Urgent Message: With hyperabduction and hyperextension of the thumb, the ulnar collateral ligament may be stretched or torn, or may avulse a segment of bone from its insertion point. Radiographic imaging of suspected “gamekeeper’s thumb” must be obtained to evaluate for an associated fracture, which may change the decision for conservative vs surgical management.
Omar Jafry, MS-3; W. Bradley Strauch, MD
Citation: Jafry O, Strauch WB. Urgent Care Evaluation and Management Of Injury to the Ulnar Collateral Ligament of the Thumb (‘Gamekeepers Thumb’). J Urgent Care Med. 2024; 18(9):26-29
Editor’s Note: While the images presented here are authentic, the patient case scenarios are hypothetical.
Clinical Scenario
A 32-year-old man presents to the urgent care with pain at the metacarpal-phalangeal (MCP) joint of the thumb, sustained the previous week when he was skiing and fell with hyperextension of the thumb. The pain is worse with range of motion, but he denies any numbness, wounds, wrist pain, or other injuries.
Physical exam reveals a hand that is normal in appearance without evidence of swelling, erythema, or wounds. Palpation of the MCP joint of the right thumb reveals pain on the medial (ulnar) aspect and with valgus testing. Laxity of the right thumb is present when comparing range of motion between both thumbs, and there is a defined endpoint. There is no pain with palpation of the interphalangeal joint or over the anatomical snuff box. Neurovascular is intact with 2+ radial pulse.
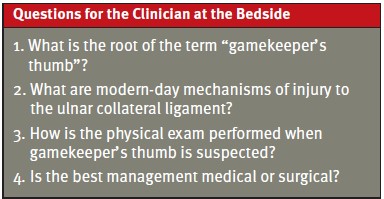
A thumb x-ray is performed, which shows an avulsion fracture of the proximal ulnar aspect of the proximal phalanx or “gamekeeper’s fracture.”
Discussion Of The Evaluation And Management Of ‘Gamekeeper’s Thumb’ (also ‘Skier’s Thumb’)
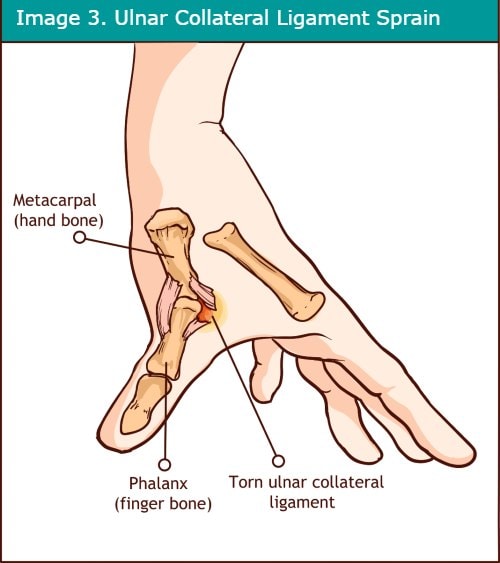
The typical mechanism of injury of the ulnar collateral ligament (UCL) of the thumb is by forced hyperextension and hyperabduction of the thumb. With severe hyperextension, the UCL can be torn or may avulse bone at the insertion of the UCL at the ulnar aspect of the proximal phalanx base (Image 1, 2). The moniker for this injury, “gamekeeper’s thumb,” originated from the injuries of gamekeepers who would develop chronic degeneration of the UCL of the MCP when twisting the necks of fowl and small game.
Today, a UCL injury commonly occurs when a skier falls, and the thumb undergoes hyperabduction and hyperextension with a ski pole in hand (“skier’s thumb”). This injury can also occur in other sports including rugby, soccer, or basketball.[1]
Understanding the Anatomy
The bones of the thumb are held in place by ulnar and radial collateral ligaments located on the ulnar and radial aspect of each phalanx, respectively. With hyperabduction and hyperextension of the thumb, the UCL may be stretched, torn, or may avulse a segment of bone from its insertion at the proximal aspect of the proximal phalanx (Image 3). The ulnar collateral ligament originates at the head of the metacarpal bone. The most common site of avulsion is at the distal aspect of the UCL (where it attaches to the base of the proximal phalanx),[2] which is called a gamekeeper’s fracture.
