Urgent Message: With STI rates rising, urgent care centers have a unique opportunity to address a pressing public health need and increase patient volumes and revenue by adding STI testing services.
Citation: Ayers A. The Urgent Need for STI Testing in Urgent Care Centers. J Urgent Care Med. 2024; 18(10)39-42
Alan A. Ayers, MBA, MAcc
Globally, the World Health Organization (WHO) estimates that more than 1 million sexually transmitted infections (STIs) are acquired every day.1 Given that the majority of these infections are asymptomatic, STI testing is a crucial tool for not only detecting existing STIs but also preventing the spread to more individuals.
However, the persistent stigma surrounding STI testing creates an environment where many people feel uncomfortable getting tested—particularly at their primary care provider’s office. This, along with improvements to rapid STI testing kits and reimbursement policies, presents an development opportunity for urgent care (UC).
Given the urgency of treating and eliminating concern over an STI, urgent care is well-positioned to give patients the peace of mind they seek while rendering essential health services. As a benefit, rapid STI testing offers an alternative route for urgent care revenue generation beyond testing for and treating the “bread and butter” respiratory conditions and minor injuries.
Who is Affected?
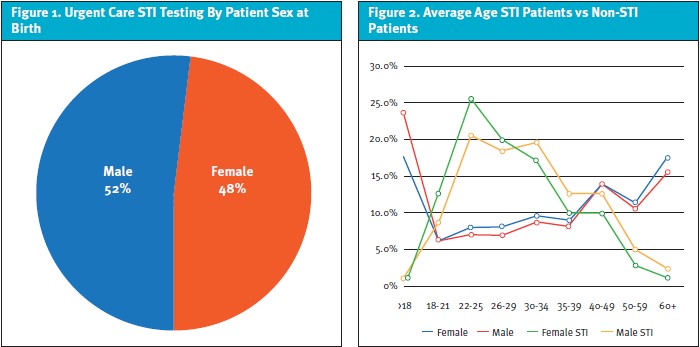
When considering the addition of STI testing in urgent care, it’s important to have a clear picture of the patient demographic that will be served. A sample of data pulled from Experity’s electronic medical record (EMR) from 2023, including over 23.3 million patient visits, sheds some light on this question. The data consists of the ICD-10 codes Z20.2 (contact with and exposure to infections with a predominantly sexual mode of transmission) and Z11.3 (encounter for screening for infections with a predominantly sexual mode of transmission).
Data from this query reveals that the typical patient seeking STI testing at urgent care is male (Figure 1). When compared to the overall urgent care population, this trend is noteworthy given that urgent visits skew toward females, who present in 57% of visits for all conditions. Notably, male STI patients also tend to be slightly older than their female counterparts despite there being little age difference between genders for non-STI patients (Figure 2).
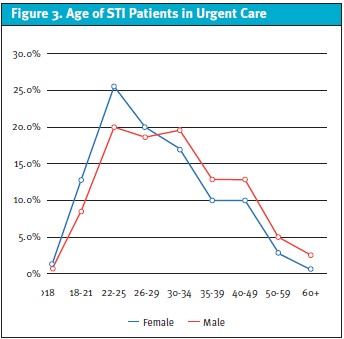
Among adult patients visiting UC, those seeking STI testing are most likely to fall between the ages of 22-34 years (Figure 3). The availability of STI testing could generate future loyalty and subsequent visits (including for non-STI care) by this population.
What is Tested?
While there are at least 30 known bacteria, viruses and parasites are known to be transmitted through sexual contact,1 the scope of testing at urgent care is typically limited to the most frequently presenting infections. Primarily, clinics test for gonorrhea and chlamydia as these are usually of the greatest concern to male and female patients. These 2 STIs are also most conducive to rapid PCR tests. For female patients, providers must be able to differentiate between bacterial vaginosis, trichomoniasis, and a yeast infection to ensure appropriate treatment.
It is important to note that testing for hepatitis, HIV, and syphilis is typically not ideal for most urgent cares. For one, these tests are most often sent out to a third-party lab. Delays brought on by this process mean the patient won’t know their results for some time after exposure and may not return for treatment after a positive result. Long wait times for results are a key contributor to patients lost to follow-up. Moreover, STIs like HIV and syphilis have a markedly larger impact on specific populations who may have access to community resources focused on preventing, diagnosing and treating these conditions.
