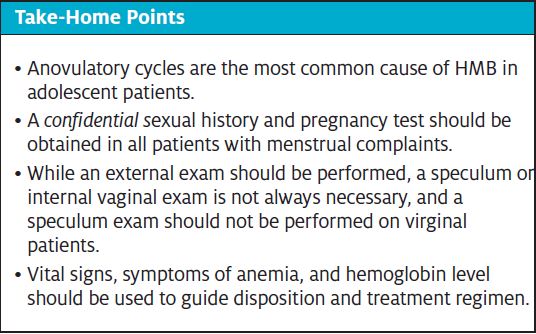
Urgent message: Anovulatory cycles are the most common cause of heavy menstrual bleeding (HMB) in adolescent patients. Just as with adult patients in the urgent care setting, it is most important to identify unstable patients and those with life-threatening causes for HMB.
Shikha Nigam, MD, MPH and Amy Pattishall, MD
Case Presentation
A 14-year-old female presents with 6 weeks of menstrual bleeding. Her cycles are irregular but she generally has 4 to 6 weeks of bleeding, followed by 4 weeks before her next menstrual cycle. She has heavy flow and often has overflow despite simultaneous use of tampons and pads. She experiences occasional headaches, shortness of breath, and exhaustion, though continues to be active in sports. Menarche was at age 11 and has been irregular with the cycle most recently as described above.
Vital signs are as follows:
- HR 115
- BP 130/69
- RR 18
- SpO2 100% on room air, afebrile
She is well-appearing, alert, and in no acute distress. Her physical exam is notable for a 2/6 systolic ejection murmur, and pale conjunctiva, buccal mucosa, and palms. Abdomen is soft, nontender, and with no hepatosplenomegaly. GU exam showed copious blood from vaginal area, with stage 5 sexual maturity rating (SMR), no internal exam was performed. Her orthostatic vital signs were positive.
Introduction
Abnormal uterine bleeding (AUB) is common in adolescent patients in the years after menarche. Heavy menstrual bleeding (HMB), a type of AUB, is defined as excessive menstrual blood loss interfering with the woman’s physical, emotional, social, and material quality of life, and occurring alone or in combination with other symptoms.1 More quantitatively, HMB is defined as experiencing menses for more than 7 days, using more than seven pads or tampons (normal strength) per day, or blood loss of >80 mL per cycle.1,2
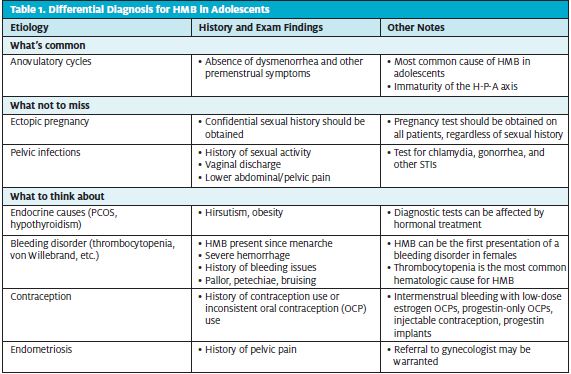
Nearly 40% of adolescents experience HMB.3 HMB can be draining and aggravating, and even life-threatening to patients, and presents a complex differential for providers (Table 1). Just as with adult patients in the urgent care setting, it is most important to identify unstable patients and those with life-threatening causes for HMB. Specific considerations in evaluating adolescent patients with HMB will be discussed in this review.
History and Physical Exam
When performing the history, pertinent questions will help determine the severity and etiology of the bleeding. Questions about age of menarche and regularity of cycles can help determine if cycles are anovulatory. A confidential sexual history should be obtained in adolescent patients, including any history of pregnancy, sexually transmitted infections (STIs) and contraceptive use. Symptoms of anemia, including fatigue, pica, pallor, shortness of breath, or palpitations, should be assessed.4 A medication history can reveal use of hormonal or anticoagulation medications.
The following questions, based on a screening tool for bleeding disorders which was validated for women ages 18 to 50, can be helpful in adolescent patients.5 This is especially important if a patient has heavy menstrual bleeding starting at menarche, when laboratory evaluation for bleeding disorder should be considered.
- On average, does your period last 7 or more days?
- Do you experience flooding or overflow bleeding through tampons or pads?
- Do you need to change your pad/tampon more often than every 1-2 hours?
- Do you have any history of anemia requiring treatment (blood transfusion, iron supplementation)?
- Is there any family history of bleeding disorders?
- Do you have any history of excessive bleeding with dental procedures, miscarriages, or birth?
The physical exam should first assess for severe anemia or hypovolemia. Vital signs may show tachycardia, hypotension, or tachypnea.4 Orthostatic vital signs should be obtained; if positive, they may assist in a diagnosis of hypovolemia. Weight and BMI may also assist in identifying potential etiology. Skin exam may reveal pallor, bruising, a petechial rash, or decreased skin turgor.5 Eyes may show conjunctival pallor. Cardiac exam should be done to assess for a murmur. The neck should be palpated to assess for thyroid size. The abdomen should be examined for distension, striae, any masses, tenderness, and hepatosplenomegaly.
On genitourinary exam, a speculum exam is often not needed, and should not be performed on virginal patients. However, an external genitourinary exam is important to evaluate sexual maturity, extent of bleeding, signs of trauma, presence of external vaginal lesions, and vaginal discharge.1 A bimanual exam should also be performed to evaluate for vaginal foreign bodies, pelvic mass, or PID.1 Though pregnancy and ectopic pregnancy may be the cause of HMB, evaluating the SMR may give you clues to an immature hypothalamic pituitary ovarian axis.
