and the numerous other benefits this provides an urgent care operation.
Alan A. Ayers, MBA, MAcc is Chief Executive Officer of Velocity Urgent Care, LLC and is Practice Management Editor of The Journal of Urgent Care Medicine.
In 2003, the Centers for Medicare and Medicaid Services (CMS) developed the “Place of Service-20” (POS-20), or “Urgent Care Facility” designation. It’s defined as “a location distinct from a hospital emergency room, an office, or a clinic, whose purpose is to diagnose and treat illness or injury for unscheduled, ambulatory patients seeking immediate medical attention.”
As most payer contracts align with the guidelines set by CMS, in the absence of extenuating circumstances or specific contract language to the contrary, most urgent care facilities use POS-20. An urgent care does also have the option, though, to contract with and bill a payer as POS-11 (ie, a “doctor’s office”) if its operational circumstances and market warrant it.
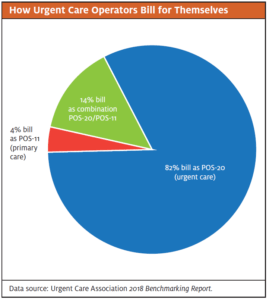
Following is a snapshot of how the urgent care industry approaches this issue, courtesy of the Urgent Care Association’s 2018 Benchmarking Report:1
- 86% of urgent cares provide an “episodic” scope of care
- 8% of urgent cares offer primary care in addition to urgent care, while roughly 3% are “hybrid” urgent care/PCPs
- Commercial contract restrictions are cited as the most common reason for not offering primary care services
- Similarly, 81% bill as POS-20 (urgent care), around 4% bill as POS-11 (PCP), and approximately 14% bill as a combination of POS-20/POS-11
- 11% of urgent care centers are dual contracted as UC/PCP
With those figures in mind, let us examine the advantages for an urgent care to contract and bill as POS-20, the few circumstances where it makes sense to contract and bill as POS-11, and the pitfalls of using POS-11 when POS-20 is the more appropriate and prudent choice.
Reasons to Contract and Bill as POS-20
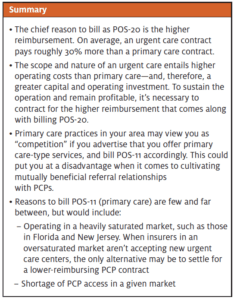
Higher reimbursement. The chief reason to bill as POS-20 is the higher reimbursement. When available, urgent care contracts always pay more than primary care contracts. (Remember, 81% of urgent care centers bill POS-20.)
On average, an urgent care contract pays roughly 30% more than a primary care contract. Typical reimbursements for urgent care are about $115.1 Because the UCA benchmarking average includes about 20% of centers billing POS-11 (for reasons we’ll discuss shortly), that national reimbursement average is necessarily lower than what is typically seen for a “pureplay” urgent care, which ranges from $130-$160 depending on the area of the country.
Primary care contracts billed as POS-11, as mentioned, are considerably lower. At the national level, we’ve seen reimbursement for PCP contracts in the $90s, which closely aligns with and is corroborated by data put forth by the American Academy of Family Practice.2
In states such as Virginia—which is unique insofar as the state legislature has established a website for reporting health costs and data—the average reimbursement for an adult primary care visit in Northern Virginia is listed as $77 (www.vhi.org).3 This figure is even lower than the national average, due in part to the large supply of primary care providers in the Washington, DC metropolitan area—resulting from large numbers of international medical graduates migrating to the D.C. area—a large and expanded Medicaid population, and the overall regional growth of managed care organizations that drive down reimbursement rates.
(Note: These are historical numbers and subject to change in 2020 with changes to CMS’s Medicare Physician Fee Schedule.)
Higher operating costs. The scope and nature of an urgent care operation entails higher operating costs than a primary care office and requires a greater capital and operating investment. To sustain the operation and remain profitable, it’s necessary to contract for the higher reimbursement that comes along with billing POS-20. The higher operating costs encompass some of the following:
- The need for greater visibility – Visibility to drive-by traffic is the number-one volume driver in urgent care. Urgent care facilities must be located in high-visibility, retail areas to draw ambulatory patients from off the street, whereas primary care offices can be tucked away in less expensive office buildings. Retail developments incur higher rents than office buildings due to the visibility and traffic they provide, the larger common areas and parking lots, and the landscaping that must be maintained. Further, larger properties have higher taxes.
- Larger facility – Urgent care is a volume-driven business that focuses on speed and service. A center must have greater square footage than a primary care office so it can quickly and efficiently move more patients in and out. Additionally, the build-out, fixtures, furnishings, and equipment for an urgent care center require a greater capital investment.
- Extensive onsite capabilities – Urgent care, unlike primary care, must have the capability to treat a patient’s nonemergency presentation on the spot. This requires an onsite x-ray machine, a procedure room to set fractures and apply sutures, and onsite labs for providing an instant diagnosis. This entails having a larger space with more specialized rooms and equipment to diagnose and treat a variety of conditions. Additionally, some urgent care centers dispense medications onsite. These requirements necessarily mean greater capital investment than a primary care office.
- Documentation of the patient chart. From the initial patient intake, primary care providers have a complete medical history for their returning patients, so there is no need to perform this kind of wellness exam on each visit. In an urgent care setting, though, each presentation is episodic, meaning the provider must perform a complete medical history and physical to address the specific medical concern, which requires more provider and staff time.
- Higher staffing levels – Urgent care centers must staff for nights, weekends, and holidays whereas PCP offices only staff for business hours 5 or 6 days a week.
