Urgent Message: Patients with a moderate-risk HEART score referred from an urgent care center for an expedited outpatient cardiology evaluation were found to have a very low rate of MACE and no occurrence of ischemic cardiac deaths.
Citation: Thomson N, Barbarash S, Lebron-Gallagher D, Julson H, Weinstock M. Major Adverse Cardiovascular Events in Patients with Chest Pain And Moderate Heart Risk Scores Who Were Referred For An Expedited Outpatient Cardiology Evaluation: A Multi-Center Descriptive Study. J Urgent Care Med. 2024; 18(11): 28-32
Nick Thomson, MD; Svetlana Barbarash, MD; Deloros Lebron-Gallagher, PA-C; Hollis Julson, MD; Michael Weinstock, MD
Abstract
Introduction: The HEART score is an effective method of risk-stratifying emergency department (ED) patients with chest pain. This group of authors first described the low rate of major adverse cardiovascular events (MACE) in patients with a moderate-risk HEART score referred from an urgent care (UC) center for an expedited outpatient cardiology evaluation in a 2020 publication. This is a follow-up study of 446 UC patients presenting with acute chest pain over a 36-month period.
In the United States, patients with a moderate-risk HEART score who present to the ED are often hospitalized for further evaluation. The safety of outpatient evaluation of these patients is not well studied. We assessed the hypothesis that the rate of MACE is low among UC patients with acute chest pain and a moderate-risk HEART score and that expedited outpatient referral for cardiology evaluation is a safe practice for this population of patients.
Methods: A cross-sectional retrospective cohort study was performed from February 14, 2019, through March 30, 2022, in 5 UC centers in Las Vegas, Nevada. Included were 446 patients who presented with chest pain or potential anginal equivalent symptoms and had a HEART score calculated to be between 4 to 6 in the UC. A streamlined disposition protocol was adopted by all UC providers for an expedited outpatient cardiology evaluation instead of immediate ED referral. The population was followed for 6 weeks with a primary endpoint of MACE (death, myocardial infarction [MI], coronary revascularization) determined by electronic medical record review and direct phone contact with patients. Outcomes were confirmed in 93% of patients.
Results: The average age of subjects was 65 years. Participants were 52% female. In the study, 395 patients (89%) were seen by a cardiology provider, and 346 patients (88%) were seen within 3 days. Diagnostic evaluations ordered included 265 cardiac stress tests (67%), 42 coronary computed tomography angiograms (11%), and 19 invasive coronary angiograms (5%). Eight patients (2%) were found to have MACE during the follow-up period: 2 had routine surgical revascularization; 4 had non-fatal MI followed by revascularization; and 2 patients died. Among the 2 patients who died, 1 was urgently referred for mitral valve replacement and died after surgery from renal failure and COVID-19, and the other patient died from COVID-19 pneumonia. There were no ischemic cardiac deaths.
Conclusion: Based on our descriptive analysis, patients with a moderate-risk HEART score referred from UC for an expedited outpatient cardiology evaluation were found to have a very low rate of MACE and no ischemic cardiac deaths occurred.
This data was originally presented as a moderated poster at the American Heart Association (AHA) conference in Chicago, Illinois, in 2022.
Introduction
Chest pain is a common chief complaint in the emergency department (ED), accounting for over 7 million annual visits in the U.S.[1] Effective risk stratification of chest pain patients is crucial for identifying those at low short-term risk of major adverse cardiovascular events (MACE), including death, myocardial infarction (MI), and coronary revascularization, to allow for safe and expedited outpatient management while ensuring optimal allocation of healthcare resources. However, even with established risk-stratification protocols in place, many physicians are uncomfortable with discharging patients even in situations of very low risk of MACE.[2],[3]
The HEART score, introduced as a chest pain risk-stratification tool in 2008[4] and validated in 2013,[5] has been implemented widely in ED settings for its ability to predict adverse outcomes in chest pain patients. This scoring system assesses 5 key parameters—history, electrocardiogram (ECG) findings, age, risk factors, and troponin levels—assigning scores ranging from 0 to 2 to each parameter. Patients are then categorized into low (0-3), moderate (4-6), or high (7-10) risk groups based on their total score.4
In the 2013 HEART score validation study, patients with scores of 0-3, indicating low risk, were found to have a short-term risk of MACE of 1.7%. However, in this study, those with moderate-risk scores (4-6), were typically admitted to the hospital and had a rate of MACE of 16.6%. Patients with scores ≥7, indicating high risk, were treated as candidates for early invasive measures due to their substantial risk of MACE of 65%.5
The HEART score’s simplicity and effectiveness in identifying patients at low risk of MACE have made it a valuable tool for guiding clinical decision-making in ED settings.[6],[7] However, the optimal management strategy for patients in the moderate-risk category remains uncertain as little is known about the effectiveness of close outpatient cardiology follow-up versus admission for this patient subgroup.
