Urgent Message: Clinicians should inquire about the mechanism of injury when a patient presents with ankle pain and consider x-ray that includes the ankle, tibia, and fibula to evaluate for the possibility of Maisonneuve fracture, especially when pain in the inferiolateral knee is also present.
Willie O’Neal, MD; Bradley Strauch, MD
Citation: O’Neal W, Strauch B. Urgent Care Recognition and Management of Maisonneuve Fractures. J Urgent Care Med. 2024; 18 (11): 21-28
Editor’s Note: While the images presented here are authentic, the patient case scenarios are hypothetical.
Questions For the Clinician at the Bedside
- When should a Maisonneuve fracture be suspected?
- Does the presence of a Maisonneuve fracture alter management of an ankle injury?
- Does the presence of a Maisonneuve fracture prolong recovery?
- Can a Maisonneuve fracture be present without any pain at the proximal tibia/fibula?
Clinical Scenario
A 25-year-old male presented to urgent care (UC) with right ankle pain that occurred after externally rotating his foot during a game of pickup football. He was not able to bear any weight on the right ankle since the injury. The pain was worse with passive and active movements of the ankle. He denied numbness, tingling, and pain in the foot. There were no other injuries.
On exam, he winced in pain with ankle movements. The right ankle was moderately swollen; the skin was intact. The foot was warm and pink, dorsalis pedis (DP) and posterior tibial (PT) pulses were 2+. Palpation revealed tenderness of the medial and lateral malleoli, distal tibia and fibula, and deltoid ligament. There was no pain with palpation of the proximal 5th metatarsal. Anterior drawer and talar tilt tests were poorly tolerated, but there was no apparent ankle laxity.

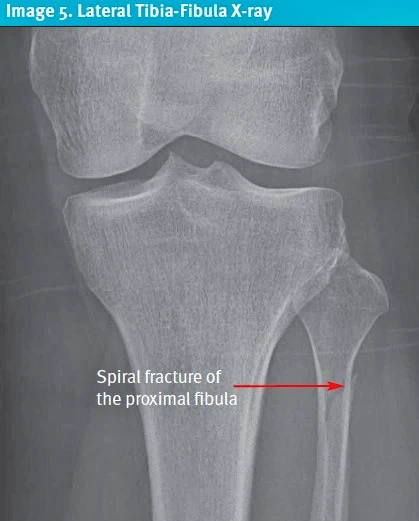
Staff ordered an x-ray (XR) prior to examination of the patient, which was read as normal (Image 1). As the patient returned from XR, he mentioned pain in the inferiolateral knee as well. The clinician astutely had concern for Maisonneuve fracture with the patient’s new pain complaint, and he was taken back for an XR of the tibia and fibula. The subsequent XR confirmed the presence of a proximal fibular fracture.