Historic Challenges Limiting Urgent Care Testing
Surprisingly, despite urgent care’s positioning to “test and treat” during the COVID-19 pandemic, data reveals STI testing in urgent care is sparce. This trend underscores the respiratory-related nature of the UC business and the challenges of adding STI testing. Limited urgent care testing may also be attributed to operational difficulties related to sending out STI tests, as well as the different clinical protocols needed to collect samples from male and female patients. However, data suggests that adding STI testing services could be an advantage for centers seeking to increase their patient volumes. According to Experity data, the top 1% of urgent care centers in the United States attribute 6% of their total visits to STI testing (Figure 4). Urgent cares falling in lower percentiles see fewer STI patients with a steep drop-off even in the 95-99th percentile. In other words, only the top 1% of urgent care centers see STI testing as a material part of their business.
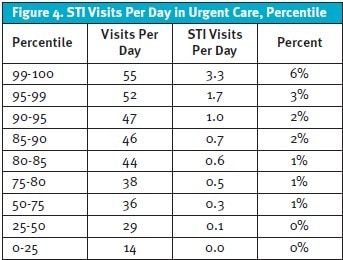
Notably, the top 10% of urgent care centers in terms of volume also see the most STI patients. This begs the question: Are STI patients boosting these numbers, or do higher pre-existing patient volumes simply increase the number of STI patient visits? It may vary for each center location, but in either case, adding services that bring in STI patients could be a valuable way for lower-volume urgent cares to drive additional patient visits.
So why aren’t more urgent care centers offering STI tests already?
Billing is 1 potential barrier. A send-out lab test on top of an urgent care visit can result in a cash bill well over $900 for uninsured patients, possibly driving patients to alternative testing locations. This strategy can still be viable—as demonstrated by the top percentile of clinics—especially when reference labs are willing to bill patients directly at a reasonable rate. However, the process becomes more complicated if the urgent care has to collect payment and remit reimbursement to the lab. The clinic also risks losing money if the staff does not accurately charge and collect patient out-of-pocket responsibility for lab services.
Meanwhile, historic limitations in rapid testing options have created a speed bump for operators to overcome. In order to add STI testing, some rapid lab equipment requires an upgrade from typical CLIA-waived (Clinical Laboratory Improvement Amendments) status to “moderately complex,” creating the need to hire a lab director and participate in subsequent inspections. Reimbursement from insurance may not cover the cost of these tests, making STI testing a money-losing proposition for many clinics.
Fortunately, improvements in rapid tests, discussed in further detail below, are poised to drastically reduce both the financial and logistical challenges posed by avoiding send-out labs altogether.
Urgent care operators have plenty of other issues to manage with STI testing. The following are some oft-cited reasons for not offering testing services:
- UC operators don’t believe they can get paid by insurance, especially for asymptomatic but exposed and concerned patients.
- They haven’t invested time or money into rapid testing and thus rely on third-party labs with long turnarounds and billing complexity that neither patients nor staff understand.
- A lag in lab reporting leads to presumptive treatment, resulting in patients not returning for test results.
- The providers simply don’t want to examine genitals or see patients from higher-risk cohorts.
- The providers don’t want to have difficult discussions, deal with partner notification, pre- or post-exposure prophylaxis or public health reporting.
- The providers would rather refer patients to community resources, such as family planning clinics, county health departments, and HIV service agencies, believing they shouldn’t “compete against free.”
Unlike many other services offered by urgent care, STI testing isn’t always straightforward to implement. However, operators cannot afford to ignore this business opportunity. Consider that federal sources recorded 2.5 million new cases of syphilis, chlamydia, and gonorrhea in 2022 alone. With the STI epidemic, and associated complications like antibiotic resistance, advancing at an alarming rate, the need for testing is even more pressing. An extraordinary number of patients need STI care, and UCs are well-positioned to offer convenient, accessible, and confidential testing.
Why Urgent Care?
Patients who are concerned about an STI have several options for where to get tested. They may opt to visit a primary care provider. They may choose to utilize free resources provided by a non-profit community health center or public health department.
