Urgent message: Referrals to the ED for CT scans were reduced when urgent care providers combined clinical judgement with EEG-based structural injury biomarker results. Such reductions could relieve the burden of referrals to EDs, minimize unnecessary radiation risk, yield better patient experience, and foster to potential cost savings.
Tanvir Dara MD, FACEP; Elizabeth McCarty MD; Paul Meredith MD; Robert Mooney MD; David Porzio MD; and Alvaro Zeballos MD
Citation: Dara T, McCarty E, Meredith P, Mooney R, Porzio D, Zeballos A. Urgent care centers can reduce ed referrals for CT scans in mild head injury with integration of brain activity biomarker. J Urgent Care Med. 2022;16(9):37-40.
Abstract
Background
Urgent care centers (UCCs) have expanded rapidly, to the point that they now outnumber emergency rooms. Though urgent care is an appropriate setting for initial assessment of mild head injury, many UCCs continue to refer a large percentage of head-injured patients to the ED for CT scanning. Ultimately, most of these are deemed unnecessary. Tools are needed to empower urgent care providers to reduce the rate of mild traumatic head injury referrals to the ED.
Objective
Evaluate the potential to reduce UCC referrals to the ED for head CT scans based on cases entered into a registry of evaluations performed including use of a brain activity-based biomarker (structural injury classifier [SIC]).
Methods
This was a retrospective study of 963 patients entered into the registry from 24 participating UCCs between June 2017 and September 2020, in whom assessments included the SIC evaluation, using the BrainScope FDA cleared medical device. The percent reduction in ED referrals for CT when using SIC alone, and when integrated with clinical judgement, are compared to three standard referral rates from UCC (50%, 75%, 100%).
Results
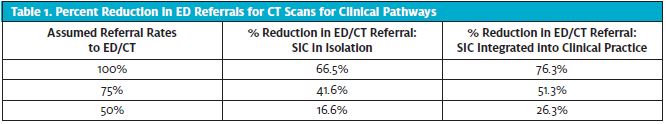
For 100%, 75%, and 50% standard referral rates, reductions of 66.5%, 41.6%, and 16.6%, respectively, were seen using the SIC alone. When using both SIC and clinical judgment to make referrals, rates were reduced by 76.3%, 51.3%, and 26.3%, respectively. In addition, performance relative to CT findings based for clinical use integrating SIC with clinical judgment resulted in 100% sensitivity, 77.3% specificity, 32.9% PPV, and 100% NPV.
Conclusion
Significant potential reduction of referrals to the ED from UCC were seen compared to each of the standard referral rates when SIC -EEG-based biomarker was integrated into the initial assessment of head-injured patients. High performance was obtained using SIC and clinical judgment, with 100% sensitivity and 100% NPV compared to CT.
INTRODUCTION
The number of urgent care centers (UCCs) is expanding rapidly, to the extent that they now outnumber emergency rooms (EDs) by a wide margin. As such, UCCs have the potential to significantly impact initial assessment of patients with mild head injuries. However, standard assessment capabilities in UCCs result in a large percentage of head-injured patients being referred to the ED for CT scanning.
In a study of 3,232 patients transferred from urgent care to the ED, Zitek and colleagues reported that most of the patient transfers were deemed unnecessary, resulting in discharge from the ED.1 Further, of the estimated 4.8 million people who are evaluated in the ED for a traumatic brain injury (TBI), more than 80% received a CT scan; of these, 91% are found the be negative.2
Researchers have reported extremely high accuracy in the objective identification of likelihood of traumatic structural brain injury (bleed of 1 cc or greater) using quantitative EEG (qEEG) as input to classifier algorithms derived using machine learning (ML) methods.3 Use of this structural injury classifier (SIC) as an electrophysiological (EEG) biomarker of brain injury in the ED has been demonstrated to potentially reduce unnecessary CT scans by more than 30%.4 The use of an EEG-based biomarker could likewise aid in reduction of unnecessary referrals from the UCC to the ED for CT, significantly impacting care of head-injured patients and helping to reduce unnecessary crowding of EDs.