Discussion
A Maisonneuve fracture is a fracture of the proximal 1/3rd of the fibula which typically results from a severe twisting ankle injury causing disruption of the syndesmosis and interosseous membrane (IOM) of the lower leg.[1] This injury pattern most commonly occurs after significant external rotation of a planted pronated foot. It can also occur more rarely when the foot is twisted while supinated.1 The Maisonneuve fracture was named after the French orthopedic surgeon Jules Germain Francois Maisonneuve, the first to physician to describe the injury. Maisonneuve fractures are characterized by a proximal fibular fracture associated with a rupture of the tibiofibular syndesmosis and the anterior fibers of the deltoid ligament caused by external rotation mechanism.[2] The injury may also include a medial malleolar fractureoccurring in 73% of cases as found in a large case series.[3] The various mechanisms of injury found in 1 study were: sports-related injuries (46%); walking/running/slipping on ice (33%); traffic accidents (15%); and falling from a height (5%).[4]
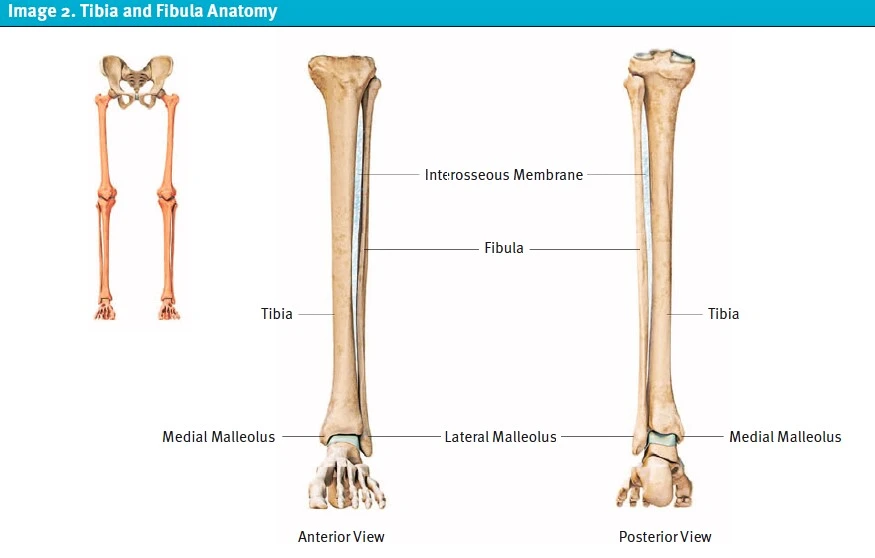
Relevant Anatomy
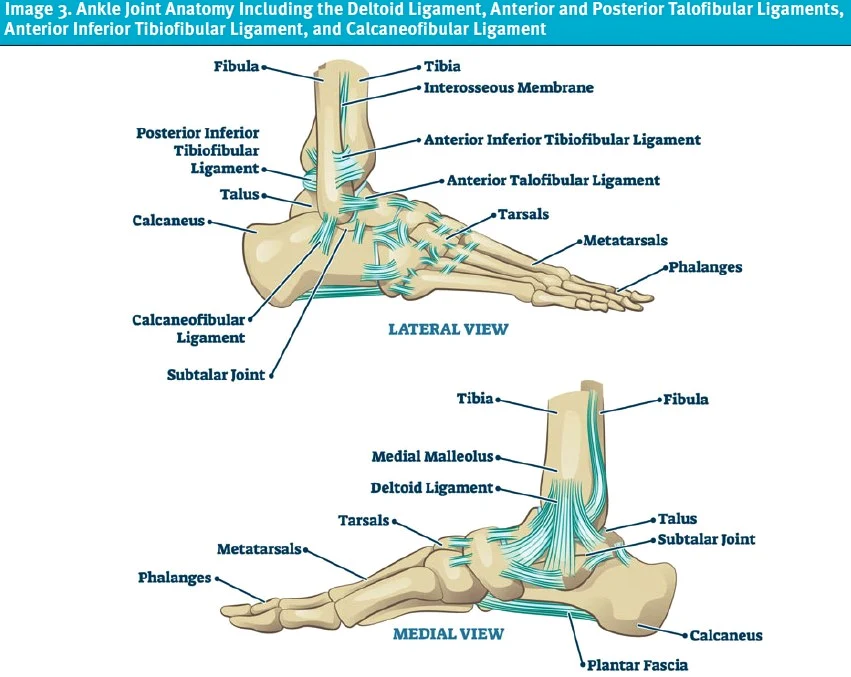
The ankle joint is comprised of the distal tibia and fibula (also called the medial and lateral malleoli) which sit atop the talus, and a strong IOM that holds the tibia and fibula together (Images 1-2). The bracket-shaped space between these 3 bones is called the “mortise” (Image 1). The ligaments of the ankle joint include (Image 3):
- Medial ligament—Deltoid ligament
- Lateral ligaments—Anterior and posterior talofibular ligaments (ATFL and PTFL), anterior inferior tibiofibular ligament (AITFL), and the calcaneofibular ligament (CFL)
These bones, ligaments, and IOM are collectively referred to as the tibiofibular syndesmosis, which plays a critical role for ankle function and stability.
