Katie Jerzewski MD, Roshni Patel MD, and Joshua Rocker MD
OVERVIEW
The novel coronavirus, or SARS-CoV-2, first appeared in the Wuhan province of China in the winter of 2019. Due to the virus’s ability to spread from an asymptomatic carrier to the next new host and Wuhan being a pivotal commercial center, it spread quickly across the globe. Asymptomatic carrier rates have ranged from 1.6% to 56.5%, depending on clinical setting and testing availability.1 In adults, common symptoms include fever, cough, body aches, lack of smell and taste, dyspnea, and/or fatigue.2 During the initial New York City outbreak, 12.2% of hospitalized patients required intubation for acute respiratory distress syndrome (ARDS).2 In this New York cohort, outcomes for intubated patients were poor. The mortality rate increased with age and was significantly greater in those older than 65-years-old with comorbidities.3
Children, however, have been relatively spared from the ARDS-like syndrome contributing to high mortality in adults. During the initial phase of the pandemic in the United States, when testing was reserved for symptomatic patients, only 2% of confirmed COVID-19 cases were among those less than 18-years-old.5 Infants less than 1-year-old accounted for the largest percentage of hospitalizations within this group, and a recent case series suggested these febrile infants had only mild clinical symptoms, no serious outcomes, and did not require mechanical ventilation or intensive care during hospitalization.6 One rare and serious complication of COVID-19 which has been identified in pediatric patients is the multisystem inflammatory syndrome in children (MIS-C). Below are case descriptions of several children who presented with MIS-C.
Case 1
A previously healthy, vaccinated 23-month-old female presents with two days of fever and rash. She has had decreased solid food intake, but has been drinking fluids and has good urine output. Her mother had tested positive for SARS-CoV-2 four weeks ago, but never required hospitalization. On exam, the patient is crying with tears and has no focal findings. Her vital signs are all within normal limits. She is discharged home with a diagnosis of viral illness. She returns 2 days later with continued fevers and rash and now has red eyes and swollen hands and feet. Her temperature is 39.2˚C and her vitals are otherwise unremarkable. Her exam is notable for bilateral, nonpurulent bulbar conjunctivitis, cracked red lips, and a singular palpable 1.5 cm cervical lymph node.
Case 2
A previously healthy 9-year-old boy presents with five days of fever. In the past three days, he has had abdominal pain complicated by several episodes of nonbilious emesis and nonbloody diarrhea. Review of systems is also notable for decreased urine output over the preceding 24 hours. He lives with his grandmother, who was recently admitted to the hospital for COVID-19, but has subsequently recovered. On exam, he is in no acute distress and has normal perfusion with a nontender abdomen. His vital signs reveal the patient is febrile (38.8˚C), tachycardic (135 beats/min), tachypneic (26 breaths/min), and hypotensive (69/32).
Resolution of these cases will be described at the end of this article.
CLINICAL FEATURES Children and young adults are uniquely susceptible to inflammatory and vasculitic complications of SARS-CoV-2. The severity of the inflammation extends over a wide spectrum. Patients may present with erythematous, violaceous, or purpuric macules on their digits, labeled “COVID toes,” that suggest an isolated vasculitis (Figure 1).7,8 This is a benign entity and a dermatologic hallmark of COVID that does not require any specific treatment when in isolation. However, SARS-CoV-2 can cause MIS-C, the more extensive and systemic syndrome unique to the pediatric population.9

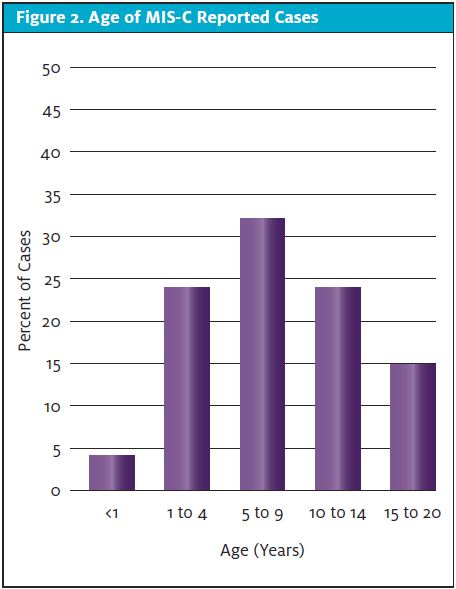