This study aimed to investigate the frequency of MACE in moderate-risk patients after receiving a negative assessment at an urgent care (UC) facility who were referred for an expedited outpatient cardiology follow-up.
Methods
A cross-sectional study was conducted from February 14, 2019, to March 30, 2022, at 5 UC centers in Las Vegas, Nevada. The study included 446 patients who presented with chest pain or possible anginal equivalent symptom and who had a HEART score of 4 to 6.
The exclusion criteria included patients under the age of 18 and unstable vital signs.
Patients were evaluated by UC providers, predominantly consisting of board-certified family medicine physicians and advanced-practice providers (APPs), including physician assistants and nurse practitioners. Subsequently, in cardiology follow-up, patients were assessed by cardiologists (for new patients) or APPs (for established patients).
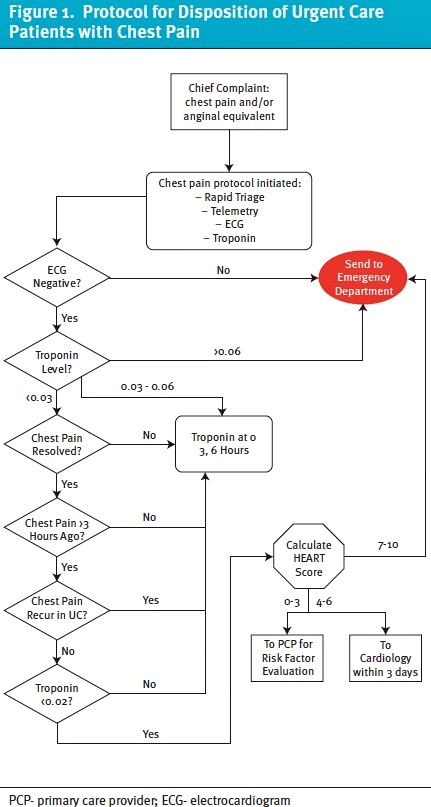
All UC providers uniformly adopted a standardized disposition protocol, leading patients with moderate-risk HEART scores to be promptly scheduled for expedited cardiology evaluation within 3 days of discharge. UC staff directly facilitated appointment scheduling. During cardiology appointments, further work-up decisions were made, encompassing medical treatment, outpatient stress testing, echocardiography, coronary computed tomography angiograms (CCTA), or conventional coronary angiography at the discretion of the cardiology clinician (Figure 1).
Participants were followed for 6 weeks after the index UC presentation; MACE served as the primary endpoint. MACE outcomes were ascertained through comprehensive review of electronic medical records and direct phone contact with patients, with complete follow-up data being available for 93% of patients. Subsequently, the rates of MACE occurrence within the 6-week follow-up period were calculated.
The study was approved by the Institutional Review Board #2020-0050 as an exempt study on June 18, 2020.
Results
A total of 446 patients with a moderate-risk HEART score were referred to outpatient cardiology in an expedited manner. The average age of patients was 65 years with 233 (52%) being female (Table 1).
| Average Age | 65 years |
| Females | 233 (52%) |
| Males | 213 (48%) |
| HEART Score 4 | 262 (59%) |
| HEART Score 5 | 141 (32%) |
| HEART Score 6 | 43 (9%) |
| Arteriosclerosis | 156 (35%) |
| Hypertension | 335 (75%) |
| Diabetes | 153 (34%) |
| Dyslipidemia | 376 (84%) |
| Obesity | 122 (27%) |
| Tobacco Use | 55 (12%) |
| CVA/TIA | 30 (7%) |
CVA- cerebral vascular accident; TIA- transient ischemic attack
Among them, 395 patients (89%) received evaluation by a cardiology provider, and 346 patients (88%) were seen within 3 days following discharge from UC.
Among the patients who were seen by a cardiology provider, 265 stress tests were ordered, representing 67% of patients seen, with 232 stress tests actually completed. Additionally, 42 CCTA studies were ordered, representing 11% of patients seen, with 30 completed. Furthermore, 19 invasive coronary angiograms were ordered, representing 5% of patients seen, with 13 completed.