This retrospective study evaluates the potential to reduce UCC referrals to the ED for head CT scans based on the cases entered into a registry from evaluations performed using the SIC.
DATA SOURCE
This report is based on registry data which contain deidentified information about the assessments of head injury patients performed at 24 participating UCCs between June 2017 and September 2020. Data were collected on the BrainScope medical device platform using an EEG-based SIC to assess the likelihood of CT positive findings. Patient demographics, output of the SIC classifier, and findings of the CT scan read by a site radiologist or neuroradiologist were entered into the registry for further analysis. Patient data were collected in accordance with site clinical practice and deidentified for entry in the registry. Since the data provided to the registry were not part of any research activity and contained no personal health information, the participating UCCs did not require IRB review.
METHODS
The SIC is derived from 1-2 minutes of artifact-free eyes-closed EEG data acquired from a frontal montage (including frontal and frontotemporal scalp regions) and selected associate clinical risk factors often associated with TBI. Details of the derivation of the classifier and its independent validation are described by Hanley, et al.3 Results of the SIC biomarker are reported as positive (likely brain injury present visible on head CT; consider further evaluation, including advanced neuroimaging or CT scan), equivocal (consider further evaluation or observation, identifies patients close to the positive threshold, much like used in medicine today for “pre-diabetic”), or negative (likely no brain injury visible on head CT). For purposes of the present retrospective study, an equivocal SIC result was treated as a positive result.
Due to the absence of a standard protocol for triaging head injured patients in the UCC environment, current referral rates to the ED for a possible CT scan from a UCC vary by site and provider. Therefore, in this study, comparisons were made assuming rates of referral rates of 100%, 75%, to as low as 50%, with actual rates likely to be at the upper end of this range. All UCC providers used the FDA cleared BrainScope medical device as an adjunct to their usual clinical assessment and ED referral decisions for CT scans.
The analyses will include comparisons between results from clinical assessment with integration of the SIC with each of the assumed referral rates. In addition, analyses will be repeated for the comparison between assumed referral rates and the SIC results had they been used in isolation (without clinical integration). It is noted that cases that were not sent to CT from the UCC or for whom no CT was ordered in the ED were deemed CT, and cases with “unknown CT results” were excluded from analyses.
RESULTS
The patient population consisted of 963 patients from 24 urgent care centers. Patients were between the ages of 18 and 85 (mean 36.2 years, SD=16.6), 39.3% male, and were evaluated within 72 hours of injury (mean 20.1 hours). The two most common mechanisms of injury were fall-related (33.8 %), and motor vehicle accident (22.4%).
When UC providers integrated the SIC results with their clinical assessment, only 23.7% (228 of 963) of the patients were sent to the ED for a CT. Had SIC results been used in isolation (without clinical integration) 33.4 % (322 of 963 patients) of patients would have been referred to the ED for CT. Performance metrics were computed relative to CT findings for traumatic intracranial brain injuries. Based on actual clinical use (SIC integrated with clinical judgment), performance resulted in 100% (13/13) sensitivity, 77.3% (735/950) specificity, 32.9% PPV*, and 100% NPV*. Performance metrics were computed relative to CT findings of traumatic brain injuries.
Not all of the patients who were SIC+ or equivocal were sent to the ED for a CT scan. The majority of these patients not sent to the ED had equivocal SIC results. Since BrainScope equivocal results indicate patients who were close to the positive result threshold, the addition of clinical judgment to the BrainScope finding can be seen.
Table 1 shows the percent reduction in ED referrals for CT scans had SIC results been used in isolation (middle column), and when integrated into the providers clinical assessment (left column), compared with a range of different estimated referral rates (100%, 75%, or 50%) under current clinical practice.
DISCUSSION
These data demonstrate that use of an EEG-based biomarker (SIC) integrated into the UCC head injury workflow can aid in significantly reducing UCC referrals to the ED for CT. The divergence rate was shown to be as high as 76.3% when integrating BrainScope into clinical workflow assuming that all patients would have been previously sent the ED, and 51.3% with an assumption of 75% previously being sent.