History
Knowing the mechanism of injury is the most important element of the history; the first step is to inquire about a fall with a mechanism of hyperabduction and hyperextension of the thumb.2 Repetitive strain on the UCL can also cause strain or tear at its insertion sites. One telltale sign of a UCL injury is pain localized to the ulnar aspect of the MCP joint worsened with range of motion.
Physical Exam
First, assess the integrity of the skin and check for swelling. Generally, the area of greatest pain with palpation is over the ulnar aspect of the MCP joint. Also, make sure to check the radial collateral ligament of the thumb and the extensor and flexor tendons of the thumb MCP and IP joint for better localization. The next step is to examine the proximal and distal joints, including the anatomic snuff box, which is a triangular depression evident on the dorsal radial aspect of the wrist with extension of the thumb. Since the radial nerve and radial artery run through the snuffbox, the next step is check for neurovascular status by assessing gross sensation as well as vascular status with documentation of radial and/or ulna pulse and capillary refill of the tip of the thumb.
Checking stability of the thumb in an acute care setting is unlikely to change management and will often result in significant pain; this test can be safely deferred.1 If testing is done, use a valgus stress test (radial deviation of the MCP joint) to check for laxity. Note that there are various degrees of laxity in finger joints, so comparison to the opposite side may be helpful. If performing stress testing of the joint, make sure to do so after x-ray results are available to ensure there is not an avulsion fracture.
Finally, assess wrist and finger range of motion and strength testing bilaterally (thumb stability, grip strength, and pinch strength). Usually there will be weakness with resisted pinch testing.
Imaging
Radiographic imaging of suspected gamekeeper’s thumb must be obtained to evaluate for an associated fracture, which may change the decision for conservative management vs surgical repair. However, a 3-view x-ray typically is normal if there is simply a sprain or tear of the UCL. With repetitive injury, the x-ray may show degenerative changes at the MCP joint. With UCL rupture, there is an associated bony avulsion present, occurring 20-30% of the time.[3]
Indications for Referral to the Emergency Department
Consider the following for referral to the emergency department:
- Intractable pain
- Open fracture
- Concern for other associated injury
Management In the Urgent Care
Place a thumb spica splint or orthoglass splint/brace to immobilize the thumb. If there is a concern for a complete rupture or an associated fracture, the patient should be referred to orthopedics or hand surgery.[4] With significant pain, consider a combination of acetaminophen and a non-steroidal anti-inflammatory medication (NSAID). Acetaminophen and NSAIDs can be used together, and alternating is not necessary as acetaminophen is metabolized/excreted by the liver and NSAIDS by the kidneys
If conservative management is the initial approach, advise follow-up with primary care or orthopedics/hand specialist in 5-7 days.
Indications for conservative management include:[5]
- Partial, non-displaced UCL tears
- Minimally displaced fractures
- Associated fractures without displacement
Recommendations include 4-6 weeks of immobilization with a well-fitting thumb spica brace, gamekeeper’s brace or fiberglass cast with a periodic 2-week follow-ups to assess for pain and stability.2,5 If pain has decreased with the immobilization, range of motion exercises may be initiated.2 If there is a concern the patient will require surgical intervention, orthopedic follow-up can occur in the same time span. If there is an associated fracture, more rapid follow is advisable.
