Urgent message: Patients with minor traumatic brain injury can be difficult to assess. Identifying those at risk for poor outcomes is critically important in the urgent care setting.
Joseph Toscano, MD
The term traumatic brain injury (TBI) describes various injury patterns that result from force being absorbed by the brain after a rapid acceleration or deceleration or head impact. TBIs can span a spectrum from minor changes to fatal catastrophes and can affect patients in any age and demographic group.
Patients with more than minor injury are usually clinically identifiable; proper medical care involves initiating stabilizing measures and transferring those patients to the appropriate treatment setting. In the urgent care clinic, the primary challenge is sorting through the majority of patients with more minor complaints in order to identify those who might be at risk for poorer outcomes.
This article will review existing, urgent care-relevant medical literature and appropriate imaging criteria regarding clinical decision making. A second article, to be published in the April issue of JUCM, will describe the application of this evidencebased decision-making in urgent care medicine, and discuss some of the basic elements
of treating minor TBI, as well as injury prevention.
Pathophysiology
Contusive and shearing forces from an impact or acceleration/deceleration force sustained by the head can have a variety of deleterious effects, including hemorrhage in and around the brain and direct neuronal injury. For the most part, all of these lesions are apparent on CT scanning, which is the most useful imaging modality for patients with acute TBI—both to define injuries which are obvious clinically, and to screen for occult injuries in those who are at risk. Though MRI may be reasonable in some cases based on the clinician’s judgment, CT is better studied in the acute care setting and is known to be accurate, more widely available, and less expensive. MRI is more often reserved to image patients with ongoing concussion symptoms beyond the first few days.
Whether the injury is focal or diffuse, a careful history and neurological exam will usually reveal abnormalities; rarely, however, patients with significant intracranial in- juries will initially appear completely normal.
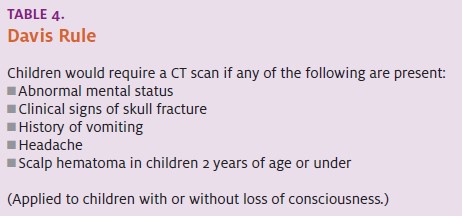
The occurrence of clinically occult but significant TBI is a sobering fact for anyone caring for one of these patients. A standardized clinical scale, the Glasgow Coma Scale (GCS) (Table 1), is typically used to assess patients with head injuries.
By adding points for a patient’s best response in each of three categories—eye opening, verbal responsiveness, and mo- tor responsiveness the GCS gives a global sense of a patient’s status at any point in time and over time. Scores range from 3 (deep coma) to 15 (normal); historically, mild injury has been defined as the presence of TBI with a GCS score of 13 to 15. Those with a GCS score be- tween 9 and 12 are defined as having moderate injury, with GCS scores 3 to 8 defined as severe injury.
Medical Literature Review
There is no literature which directly describes an approach to evaluating patients with TBI in the urgent care set- ting. Until this information is available, we must extrapolate from emergency medicine studies.
There are several difficulties with doing this directly.
The spectrum of injury in the emergency department is different than that typically seen in the urgent care clinic. The mere fact that patients with a GCS of 13 might be considered to have mild TBI may be uncomfortable for most urgent care practitioners to consider.
In addition, the latitude to observe patients for several hours, with ready access to CT scanning, distinguishes an emergency medicine approach to these patients from those which might be possible in the clinic setting. Still, there are study data that can be considered useful.
The portion of existing literature relevant to the urgent care clinician regards the development of decision instruments to select patients who need neurological imaging (i.e., to determine which patients can be dis- charged without CT scanning and which require this next-step in the evaluation). Decision rules that compensate by using a larger number of criteria or more general indicators increase sensitivity (the ability not to miss an injury), but decrease
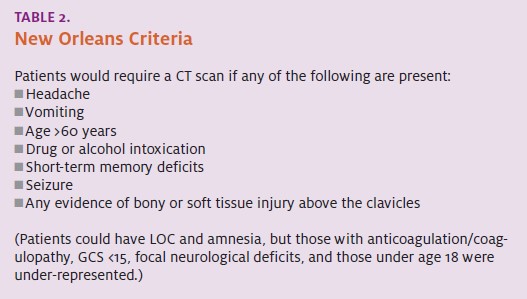
specificity (the ability to safely exclude it). The first of several groups to more recently publish a decision instrument for TBI was Haydel, et al in 2000.1 In a single paper, the authors described the derivation of their decision instrument (Table 2), usually referred to as the New Orleans Criteria. They found it to be 100% sensitive in detecting injuries when applied to a subsequent group of patients. The study has been criticized, however, for not being specific enough to decrease the need for neuroimaging in general; indeed, it em- ploys the criterion of “any evidence of trauma above the clavicles” as an indication for a CT scan.
