Urgent message: Urgent care providers need to be vigilant for more than acute coronary syndrome, pulmonary embolism, and thoracic aortic dissection when patients present with chest pain—such as this 20-year-old who developed pneumomediastinum while smoking marijuana.
Xiangyang Jiao, MD
Case Presentation
A 20-year-old female presented to urgent care for pleuritic chest pain and shortness of breath for about 2 hours. The chest pain was located in the upper and mid chest, was dull, pressure like, mild, and radiated to the right side of the neck. The chest pain was not improved with acetaminophen. She worked as a server at the nearby sports bar and denied any injury or any unusual mental stress. No cough, palpitations, nausea, diaphoresis. No recent travel or any illness, no known exposure to COVID. PMH negative except for anxiety. SH: Occasional tobacco use and smokes marijuana 3-4 times a week.
Vitals BP 120/76, HR 72, R 12, Pulse O2 98%. She appeared comfortable without distress, spoke long, full sentences. Heart and lung auscultation were normal, and no leg tenderness or any swelling.
Differential Diagnosis
The differential diagnoses include anxiety, gastroesophageal reflux, musculoskeletal strain, pulmonary embolism, and pneumothorax.
Testing
As part of our standard chest pain evaluation protocol, EKG and CXR were ordered. EKG was normal sinus rhythm, no ST-T changes.
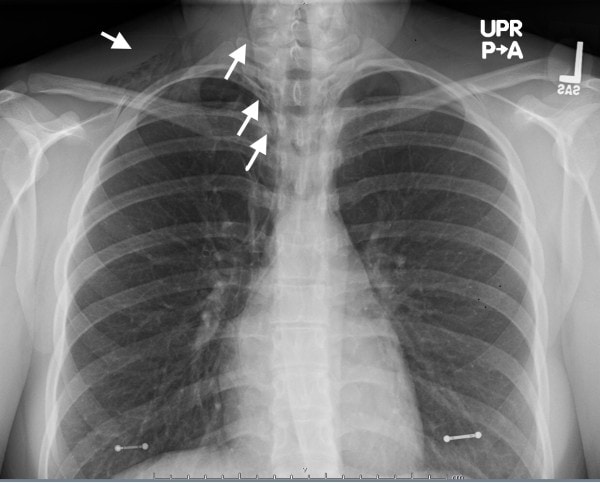
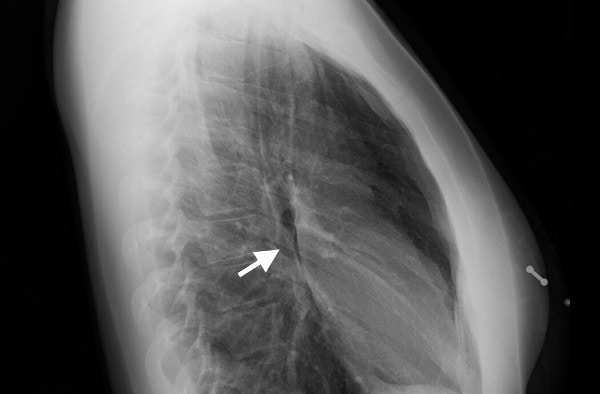
The chest x-ray showed a lucency along the right superior mediastinum and medial right upper lobe, as well as overlying the right lung apex and base of right neck (Figure 1 and Figure 2) consistent with spontaneous pneumomediastinum.