However, urgent care offers patients seeking STI testing unique benefits, including rapid service and discreet care. These factors give UC an advantage over traditional testing providers. Increased access to STI testing is a net benefit to both the urgent care and the community.
Benefit to Public Health
Despite the low- or no-cost testing options offered by community non-profits, family planning clinics, and public health departments, many people avoid getting tested at these locations as they tend to carry a stigma. Likewise, patients may be uncomfortable visiting their primary care provider for testing since they may be uncomfortable sharing details of their sexual behavior.
This positions urgent care as a strong alternative. Patients can walk in for testing at their convenience and receive confidential care from a provider without establishing an ongoing relationship. For many, this is a far more comfortable option. The ease and privacy of UC could help improve STI testing rates and decrease overtreatment.
Improved Rapid Testing
Historically, limitations in the efficacy and profitability of STI testing have been attributed to available in-office testing options or the need to send out samples for third-party lab testing. Recent improvements in rapid testing, particularly through PCR tests and urine samples rather than traditional swabs, are helping change that narrative.
New PCR rapid test kits will make in-office testing for STIs as quick and easy as testing for influenza and strep—something urgent care centers already excel at. Moreover, the FDA will likely approve urine collection tests, making collecting samples even easier for urgent care staff in the near future.
Faster test results through new rapid testing kits could also lower the number of “lost” patients who never return to the clinic for treatment after a positive result. This could improve care for partners, who can be notified and begin their own treatment sooner.
Improved Reimbursement
In an effort to combat rising STI rates, the federal government has mandated reimbursement of STI testing for certain populations. Current regulations mainly focus on whether the patient is symptomatic. Urgent care operators must know these guidelines to ensure that STI testing services can remain profitable.
For instance, payers may consider post-exposure, asymptomatic testing a preventative service. While such tests are typically covered in a primary care office, they may be excluded from urgent care contracts because services are classified as episodic.
In the private sector, the Affordable Care Act (ACA) mandates that most health plans cover recommended preventative services, including HIV and other STI testing.3 This includes testing for STIs like syphilis, chlamydia, and gonorrhea—prime candidates for UC services. However, plan coverage may vary. Notably, the ACA requires all plans to cover HIV testing for all individuals between the ages of 15 and 65, as well as other ages within high-risk populations.
Medicaid has also expanded its coverage of STI-related care, including testing, counseling, screenings, and preventive vaccinations.4 Eligible populations may receive no-cost care for these services. Although most programs cover STI screenings, and all cover medically necessary HIV screenings, not all cover treatment if diagnosed. Medicare Part B, meanwhile, covers STI screenings once per year, or more often for individuals who are pregnant or at increased risk.
While the nuances of insurance reimbursement vary, operators should be aware that coverage is trending in a positive direction due to the growing rates of STIs and government initiatives to reverse this course. This is good news for urgent care, as adding these services with insurance reimbursement is a potentially profitable pathway that no longer relies on cash payments from patients.
Conclusion
The imperative need for urgent care centers to integrate STI testing into their service offerings is clear. With STI numbers reaching staggering new heights across the country, urgent care operators have a unique opportunity to help address this public health issue while also boosting patient volumes and revenue. Urgent care’s convenience, accessibility, and confidentiality make it an ideal setting for reaching a broad and diverse patient population, while advancements in rapid testing and evolving reimbursement policies are poised to alleviate historic barriers.
References
- World Health Organization website. Sexually Transmitted Infections Fact Sheet. July 10, 2023. Accessed at: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
- Centers for Disease Control and Prevention website. Sexually Transmitted Infections Surveillance, 2022. Accessed at: https://www.cdc.gov/std/statistics/2022/default.htm#:~:text=In%202022%2C%20more%20than%202.5,from%20all%20STI%20prevention%20partners.
- Kaiser Family Foundation website. Preventive Services Tracker. Accessed at: https://www.kff.org/affordable-care-act/report/preventive-services-tracker/
- Kaiser Family Foundation website. Medicaid Coverage of Family Planning Benefits: Findings from a 2021 State Survey Accessed at: https://www.kff.org/womens-health-policy/report/medicaid-coverage-of-family-planning-benefits-findings-from-a-2021-state-survey/
Download the Article PDF: The Urgent Need for STI Testing in Urgent Care Centers