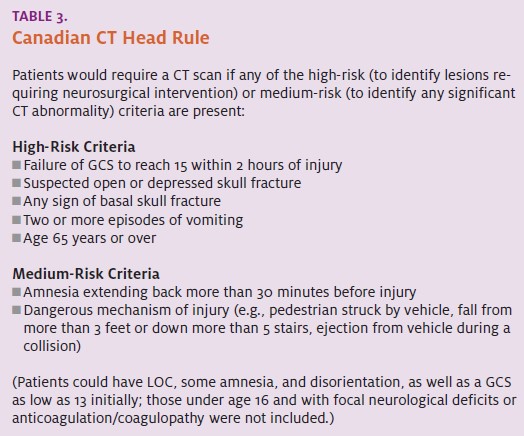
In 2001, the Canadian CT Head Rule (Table 3) was published.2 Though the rule was quite sensitive, study patients included only those over age 16, and up to two hours of observation were used to clear patients clinically, which limits its applicability in some patient-care settings.
Still, the use of the Canadian high-risk criteria was 100% sensitive for injuries requiring neurosurgical intervention, and only 32% of patients in their study population would have required scanning with this strategy; these patients included those with loss of consciousness, some amnesia, and disorientation, as well as those with a GCS as low as 13.
Several studies have confirmed the high sensitivity of both the New Orleans criteria and the Canadian CT Head Rule, while the conclusions reached in at least one study were less supportive. In addition, several studies from outside the U.S. have shown that implementation of either of these decision rules might actually increase imaging rates compared with general clinician judgment, without leading to the detection of additional intracranial injuries.
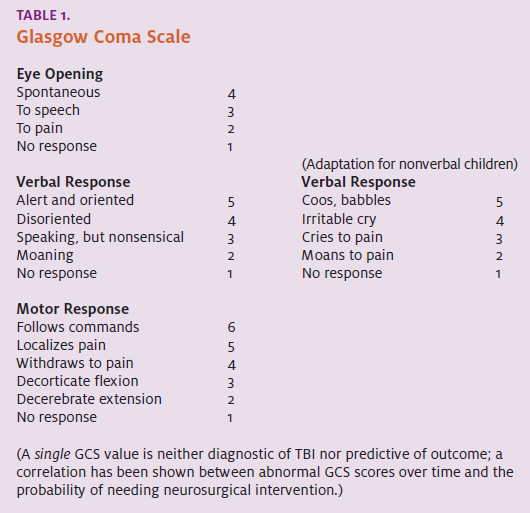
A group from the University of California, Davis and the Oregon Health & Science University sought to create a similar decision instrument specifically for children. The Davis Rule (Table 4), published in 2003, was found to be 99% sensitive for any traumatic brain injury and 100% sensitive in detecting injuries which required intervention.3
The study’s strength was the inclusion of patients as young as 10 days of age. In children £2-years-old (which includes 16% of the 2,043 patients included), the pres- ence of scalp hematoma was found to be a significant predictor of injury. However, this study also had the low- est level of inter-observer agreement of any of the variables , underscoring the need for a very careful scalp ex- amination in these children. Though it has yet to be externally validated, this rule is frequently used in the emergency department to make decisions about imaging in children after TBI.
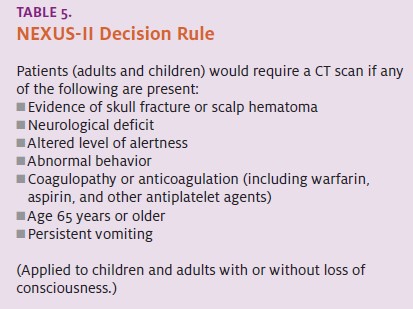
A more recent publication is the NEXUS-II study,4 which included children and adults with head trauma who had a GCS of 15, with or without loss of consciousness. Published in 2005 (a pediatric subgroup analysis was published in 20065), the NEXUS-II criteria (Table 3)
- proved to be 98.3% sensitive at identifying clinically important The rule would have missed one patient in that study who required immediate neurosurgical intervention, but most of those who would not have been scanned according to the rule had relatively minor injuries.
Unfortunately, specificity was low (13.7%), and these criteria have yet to be validated beyond the ini- tial study population.