Clinical History
Clinicians should inquire about the mechanism of injury with a focus on high impact injuries to the ankle, such as a fall from height or a motor vehicle accident. Elucidating whether the injury resulted from foot inversion (as is the case with the vast majority of ankle injuries) or eversion is an important historical feature to clue clinicians into the possibility of Maisonneuve fracture. As with any trauma evaluation, it is important to inquire about the possibility of associated injuries to the head, neck, torso, or other extremities. Evaluate for pain in other injury prone areas of the lower leg such as the Achilles tendon, the midfoot, and the proximal 5th metatarsal. Because an ankle injury with associated Maisonneuve fracture is likely to cause significant pain, patients may not specifically complain of severe pain at the proximal fibula.4,[5] Inquire about foot drop or numbness and paresthesia of the lateral lower leg and dorsum of foot to assess for the possibility of concomitant common peroneal nerve injury.
Physical Examination
The physical exam, as is the case with any ankle injury, should focus on the ankle, foot, and knee. It is important to have the patient remove their shoes and socks to expose the entire lower leg and evaluate for signs of trauma including swelling, deformity, and/or ecchymosis. Palpate the entire lower leg carefully, including both malleoli and the ankle ligaments, observing for areas of maximal tenderness. Palpate the entirety of the fibula with special attention to the proximal 1/3rd when considering a Maisonneuve fracture. Pain at the medial ankle may represent a deltoid ligament or medial malleolus injury. Pain at the lateral ankle may represent an ATFL, AITFL, PTFL, or lateral malleolus injury.
Evaluate range of motion of the ankle, knee, and toes. Special tests to evaluate for stability of the lower leg include the tibiofibular squeeze test and dorsiflexion external rotation stress test, which may indicate injury to the syndesmosis and IOM.1 However, performing these tests or other tests that require weight bearing will likely result in increased pain and unlikely change the management approach. Assessment for laxity in the acute setting often does not change management and can cause significant pain, therefore, this only need be performed as the patient can tolerate. Perform a focused neurovascular assessment of the DP and PT pulses and sensation of all aspects of the foot. Evaluate for any wounds or skin defects, which may suggest open injuries and have significant implications for immediate management.
Diagnostic Testing
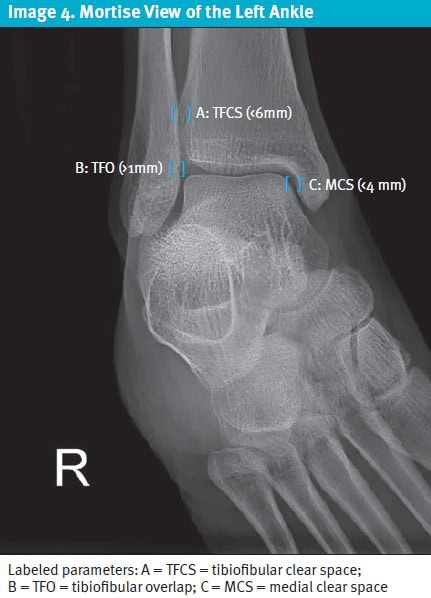
Testing centers around ankle radiographs, which include anteroposterior (AP), lateral, and mortise views. Significant ligamentous injury may be seen with pronation-external rotation injuries of the foot due to disruption of the syndesmosis. Because ligamentous injuries cannot be directly visualized on XR, secondary effects of ligamentous injury must be relied upon to suspect the diagnosis. Syndesmotic diastasis (widening of the syndesmosis) is an important suggestive finding of this to note.