Samora et al. conducted a systematic review of 14 articles, compromising 293 thumbs—with 200 acute and 93 chronic injuries—with outcomes measured over 2 years of follow-up, including pain, range of motion, key-pinch strength, and stability. Findings showed nonoperative management often failed, though there was no harm with using conservative therapy first.3
Surgical indications vary, but surgery is usually indicated for a significantly rotated and/or displaced fracture, a large displaced intra-articular fracture, a complete rupture of the UCL in an active person, persistent laxity and/or pain after a trial of immobilization, or a Stener lesion. A Stener lesion occurs when a complete UCL tear results in the interposition of the aponeurosis of the adductor pollicis muscle between the metacarpophalangeal joint and the torn UCL. Also, it is suspected when a tender nodule around the UCL is palpated during exam and there is no firm endpoint on stress testing. Surgical techniques include UCL repair and autograft UCL reconstruction for chronic injury without a significant difference between the groups; surgical management is frequently successful with a low rate of complications.5
Next Level Urgent Care Pearls
- Patients who depend upon the thumb for competitive athletics or vocation may benefit from primary referral to sports medicine/orthopedics/hand specialist instead of primary care.
- Ensure there is immobilization with a dedicated thumb spica splint, which may not be achieved with a volar or ulnar gutter splint.
- Assess the radial collateral ligament in addition to the UCL.
- If stress testing for laxity causes too much pain, an injection of lidocaine may allow for a better exam.
- Compare to the contralateral thumb as there is a significant amount of baseline laxity (which varies from person to person)
- Assess for a Stener lesion where the UCL displaces proximally and appears as a tender nodule around the UCL—note that swelling at the base of the thumb may also be from scar tissue formation.2
- Surgical therapy has a good success rate with minimal complications.4
Red Flags and Legal Pitfalls
- Injury to the UCL may be missed by inexperienced providers.
- Consider the possibility of trauma to the scaphoid, extremities, head or neck.
- Injury to the scaphoid should be assessed with palpation of the anatomic snuff box. If a scaphoid injury is suspected, immobilization of the thumb and wrist is necessary.
- Discuss conservative or surgical management.
Clinical Scenario Conclusion
The patient was placed in a Velcro thumb spica brace, NSAIDs were recommended for pain control, and the patient was referred to orthopedic hand surgeon where the pros and cons of operative treatment were discussed. The patient decided to pursue surgical management and regained full use of his thumb with no operative or postoperative complications.
Takeaway Points
- A typical mechanism of injury to the UCL is hyperabduction and hyperextension of the thumb.
- With a tear of the UCL or avulsion fracture, there will be laxity upon valgus stress testing.
- Initial management of a UCL sprain is usually conservative, though surgical management will sometimes be necessary.
- Surgical management is frequently successful with a low rate of complications.
Manuscript submitted March 5, 2024; accepted April 25, 2024.
References
- [1]. Madan SS, Pai DR, Kaur A, Dixit R. Injury to ulnar collateral ligament of thumb. Orthop Surg. 2014;6(1):1-7. doi:10.1111/os.12084
- [2]. Chang AL, Merkow DB, Bookman J, Glickel S. Thumb Metacarpophalangeal Joint Ulnar Collateral Ligament Injuries: Management and Biomechanical Evaluation. J American Academy of Orthopaedic Surgeons. 31(1):p 7-16, January 1, 2023. DOI: 10.5435/JAAOS-D-22-00112
- [3]. Samora JB, et al. Outcomes after injury to the thumb ulnar collateral ligament–a systematic review. Clin J Sport Med. 2013; 23:247-254
- [4]. Daley D, Geary M, Gaston RG. Thumb Metacarpophalangeal Ulnar and Radial Collateral Ligament Injuries. Clin Sports Med. 2020;39(2):443-455. doi:10.1016/j.csm.2019.12.003
- [5]. Giddins GE. The non-operative management of hand fractures. J Hand Surg Eur Vol. 2015;40(1):33-41. doi:10.1177/1753193414548170
Author Affiliations:. Omar Jafry, MS-3, University of Pikeville-Kentucky College of Osteopathic Medicine. W. Bradley Strauch, MD, Adena Orthopedic and Spine Institute, Chillicothe, Ohio. Authors have no relevant financial relationships with any ineligible companies.
Read More