Since NEXUS-II, other decision instruments for evaluating patients with TBI have been derived, including CHALICE6 and CHIP,7 but these have yet to be validated, too, and are considerably more complex than the earlier rules.
Specialty Society Guidelines
Apart from the individual studies described above, two specialty societies have published clinical practice guidelines regarding the care of patients with mild TBI. Each was developed using the available medical literature at that time, and, to some degree, consensus opinion.
AAP/AAFP Guidelines
In 1999, the American Academy of Pediatrics (AAP), together with the American Academy of Family Physicians (AAFP), published guidelines for the care of children with minor closed head injury.8 Their publication preceded the availability of any of the study data described above and has not been updated since.
The AAP/AAFP guidelines apply to patients aged 2- to 20-years-old who are evaluated within 24 hours of head injury. A thorough history and physical examination (including fundoscopic exam) is recommended, and patients with multiple trauma, known or suspected cervical spine injury, preexisting neurological disorder, bleeding diathesis, suspected intentional trauma, language barriers, or the presence of drugs or alcohol were felt to require individualized care outside of the guidelines.
Evidence of skull fracture or abnormal eye or neurological examination was felt to be an indication of the need for CT scanning and specialty consultation. For children without any of these exclusion factors and with a normal examination and no suspected skull fracture, the decision point for using CT scanning was the presence of brief (<1 minute) loss of consciousness, though headache, seizure following the injury, lethargy, and vomiting are also mentioned as worrisome findings. CT scanning, along with careful observation, was considered an option in the management of these children.
The routine use of skull films was not recommended. Those without loss of consciousness could be managed by observation alone. The period of observation recommended for any child with minor head in- jury is at least 24 hours by a competent caregiver with ready access to appropriate medical care if deterioration should occur.
If this is not available or possible, then admission to a hospital or other facility is recommended. In addition, maintaining a high index of suspicion is advised, even several days after minor head injury, if behavioral changes or other signs of worsening do occur. Clear, written instructions regarding care and follow-up should be given. Though not discussed directly by the guide- lines, those with more than brief loss of consciousness likely should be managed at least as aggressively.
The subject of discharge instructions and return to normal activities will be discussed more thoroughly in part II of this article in the April issue of JUCM.
ACEP Guidelines
The American College of Emergency Physicians’(ACEP) Clinical Policy guidelines were published in 2002 and had both the New Orleans and Canadian studies, as well as other existing literature, on which to rely.9
The strongly evidence-based policy limited its scope to patients >15 years of age with blunt trauma to the head within 24 hours of evaluation and a GCS of 15.
The guideline was applicable to those with post-traumatic loss of consciousness or amnesia of any duration, but excluded those with bleeding disorders, penetrating or multisystem trauma, or focal neurological findings.
The three main conclusions of the policy were as follows:
- Skull radiographs are not recommended in the evaluation of patients with
- Head CT scanning is not necessary in patients after head injury if they do not have headache, vomit- ing, post-traumatic seizure, drug or alcohol intox- ication, short-term memory deficits, physical exam evidence of trauma above the clavicles, or are £60 years of age (essentially mirroring the New Orleans Criteria).
- Patients who have a normal exam and CT scan (if indicated) may be safely discharged from the emer- gency department any time after six hours post- injury, or sooner if in the care of a competent person who can observe them for at least this
Specific Considerations
The Element of Time
The value of observing patients for improvement in nonfocal symptoms (i.e., initial loss of consciousness, amnesia, headache, seizure, vomiting) or GCS 13 or 14 over time is emphasized by the findings of the Canadian CT Head Rule study, as well as the AAP/AAFP policy.
Indeed, observation should be the cornerstone of the short-, intermediate-, and longer-term management of any patient with head injury. The optimum period of observation is uncertain, but close observation for two to six hours, with attention to any change even subtle ones for up to several days after head injury seems advisable. Any patient with a worsening level of consciousness or mental status, abnormal behavior, recurrent seizures, repeated vomiting, or the development of focal findings should be evaluated, preferably in the emergency department, in conjunction with CT scanning of the head.
An isolated but worsening headache after head trauma, though nonspecific, would also prompt CT scanning in most instances.
Infants and Children
Though toddlers and older children who appear neurologically normal after head trauma seem to be at about the same risk as adults for significant clinically occult intracranial injury, there is good evidence that infants are at increased risk of such after even minor falls (e.g., from sofas or beds).
In addition, infants and young children can be more difficult to assess reliably. Maintaining a high index of suspicion is important, and close observation should be emphasized for all of these patients, whether CT scanning is performed or not.