- Less productive labor – Primary care visits are predictable and thus scheduled in advance, allowing the provider to adapt staffing levels to the expected demand. Urgent care, on the other hand, can have wide variability in demand depending on the season, day of week (eg, Monday mornings are the busiest), time of day (mornings are busier than afternoons), and factors such as whether flu or strep is going around. This requires staffing to the ebb-and-flow of walk-in traffic, so labor will therefore be less productive in urgent care.
- Marketing expenses – Primary care does not need to continually market to patients who are already established with the provider and will return three or four times a year for checkups and follow-ups. Urgent care is “retail medicine,” so there must be ongoing marketing campaigns to remain top-of-mind to consumers and create brand awareness in competitive markets.
Foster PCP relationships. To increase patient volumes, urgent care must cultivate mutually beneficial referral relationships with PCPs so that the PCP will refer their patients to the urgent care when the PCP office is closed, and a night/weekend/holiday need arises. Hence, when an urgent care center advertises services like “wellness exams” and “chronic disease management,” PCPs view the urgent care as direct “competition,” and may not refer their patients. Additionally, the POS-11 urgent care will not be found in payer directories when health insurance members search for “urgent care.” Urgent care and primary care should be complementary, not in competition.
Primary care disrupts flow in urgent care. The top metric for measuring patient satisfaction and labor productivity is time in the urgent care center—ie, door-to-door time. Performing activities that bill as POS-11 and not POS-20 (such as an initial PCP intake, ordering and reviewing labs, or reconciling prescriptions) can be time-consuming, especially for a new chronic patient. Combining PCP services with urgent care would therefore lead to wide variability in visit length, resulting in longer wait times.
As an aside, it’s overall bad policy for patients to attempt to manage a chronic condition in urgent care rather than with a PCP. The chronic patient walks in off the street and potentially sees a different provider each visit instead of having scheduled follow-ups with a single primary care provider. Chronic patients with conditions like diabetes and hypertension need a solid “medical home” where the providers are connected to local specialists and have hospital admitting privileges—one reason payers are moving patients to “panels” and paying providers “risk incentives” for positive health outcomes.
In short, the further the business strays from the “core” urgent care services, the less likely it is to perform well on the factors that differentiate urgent care from other providers.
Reasons to Contract and Bill as POS-11
As outlined, contracting and billing as POS-20 holds numerous advantages for urgent care, which is why it’s the standard. Payers set the reimbursement rates based on how much it should cost to deliver urgent care services and what’s needed for an urgent care center to survive. There are a couple extenuating circumstances, though, where billing POS-11 makes business sense for an urgent care provider, listed below:
Operating in a heavily saturated market. In some heavily saturated markets such as those in Florida and New Jersey, insurance companies may inform new centers that their network is “full of urgent care” and an urgent care contract simply isn’t available in their area. When an oversaturated market isn’t accepting any new centers, the only alternative is to settle for a lower-reimbursing PCP contract if the center wants to open.
Shortage of PCP access. Let’s say the urgent care operates in a rural or urban area where there is less PCP access and people are relying on urgent care to meet their PCP needs. What’s often the case is that these same rural areas with few PCPs also lack sufficient population density to support a “pureplay” urgent care. The urgent care will then engage in a mixed model of UC/PCP to serve more patients in the area.
When there indeed is a business model that offers both primary and urgent care, it’s typically handled in one of two ways:
- All PCP visits are billed as urgent care. This disadvantages patients with higher copays for sick visits and higher out-of-pocket costs, though, as routine PCP services like vaccinations and wellness exams are typically not reimbursable under urgent care contracts.
- The urgent care sets up a separate PCP business under the same roof. Their PCP business has a unique tax ID, creates separate primary care (POS-11) contracts with payers, and implements a process to segregate which patient traffic is urgent care (ie, walk-in, episodic) vs primary care (ie, scheduled appointments, wellness exams, quarterly follow-up on disease states like diabetes).
In sum, there are situations and circumstances where an urgent care can bill POS-11 and still be a viable business. We’ve seen other cases, however, where urgent care facilities billing POS-11 have run into a host of problems related to not being able to cover operating expenses, inefficient patient flow, PCP referral issues, credentialing, getting claims paid, and staffing that led to their eventual closure. Hence, it behooves each individual urgent care operator to assess their market, business model, facility, and capabilities before opting to bill and contract as POS-11 rather than POS-20.
Conclusion
For urgent care, billing POS-20 holds numerous benefits, chief among them establishing a consistent record of urgent care utilization in a given market that justifies a higher reimbursement for all surrounding centers. Additionally, the clear recognition of being an urgent care facility provides rationale for the higher costs of operating a walk-in facility when negotiating higher rates during contracting . There are a few legitimate circumstances, however, when an urgent care would bill POS-11, but those situations where it actually makes sound business sense are few and far between. POS-20 in the majority of cases is therefore the appropriate option to support a thriving urgent care operation.
References
- Urgent Care Association. 2018 Benchmarking Report. https://www.ucaoa.org/Resources/Industry-Reports/Benchmarking.
- American Academy of Family Physicians. AAFP to CMS: Make 2019 MPFS work for FPs, primary care. Available at: https://www.aafp.org/news/government-medicine/20190109mpfscomment.html. Accessed February 3, 2020.
- Virginia Health Information. Potentially Avoidable ED visits in 2017. Available at: http://www.vhi.org/Media/flyers/Potentially%20Avoidable%20ED%20Visits.pdf. Accessed February 3, 2020.