MIS-C is a postviral inflammatory process rather than an active infection. SARS-CoV-2 PCR testing is commonly negative and antibody testing is positive at the time of presentation.5,9 As evident in early reports from other countries, patients present with Kawasaki-like symptoms yet with greater cardiogenic involvement often requiring vasopressor support.10,11 MIS-C generated significant media coverage mostly because of its novel clinical presentation, its rapid appearance on the scene, and because it was previously believed that children were not significantly affected by the virus. The CDC has published, as of September 3, 2020, that there have been 792 confirmed cases of MIS-C in the U.S., with 16 deaths. Unlike primary COVID illness, which affected mostly older children, the average age of children with MIS-C is 8 years, but the age distribution is broad and bell shaped (Figure 2). Additionally, more than 70% of reported cases have occurred in children who are Hispanic/Latino or non-Hispanic black.12
RECOGNITION
It is essential to recognize signs of possible MIS-C patients; however, this is difficult because the initial symptoms occur in previously healthy patients13 and may be similar to other viral syndromes. Recent reports show that all patients present with fever. Common symptoms are gastrointestinal (abdominal pain, diarrhea, or vomiting [53%-100%]), rash (52%-76%), and conjunctivitis (45%-81%). Other concerning symptoms included neurologic (headache, visual changes, irritability, stiff neck [26%-86%]), oral mucous membrane involvement (29%-76%), and skin desquamation (18%-19%). While patients can have a neutrophil-predominant leukopenia, MIS-C patients commonly demonstrate a significant inflammatory response, with high C-reactive protein (median 200-229mg/L; normal 0.0-8.0mg/L) and ferritin (610-648 ng/mL; normal 15-200 ng/mL) values. Many patients also have direct cardiac involvement, made evident by elevated pro-BNP (78%-88% of patients) and troponin (68%-82%) levels.5,14-17 Patients with abnormal echocardiograms were diagnosed with left ventricular dysfunction (approximately 31%-35%) or coronary artery prominence (41%) or dilatation (22-76%).15-17
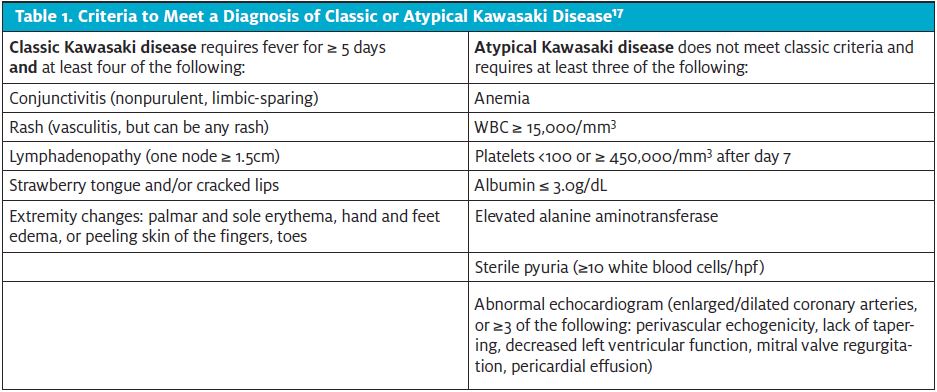
MIS-C patients appear to be loosely categorized into three nonmutually exclusive categories. They can have fever and signs of inflammation (40%); meet classic or incomplete Kawasaki criteria, depending on their lab results and/or a finding of coronary artery dilatation (Table 1); or develop a toxic shock syndrome-like picture (47%-76%).15-17
Long-term outcome data for these patients are limited, and any cardiac or coronary artery consequences will require further studies and analysis over the next months and years. A review of patients hospitalized for MIS-C in the United Kingdom noted 50% of admitted patients required admission to the pediatric critical care unit, with nearly half requiring mechanical ventilation (43%) or inotropic support (47%). A small number of those patients required extracorporeal membrane oxygenation (5%).15 In New York cohorts, those who required mechanical ventilation were primarily intubated for hemodynamic instability, not respiratory concerns.13,19 The mean hospital floor stay according to case series in New York City was approximately 4 to 7.1 days.13,15 Overall fatality rate was very low in a number of published case series (0-2%).15-17
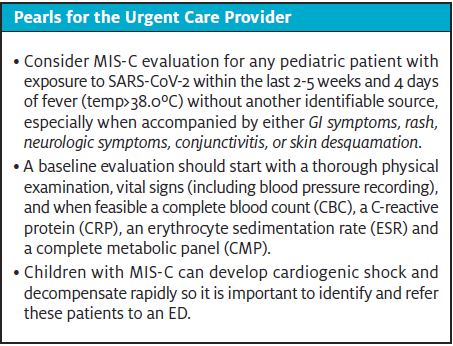
While both COVID-19 and MIS-C are still novel processes, frontline clinicians can be reassured that these are relatively rare conditions in the pediatric population. Children who do require hospitalization can be identified through careful history-taking, examination, and informed lab work. Very ill children can be quickly identified by abnormal vital signs. Pending transfer, initial management should focus on initiation of antipyretics and fluid resuscitation in the urgent care setting.
Case Resolution 1
This patient meets criteria for classic Kawasaki disease. Given her exposure to SARS-CoV-2 four weeks ago, this presentation is most consistent with MIS-C. Your patient is clinically stable with normal vital signs so she is transferred non-emergently to a nearby pediatric referral center where her lab evaluation reveals a WBC of 19, with a pronounced lymphopenia, CRP of 460 mg/L, ferritin 2071 ng/mL, troponin 13 ng/mL (normal 0.0 – 0.10 ng/mL) and pro-BNP 1958 pg/mL (normal <125 pg/mL). She is diagnosed with MIS-C and admitted to the hospital where she receives IVIG therapy and recovers uneventfully.