As noted earlier, the presence of a scalp hematoma has been shown in several studies to correlate to an in- creased risk of intracranial injury in infants and children, so careful consideration should be given this finding.
Finally, head trauma can be a presenting injury in children who are victims of abuse. In situations where the mechanism of injury is uncertain or difficult to believe, additional screening for child abuse is warranted.
Elderly Patients
Many characteristics put elderly patients at increased risk of sustaining significant injury after even relatively minor head trauma and often with a delay in the development of symptoms. Maintaining an extremely low threshold for imaging and observation for elderly patients, even with a normal exam and no other worrisome features, would seem to be a safe, and not excessive, strategy.
Anticoagulation/Coagulopathy/Antiplatelet Agents
The occurrence of rapid neurological deterioration following even very minor head injury in patients with coagulopathy or those on warfarin anticoagulation is well described.
This can occur after a period of clinical normalcy or even an initial brain CT scan which shows no hemorrhage or other acute abnormality performed soon after injury. The NEXUS-II study and others also suggest that at least some increased risk extends to those on aspirin, clopidogrel, and other antiplatelet therapies.
No specific guideline has been found to be useful for excluding the chance of injury in these patients, and a strategy that incorporates a period of several hours of observation with a low threshold for hospital admission, often combined with delayed (with or without immediate) neuroimaging is becoming common for these patients in emergency medicine practice.
Summary
The concept of clinically occult but significant TBI continues to be vexing to acute care clinicians. In the studies discussed in this article, and others, the incidence of an abnormality on brain CT in patients who appear normal after a minor head injury ranges from 3% to 13%, typically with £1% requiring neurosurgical intervention. Careful patient examination, combined with the appropriate use of CT scanning and observation, can help identify these patients.
Due to the overlap of symptoms in those with and without significant injuries, however, there is no proven strategy that allows practitioners to readily distinguish between those who need CT scanning and those who do not. In the end, each practitioner must decide, for each patient, the risks and benefits of the various possible courses of action.
Becoming familiar with one of the validated decision rules (New Orleans or Canadian), applying it consistently, knowing its limitations (e.g., age range, other excluded patient groups), and having a plan for patients for whom it is not applicable may be the most prudent strategy for some.
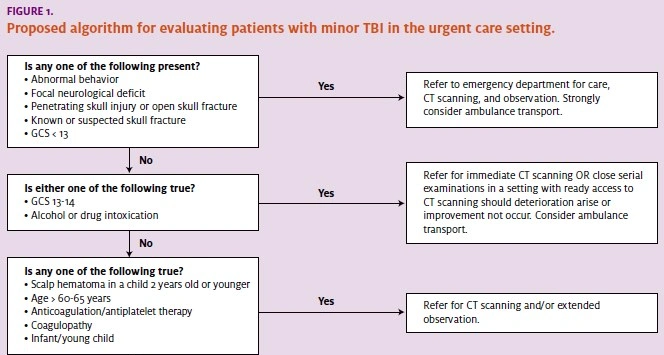
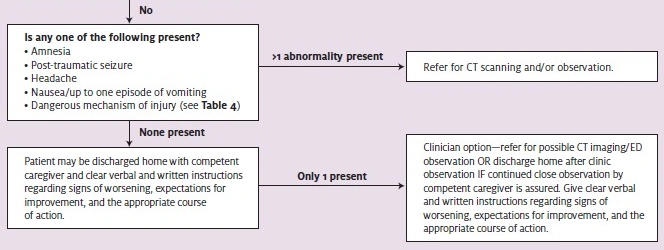
Using the information from all the studies in a more tempered approach, it is possible to clinically assign patients into one of three groups: those who definitely need referral and scanning based on the results of several studies those who definitely do not all those in between Such an approach would comprise the
following (Figure 1):
- Patients who present to the urgent care clinic with head injury can first be promptly and rapidly evaluated (history, GCS, HEENT and neurological exam) for any of the typically clinically obvious, highest-risk indicators—abnormal behavior; penetrating, open, or closed skull fracture; neurological deficit; or GCS <13.
These patients would most safely be transportedto the ED by ambulance, so calls to 911 should be made and provider-to-provider communication with the receiving facility initiated.
In the clinic, the staff should render all available stabilizing care, including efforts to maintain the patient’s airway, breathing, oxygenation, and circulation at a BLS level, at a minimum.