Three radiographic parameters are used evaluate tibiofibular syndesmotic diastasis: tibiofibular clear space (TFCS); medial clear space (MCS); and tibiofibular overlap (TFO) (Image 4). These parameters are helpful in guiding diagnosis and management but are not required, and syndesmotic instability may be present even if they are normal.[6] Generally, >6mm width of the TFCS and >2mm displacement of the MCS are agreed upon as abnormal and may indicate syndesmotic instability.[7],[8],[9],[10] If both the TFCS and MCS are widened, the specificity for syndesmotic injury is 86%.7
When suspecting Maisonneuve fracture, it is critical to obtain both AP and lateral tibia-fibula radiographs. In one review of Maisonneuve fractures, the fracture of the proximal fibula (Image 5) was not reliably visible when only an AP view was obtained.1 Advanced imaging, (ie, computed tomography or magnetic resonance imaging) is fortunately not typically indicated as these modalities are largely not available in UC settings.
Urgent Care Management
Indications for emergent orthopedic evaluation for surgical repair include injuries associated with vascular or neurologic compromise, concern for compartment syndrome, and/or ankle fracture-dislocations. Otherwise, initial UC management involves splinting, instructions for non-weight bearing, and pain control. Options for splinting include a sugar tong splint, posterior splint, or air splint and knee immobilizer. Provide crutches to ensure the patient can comply with non-weight bearing. Initial pain management should include oral non-steroidal anti-inflammatory drugs and acetaminophen. A limited quantity of opioid analgesics may be provided depending on the degree of pain and consideration for the individual’s risk for adverse reactions and/or dependence.
If there is significant syndesmotic diastasis (ie, separation) or an associated fracture of the distal tibia, non-emergent evaluation for surgical repair is indicated.1 If there is no significant syndesmotic diastasis or ankle fracture, conservative management may be considered.1 The proximal fibular fracture itself is typically managed with immobilization and non-weight bearing. If there is neurovascular injury associated with the fibula fracture, surgical evaluation is needed. If emergent orthopedic evaluation is not indicated, orthopedics follow-up should be as soon as possible, ideally within 3-7 days after injury.
Next-Level Urgent Care Pearls
- If a Maisonneuve fracture is diagnosed, and there is not an associated ankle dislocation or neurovascular compromise, a real-time discussion with an orthopedist (as available) may help avoid a an emergency department visit.
- Be cautious if the XR for patients with “ankle injury” are ordered by staff prior to examining the patient. The knee should be examined in all patients with ankle injuries, and if there is proximal fibular tenderness, an AP and lateral series of the tibia and fibula should also be obtained.
- Inquire about the possibility of other associated injuries, and always directly visualize and assess the joint above and below the site of injury (eg, foot and ankle).
- If the ankle XR shows no obvious widening of the mortise and a Maisonneuve fracture is identified, then stress/weight-bearing radiographs may be helpful in determining the likelihood of the patient requiring surgical fixation. However, if this is not feasible or the patient cannot tolerate any weight-bearing, this can be deferred until orthopedist follow-up.
Red Flags and Pitfalls
- Even when the patient is not complaining of subjective pain at the proximal fibula, a Maisonneuve fracture may be present. It is important to specifically palpate the proximal fibula with each ankle pain/sprain patient.
- While uncommon, Maisonneuve fractures associated with higher energy mechanisms may put patients at risk of immediate or delayed compartment syndrome. In patients with more severe mechanisms and those who are anticoagulated, ensure patients are aware of this possibility and that they understand that severe and escalating pain, particularly if it occurs without movement or weight-bearing, or is associated with paresthesias, should prompt immediate ED evaluation.[11]
- With a Maisonneuve or other proximal fibula fracture, ensure to evaluate for damage of the common peroneal nerve. Due to the proximity and course of the common peroneal nerve and its branches to the proximal fibula, it is particularly vulnerable to injury. Assess foot dorsiflexion and eversion, as well as sensation of the lateral lower leg and dorsum of the foot.
Clinical Scenario Conclusion
The patient’s XR of the tibia and fibula revealed a spiral fracture of the proximal fibula. He received acetaminophen 1,000 mg, ibuprofen 600 mg, and an ice pack for analgesia while in UC. The patient was immobilized with a lower leg sugar tong splint and provided crutches with instructions to maintain strict non-weight bearing. Because he did not have deformity of the ankle or neurovascular compromise, the patient was referred to orthopedics within the next 2-3 days.