Work-Up
If the patient is stable and your facility is capable of performing them, a number of labs are useful in identifying etiology and treating the patient.
Pregnancy, though less common than in adults, should always be on the differential. A pregnancy test is critical to evaluate for complications of pregnancy such as miscarriage or ectopic pregnancy. A CBC is important to evaluate extent of anemia and for thrombocytopenia.
Other potentially useful labs include coagulation studies, fibrinogen, ferritin, and TIBC.1 If transfusion is warranted, a type and screen would need to be obtained. Coagulation studies can help identify clotting disorders, platelet disorders, or liver dysfunction. While unlikely to impact initial treatment, thyroid and von Willebrand studies can identify possible etiologies of HMB.
Studies that may be useful in identifying an endocrine etiology (such as polycystic ovarian syndrome, or immature hypothalamic-pituitary-ovarian axis) are FSH, LH, estrogen, prolactin, 17 hydroxyprogesterone, and testosterone.1 Because these labs may be affected by treatment with hormonal contraceptives, it is helpful to obtain these labs early, though it should not delay treatment.
If warranted ana available, ultrasound of the ovaries and uterus may support diagnosis of polycystic ovarian syndrome (PCOS), show structural abnormalities, and assess the thickness of the endometrium.1
Treatment
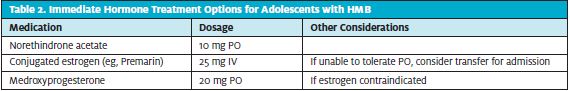
Patients who are hemodynamically unstable should receive rapid volume resuscitation and transfusion. These patients will likely require transfer to higher level of care for further evaluation and management. Treatment is aimed at stopping the bleeding and correcting anemia. Specific treatment regimens vary depending on level of anemia and patient symptoms, but typically consist of high-dose estrogen (with or without progestin) to stop the bleeding, followed by a taper of a combination estrogen/progesterone. In general, patients who have symptomatic anemia or an Hb less than 7 should be transferred for IV estrogen and transfusion.
Medications that can be used to stop bleeding in the urgent care setting are summarized in Table 2. Many patients can be managed on an outpatient basis; examples of treatment options are presented in Table 3. If estrogen is contraindicated then medroxyprogesterone is preferred. Contraindications to estrogen therapy including a history of deep vein thrombosis or pulmonary embolism, lupus, Kawasaki disease, nephrotic syndrome, or cardiac conditions necessitating aspirin or anticoagulation therapy.1
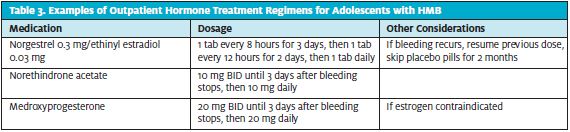
In addition to stopping the bleeding, it is important to support hematopoiesis. Iron supplementation with 65 mg elemental iron is beneficial, as iron stores may be depleted. A stool softener should be considered to alleviate the constipation side effect of iron supplementation. An antacid and antiemetic may help with GI side effects caused by estrogen therapy. Follow-up with a gynecologist or hematologist is important for long-term care.
Resolution
The patient had microcytic anemia (Hb 4.6, MCV 54) and was transfused two units of PRBCs. Iron studies were indicative of iron deficiency and she was started on iron supplementation. There were no findings of PCOS, von Willebrand disease, or anatomic etiology for her HMB. Her HMB was determined to be due to an immature hormonal axis and anovulatory cycles. She was given IV estrogen. Bleeding was controlled while inpatient and she was discharged with oral hormonal control. She was lost to follow-up and presented less than 2 years later with similar complaints and required repeat transfusion.
Conclusion
Heavy menstrual bleeding is a common issue among adolescents. It is important to assess patients for anemia and acute bleeding. While determining the etiology is not the primary objective in the urgent care setting, it is important to understand the differential to identify potentially life-threatening causes and to obtain tests that can be altered by treatment. Anovulatory cycles are the most common cause of heavy menstrual bleeding in adolescents, but bleeding disorders and endocrine disorders such as PCOS are also important to consider. Taking a confidential sexual history and obtaining a pregnancy test are essential in evaluating for pregnancy related causes and STIs. It is also vital to identify patients who need transfusion or further work-up that is outside the capability of the urgent care center. Treatment focuses primarily on arresting the menstrual bleeding to prevent anemia if it has not already occurred. The importance of follow-up should be stressed to the patient and family, as HMB is likely to recur if therapy is stopped without guidance.
References
- Haamid F, Sass AE, Dietrich JE. Heavy menstrual bleeding in adolescents. J Pediatr Adolesc Gynecol. 2017;30(3):335-340.
- The American College of Obstetricians and Gynologists Committee on Adolescent Health Care. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Committee Opinion. Number 651; December 2015. Available at: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2015/12/menstruation-in-girls-and-adolescents-using-the-menstrual-cycle-as-a-vital-sign. Accessed June 7, 2021.
- Graham R-A, Davis J A-M. The adolescent with menorrhagia: diagnostic approach to a suspected bleeding disorder. Pediatr Rev. 2018;39(12):588-600.
- Janus J, Moerschel SK. Evaluation of anemia in children. Am Fam Physician. 2010;81(12):1462-1471.
- Philipp CS, Faiz A, Heit JA. Evaluation of a screening tool for bleeding disorders in a US multisite cohort of women with menorrhagia. Am J Obstet Gynecol. 2011;204(3):209.e1-7.
Author affiliations: Shikha Nigam, MD, MPH, Division of Pediatric Emergency Medicine at Emory University School of Medicine; Children’s Healthcare of Atlanta. Amy Pattishall, MD, Division of Pediatric Emergency Medicine at Emory University School of Medicine; Children’s Healthcare of Atlanta.