Case Resolution 2
This patient is acutely ill. Although he may appear well, he has tachycardia, tachypnea and hypotension. You quickly identify this patient as being in shock likely caused by MIS-C. The patient receives a saline bolus and EMS is activated to transfer the patient to the closest hospital. In the ED, his blood pressure does not improve with continued fluid resuscitation. His labs reveal moderate acute kidney injury and significant elevation in all inflammatory markers and cardiac enzymes. His echocardiogram reveals mild dilatation of the coronary arteries and slight decreased function of the left ventricle. He is admitted to the PICU on a norepinephrine infusion with a diagnosis of cardiogenic and distributive shock. His COVID antibody test is IgG positive demonstrating a recent infection. In the ICU, he receives IVIG, methylprednisolone, and low-dose aspirin as therapy for an ultimate diagnosis of MIS-C. His fever resolves within 24 hours post-IVIG administration, his blood pressure improves, and he is discharged home on hospital day 6 on low-dose aspirin and with outpatient cardiology follow-up.
Citation: Jerzewski K, Patel R, Rocker J. Multisystem inflammatory syndrome in Children (MIS-C): who should not be MISC’ed?. J Urgent Care Med. October 2020. Available at: https://www.jucm.com/multisystem-inflammatory-syndrome-in-children-mis-c-who-should-not-be-misced/
References
- Gao Z, Xu Y, Sun C, et al. A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect. Epub ahead of print. May 15, 2020.
- Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). [Published correction appears in Int J Surg. 2020;77:217. Int J Surg. 2020;76:71‐76.]
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052‐2059. [Published correction appears in doi: 10.1001/jama.2020.7681].
- Johns Hopkins University and Medical Center. COVID-19 Map. Coronavirus Resource Center. 2020. Available at: coronavirus.jhu.edu/map.html. Accessed September 11, 2020.
- Centers for Disease Control and Prevention. CDC COVID-19 Response team. Information for Pediatric Healthcare Providers. Available at:www.cdc.gov/coronavirus/2019-ncov/hcp/pediatric-hcp.html. Accessed September 11, 2020.
- Mclaren SH, Dayan PS, Fenster DB, et al. Novel coronavirus infection in febrile infants aged 60 days and younger. Pediatrics. Epub ahead of print. June 11, 2020.
- Cordoro KM, Reynolds SD, Wattier R, McCalmont TH. Clustered cases of acral perniosis: clinical features, histopathology and relationship to COVID-19. Pediatr Dermatol. Epub ahead of print. May 12, 2020.
- WHYY PBS. ‘COVID toes,’ other rashes latest possible rare virus signs. Available at: https://whyy.org/articles/covid-toes-other-rashes-latest-possible-rare-virus-signs/. Accessed September 11, 2020.
- New York State Department of Health. Childhood inflammatory disease related to COVID-19. Available at: https://coronavirus.health.ny.gov/childhood-inflammatory-disease-related-covid-19. Accessed September 11, 2020.
- Riphagen S, Gomez X, Gonzales-Martinez C, et al. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020. Epub ahead of print. May 7, 2020.
- Verdoni L, Mazza A, Gervasoni A, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. Epub ahead of print. May 13, 2020.
- Centers for Disease Control and Prevention. Multisystem inflammatory syndrome. Cases in the U.S. Available at: https://www.cdc.gov/mis-c/cases/index.html. Accessed September 11, 2020.
- Capone C, Subramony A, Sweberg T, et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory disease of childhood (MIS-C) associated with SARS-CoV-2 Infection. J Pediatr. Epub ahead of print. June 14, 2020.
- World Health Organization. Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19. Available at: www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19. Accessed September 11, 2020.
- Whittaker E, Bamford A, Kenny J, et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. Epub ahead of print. June 08, 2020.
- Cheung EW, Zachariah P, Gorelik M, et al. Multisystem inflammatory syndrome related to covid-19 in previously healthy children and adolescents in New York City. JAMA. Epub ahead of print. June 8, 2020.
- Toubiana J, Poirault C, Corsia A, et al. Kawasaki-like multisystem inflammatory syndrome in children during the Covid-19 pandemic in Paris, France: prospective observational study. BMJ. June 2020;3:369:m2094.
- Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the committee on rheumatic fever, endocarditis, and Kawasaki disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004;114(6):1708–1733.
- Morris BM, Belay E, Levin MS, et al. Webinar May 19, 2020. Multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19). Centers for Disease Control and Prevention. Available at: emergency.cdc.gov/coca/calls/2020/callinfo_051920.asp. Accessed September 11, 2020.
Author affiliations: Katie Jerzewski, MD, Cohen Children’s Medical Center, New Hyde Park, NY; Roshni Patel, MD, Cohen Children’s Medical Center, New Hyde Park, NY; Joshua Rocker MD, Cohen Children’s Medical Center, New Hyde Park, NY. The authors have no relevant financial relationships with any commercial interests.