Takeaway Points
- Evaluate for syndesmosis instability and a proximal fibular fracture in all ankle injuries. Either of these findings may have implications on both immediate management, activity precautions, and likelihood of requiring surgical fixation.
- If there is proximal fibula pain subjectively or tenderness on exam, obtain AP and lateral tibia-fibula radiographs to evaluate for a Maisonneuve fracture.
- Obtain AP, laterolateral, and mortise views of the ankle. If the mortise view shows widening of the TFCS (>6mm) or MCS (>2mm difference vs contralateral side of mortise), syndesmosis instability may be present.
- Once a Maisonneuve fracture is confirmed, management includes pain control, splint immobilization with strict non-weight bearing, and timely orthopedic evaluation.
- Orthopedic management usually includes surgical fixation if there is ankle syndesmotic injury, however there are some instances when conservative therapy may be an option.
Manuscript submitted July 7, 2024; accepted August 2, 2024.
- [1]. Bartoníček J, Rammelt S, Tuček M. Maisonneuve Fractures of the Ankle: A Critical Analysis Review. JBJS Rev. 2022 Feb 21;10(2). doi: 10.2106/JBJS.RVW.21.00160. PMID: 35180143.
- [2]. Maisonneuve MJG. Recherches sur la fracture du péroné. Arch Gen Med 7:165–187, 1840.
- [3]. He J, Ma X, Xin J, et al. Pathoanatomy and Injury Mechanism of Typical Maisonneuve Fracture. Orthopaedic Surgery. 2020;12(6):1644-1651. doi:https://doi.org/10.1111/os.12733
- [4]. Kalyani BS, Roberts CS, Giannoudis PV. The Maisonneuve Injury: A Comprehensive Review. Orthopedics. 2010;33(3):190-195. doi:https://doi.org/10.3928/01477447-20100129-25
- [5]. Taweel NR, Raikin SM, Karanjia HN, Ahmad J. The Proximal Fibula Should Be Examined In All Patients with Ankle Injury: A Case Series of Missed Maisonneuve Fractures. The Journal of Emergency Medicine. 2013;44(2):e251-e255. doi:https://doi.org/10.1016/j.jemermed.2012.09.016
- [6]. Smith MG, Ferguson E, Kurdy NM. Persistent Diastasis in a Maisonneuve Fracture—Interposition of a Tibial Osteochondral Fragment: A Case Report. The Journal of Foot and Ankle Surgery. 2005;44(3):225-227. doi: https://doi.org/10.1053/j.jfas.2005.02.004
- [7]. Schoennagel BP, Karul M, Avanesov M, et al. Isolated syndesmotic injury in acute ankle trauma: Comparison of plain film radiography with 3T MRI. European Journal of Radiology. 2014;83(10):1856-1861. doi:https://doi.org/10.1016/j.ejrad.2014.06.034
- [8]. Pogliacomi F, De Filippo M, Casalini D, et al. Acute syndesmotic injuries in ankle fractures: From diagnosis to treatment and current concepts. World Journal of Orthopedics. 2021;12(5):270-291. doi:https://doi.org/10.5312/wjo.v12.i5.270
- [9]. Tourné Y, Molinier F, Andrieu M, Porta J, Barbier G. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthopaedics & Traumatology: Surgery & Research. 2019;105(8):S275-S286. doi:https://doi.org/10.1016/j.otsr.2019.09.014
- [10]. Grath GB. Widening of the ankle mortise. A clinical and experimental study. Acta Chir Scand Suppl. 1960;Suppl 263:1-88.
- [11]. Tangaraju L, et al. Delayed Occurrence of Compartment Syndrome in Maisonneuve Fracture – Timely Catch To Save A Limb. Malaysian Orthopaedic Journal. 2023 (16) Supplement A.
Down the article PDF: Urgent Care Recognition and Management of Maisonneuve Fractures