Even at the lowest estimated rate of 50% previously being sent to the ED for head CT scan, reduction would still be 26.3%. Although significant reductions were seen when SIC was used in isolation, the highest reduction rates were seen when providers integrated SIC with their clinical judgement. All demonstrate a significant impact on unnecessary ED referrals from UCC when using the additional information provided by integrating the SIC.
LIMITATIONS
A limitation of this study was there was no follow-ups on patients after they we sent home from the UCC or the ED to ensure they did not deteriorate or require further neuroimaging. This is currently being investigated in an ongoing study.
Another limitation was due to the small number of CT+ cases in the sample and thus, the 100% sensitivity reported should be interpretated with caution. This is also representative of the UCC population; the majority of CT-positive patients may not go to a UCC for initial care of a suspected head injury. However, a published paper in an ED population has replicated this finding in a larger group.4
Finally, the highest accuracy was found when comparing the SIC with the clinical judgement to CT results. Information as to how the SIC result was incorporated into the clinical assessment of head injured patients would be helpful to understand how to optimize the UCC head injury triage.
CONCLUSION
There is consensus that the current referral practices to the ED for a CT scan from the UCC need to be reevaluated.5 Patients with mild head injuries need to be categorized into those who need to be transferred to a higher level of care in the ED and those who can be managed in the UCC environment. Integrating the BrainScope SIC into head injury triage in the UCC environment can provide objective data to help providers with the referral decision.
The utility of the SIC biomarker extends from the UCC to the ED environment, with the ability to aid in the reduction of the number of referrals to the EDs from the UCC. Access to the SIC results, may facilitate more objective and reliable decision pathways for the UCC provider, with improved outcomes and better use of resources.
In this registry population of >950 patients, the SIC was demonstrated to have 100% sensitivity and NPV. Significant reduction in UCC referrals to the ED for CT scans was observed when UCC providers combined clinical judgement with the structural injury biomarker result. Such reductions (as high as 76.3%) could relieve the referral burden to EDs, minimize unnecessary radiation risk, yield better patient experience, and lead to potential cost savings. More widespread use of such an EEG-based biomarker as part of head injury assessment can help the UCC provider evaluate and treat a greater proportion of these patients, and could aid in making more confident referrals to the ED.
Acknowledgements
All authors have no competing financial interests to disclose. The UCCs were only reimbursed by BrainScope at a fair market value commensurate with their time and effort in entering the deidentified patient data into the registry. The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Korley F, Kelen G, Jones C, Diaz-Arrastia R. Emergency department evaluation of traumatic brain injury in the US, 2009-2010. J Head Trauma Rehabil. 2016;31(6):379-87.
- Hanley D, Prichep LS, Bazarian J, et al. Emergency department triage of traumatic head injury using brain electrical activity biomarkers: a multisite prospective observational validation trial. Acad Emerg Med. 2017; 24(5):617-627.
- Naunheim R, Konstantinovic Koscso M, Poirier R. Reduction in unnecessary CT scans for head-injury in the emergency department using an FDA cleared device. Am J Emerg Med. 2019;37(10):1987-1988.
- Siegfried I, Jacobs J, Olympia, RP. Adult emergency department referrals from urgent care centers. Am J Emerg Med. 2019;37(10):1949-1954. 5.
- Zitek T, Tanone T, Amos A, et al. Most transfers from urgent care centers to emergency departments are discharge and many are unnecessary. J Emerg Med. 2018; 54(6):882-888.
Author affiliations: Tanvir Dara MD,FACEP, WellNow Urgent Care, Buffalo, NY. Elizabeth McCarty, MD, Mercy Urgent Care/Mercy Occupational Medicine, Asheville, NC. Paul Meredith MD, HealthCARE Express, Texarkana, TX. Robert Mooney MD, STAT MED Urgent Care, Concord, CA. David Porzio MD, Marque Medical, Irvine, CA. Alvaro Zeballos MD, BetterMed Urgent Care, Richmond, VA. The authors have not relevant financial relationships with any commercial interests.