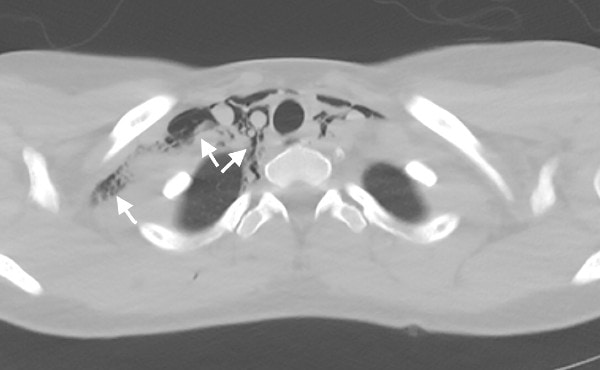
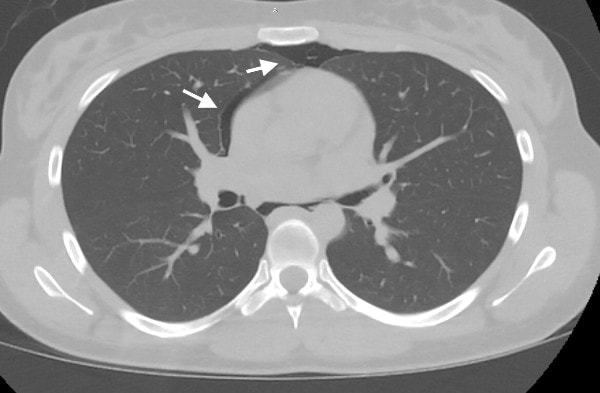
Urgent Care Disposition
The patient was sent to ED for further evaluation. CT of chest and esophagram with oral contrast confirmed moderate pneumomediastinum without pneumothorax or esophagus perforation (Figures 3 and 4). Detailed history suggested its cause from barotrauma from marijuana use (inhalation either through a high-resistance smoking apparatus or forced exhalation against a closed glottis). Patient was observed in hospital for 48 hours, pneumomediastinum was gradually resolving on repeat chest x-ray and patient was asymptomatic upon discharge.
Discussion
Pneumomediastinum, also called mediastinal emphysema, is a rare condition where free air is leaked into mediastinal space from either respiratory or GI tract. It is usually associated with physical trauma (including excessive coughing, vomiting, mechanical ventilation) or underlying chronic conditions (asthma, interstitial lung disease, COPD, bronchiectasis, lung cysts, lung malignancy). Spontaneous pneumomediastinum (SPM) may occur in otherwise healthy subjects without identifiable causative factors,1 though after detail and careful history taking, many of initially diagnosed SPM are found to be caused by substance inhalation,1-3 as in this case.
Presenting symptoms of SPM may be acute or have a subacute onset presentation . Retrosternal chest pressure or pain and/or mild dyspnea are most common, followed by cough, neck pain, back pain, sore throat. If large amount air is leaked in a rapid pace, or with concomitant pneumothorax (reportedly in 40% of all pneumomediastinum), palpitation, anxiety, emesis, dysphagia, or tachypnea can also occur. Physical exam is often normal, with crepitus in the shoulder region or chest wall identifiable in less than a quarter of cases, and the pathognomonic Hamman’s sign (a crunch or click sound on auscultation over the cardiac apex and the left sternal border synchronous with the heartbeat), indicating air leaked into pericardial space, rarely present.1
Diagnosis can be established with a plain chest x-ray. Positive up to 90% of the time, this may show lucent streaks, air bubbles outlining mediastinal structures, or visible mediastinal pleura.1 Subsequent chest CT is needed to assess the extent of pneumomediastinum, concomitant pneumothorax, pneumopericardium, as well as to identify causative factors. Unless there is underlying risk, other diagnostic tests, like bronchoscopy, endoscopy, mediastinal ultrasound, and extensive blood work are often not needed.
Management of isolated SPM is generally supportive. In severe cases, needle or chest tube decompression may be needed.
Take-Home Points
- Chest pain and or dyspnea require consideration of forced inspiration or expiration at onset, such as with smoking marijuana.
- Maintain a low threshold for EKG and chest x-ray.
- Pneumothorax and pneumomediastinum presentations can be subtle.
- Pneumomediastinum is typically managed symptomatically.
References
- Kouritas VK, Papagiannopoulos K, Lazaridis G, et al. Pneumomediastinum. J Thorac Dis. 2015;7(Suppl 1):S44–S49.
- Perna V, Vilà E, Guelbenzuj JJ, et al. Pneumomediastinum: is this really a benign entity when it can be considered as spontaneous? Our experience in 47 adult patients. Eur J Cardiothorac Surg. 2010;37:573-575.
- Weiss ZF, Gore S, Foderaro A. Pneumomediastinum in marijuana users: a retrospective review of 14 cases. BMJ Open Respir Res. 2019;6(1):e000391.
Author affiliations: Xiangyang Jiao, MD, OhioHealth Urgent Care. The author has no relevant financial relationships with any commercial interests.