In the clinic, the staff improvement, and the subsequent appropriate course of action are important. Recommendations for such instructions will be included in part II of this article. A follow-up phone call after several hours and a scheduled appointment should render all available stabilizing care, including efforts to maintain the patient’s airway, breathing, oxygenation, and circulation at a BLS level, at a minimum.
- Patients with GCS 13 or 14 and those with drug or alcohol intoxication will require either prompt CT scanning and/or extended observation in a setting with prompt access to scanning, and should be transferred to the ED either by ambulance
- Patients who remain after this initial triage process will have a GCS score of 15 and a normal neurological exam, without At this point, a more thorough history and exam can be performed to aid decision making.
- Patients over 60 to 65 years of age, those on anti- coagulation or with coagulopathies, those with repeated vomiting, and children aged £2 years of age with a scalp hematoma should be referred for CT scanning; private auto transport should Clinicians should maintain a low threshold for referring infants and young children for scanning or ED observation, even if a scalp hematoma is not apparent.
- At the next decision level, patients may be found to have post-traumatic amnesia (memory deficits) or seizure, headache, up to one episode of vomiting, evidence of trauma above the clavicles (other than scalp hematoma in a child £2 years or penetrating injury or skull fracture in anyone), or a dangerous mechanism of CT scanning would be considered appropriate for these patients
Based on the most recent study data, however, if competent observation can be accomplished at home, it would not be unreasonable to discharge patients exhibiting one of these abnormal findings after a period of observation in the clinic during which the patient does not worsen, or particularly if he or she improves (e.g., improved memory, decreased headache, or decreased nausea).
A clear discussion supplemented with written instructions regarding the signs of worsening, expectations for improvement the following day can also provide reassurance to both the patient and clinician in this situation.
Because of the uncertain benefits and risks associated with any approach, it is always advisable to engage the patient, and the patient’s family in the case of children or other dependents, in the decision-making process. With further study, more data may inform more efficient decision making for patients with possible mild TBI.
In the meantime, careful patient evaluation, knowledge of the prevailing literature and recommendations, utilization of observation (in clinic and at home), and close collaboration with ED colleagues when necessary, form the basis of the most appropriate management of these patients in the urgent care setting. Decisions about referral and CT scanning of the brain can be made based on clinical variables which are typically apparent, and should be sought by the urgent care clinician.
REFERENCES
- Haydel MJ, Preston CA, Mills TJ, et Indications for computed tomography in patients with minor head injury. New Engl J Med. 2000;343(2):100-105.
- Stiell IG, Wells GA, Vandemheen K, et The Canadian CT head rule for patients with minor head injury. Lancet. 2001;357:1391-1396.
- Palchak MJ, Holmes JF, Vance CW, et A decision rule for identifying children at low risk for brain injuries after blunt head trauma. Ann Emerg Med. 2003;42(4):492-506.
- Mower WR, Hoffman JR, Herbert M, et al, for the NEXUS II Developing a decision instrument to guide computed tomographic imaging of blunt head injury patients. J Trauma. 2005;59(4):954-959.
- Oman JA, Cooper RJ, Holmes JF, et al, for the NEXUS II Performance of a decision rule to predict need for computed tomography among children with blunt head trauma. Pediatrics. 2006;117(2):e238-246.
- Dunning J, Daly JP, Lomas JP, et Derivation of the children’s head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Children. 2006;91(11):885-891.
- Smits M, Dippel DW, Steyerberg EW, et Predicting intracranial traumatic findings on computed tomography in patients with minor head injury: The CHIP Prediction Rule. Ann Intern Med. 2007;146(6):397-405.
- The Management of Minor Head Injury in Committee on Quality Improvement, American Academy of Pediatrics. Commission on Clinical Policies and Research, American Academy of Family Physicians. Pediatrics. 1999;104(6):1407-15. Available online at: http://aappolicy.aappublications.org/cgi/reprint/pediatrics;104/6/1407.pdf
- Jagoda AS, Cantrill SV, Wears RL, et Clinical policy: neuroimaging and decision mak- ing in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2002;40(2):231- Available online via: www.acep.org/practres.aspx?id=30060&coll= 1&collid=74.
- Radiation exposure in x-ray Radiological Society of North America. March 20, 2007. Available online at http://www.radiologyinfo.org/en/pdf/sfty_xray.pdf. Accessed No- vember 12, 2007.
- Ropper AH, Gorson Clinical Practice. Concussion. New Engl J Med. 2007;356(2):166- 172
- Edwards Head Trauma. In: Urgent Care Medicine. McGraw Hill Companies, Inc.; 2002:526-531.