During the 6-week follow-up period, a total of 8 patients (2%) were found to have a MACE outcome (Table 2). This included 2 patients who underwent routine surgical revascularization, 4 patients who experienced non-fatal myocardial infarctions followed by revascularization procedures, and 2 patients who died related to causes other than ischemic cardiac events. One patient, urgently referred for mitral valve replacement, died post-surgery from renal failure and complications related to COVID-19. The other patient died from COVID-19 pneumonia. There were no cases of ischemic cardiac deaths observed during the study period.
| Patient Age and Sex | Symptoms | Heart Score | Positive Components | Time to Cardiology Evaluation | Diagnostic Test | MACE Outcome |
| 67, M | UC 5/13/19 with throat pain for 2 weeks | 5 | History: 2 Age: 2 Risk: 1 | 1 | Stress delayed | ACS 5/26/19, PCI to RCA |
| 70, M | UC 7/15/19 CP responsive to NTG | 6 | History: 2 Age: 2 Risk: 2 | 2 | LHC recommended | LHC 8/7/19 noting MVCAD, 4V CABG 8/19/19 |
| 65, F | UC 10/23/19 with mild CP, dyspnea x 7 days | 5 | History: 1 EKG: 1 Age: 2 Risk: 1 | 2 | TTE normal LVEF. | Referred for LHC, 2V CABG 11/27/19 |
| 54, M | UC 3/8/20 with CHF | 4 | N/A | 2 | TTE with critical bioprosthetic MS and severe elevated PAP. Sent directly to ED | Underwent CABG/MVR. Developed renal failure/COVID and died |
| 67, F | UC 2/23/21 with sharp CP at rest | 4 | History: 0 Age: 2 Risk: 2 | 2 (no show) | None | 2/24/21 NSTEMI with PCI to LCx and RCA |
| 84, F | UC 7/19/21 with exertional chest heaviness | 5 | History: 1 Age: 2 Risk: 2 | 3 (no show) | None | 8/11/21 STEMI leading to 4V CABG |
| 71, M | UC 9/14/21 | 5 | History: 1 Age: 2 Risk: 2 | 2 | Nuclear stress cancelled due to hospitalization | 9/25/21 with COVID pneumonia, cardiac arrest due to hypoxia 10/9/21. |
| 87, M | UC 9/20/21 with CP and CHF symptoms | 4 | History: 0 Age: 2 Risk: 2 | 3 | Treated for CHF, referred for angiogram as part of pre-TAVR work up for severe AS | 10/13/21 NSTEMI with PCI to proximal/mid Diagonal branch |
M – male; F – female; UC – urgent care; CP- chest pain; CHF- congestive heart failure; SOB- shortness of breath; NTG- nitroglycerin; CABG- coronary artery bypass graft; CAD- coronary artery disease; DES- drug eluting stent; ECG- electrocardiography; LHC- left heart catheterization; LAD- left anterior descending; LCx- left circumflex; MS- mitral stenosis; AS- aortic stenosis; TAVR- transcatheter aortic valve replacement; MVR- mitral valve replacement; nSTEMI- non- ST-elevation myocardial infarction; RCA- right coronary artery; TTE- transthoracic echocardiogram; EF- ejection fraction; PCI – percutaneous coronary intervention.
Discussion
The findings of this descriptive study provide valuable insights into the short-term risks and management strategies of patients presenting to UC centers with moderate-risk HEART scores. Our results indicate that the implementation of a streamlined disposition protocol directing these patients to expedited outpatient cardiology evaluation is feasible and associated with timely access to specialized care and low MACE rates.
The high rate of cardiology provider evaluation (93%) emphasizes the effectiveness of this approach in ensuring that patients receive appropriate follow-up when a protocol is in place. Moreover, the majority of patients (88%) were seen within 3 days post-discharge, highlighting the success of the expedited referral process. This timely access to cardiology evaluation allows for prompt diagnostic testing with stress tests being the most commonly ordered test (67%). However, there remains room for improvement in completion rates of diagnostic tests, as evidenced by the discrepancy between tests ordered and tests completed. Furthermore, it is uncertain the degree to which these further cardiac investigations may affect longer-term risk of adverse cardiovascular outcomes in the moderate-risk HEART score group.
Our study observed a low rate of MACE within the 6-week follow-up period (2%), which is lower than previous research on the effectiveness of the HEART score in risk stratification for patients with acute chest pain.5 The 2% “acceptable miss rate” is consistent with recommendations from the American College of Emergency Physicians (ACEP) clinical policy statement.6 Notably, there were no ischemic cardiac deaths observed, suggesting that the expedited outpatient cardiology evaluation pathway is effective in identifying moderate-risk HEART score patients.[8], [9],[10]
Of note, many UC facilities are not able obtain rapid results for troponin blood tests. We excluded patients with positive troponin blood tests in this study. In recent years, the HEAR score (History, ECG, Age, Risk factors [ie, no troponin]) has been studied as a more rapid option for risk stratifying chest pain patients in lower resource environments. At extremely low scores, such as 0 or 1, the negative predictive value is very high; these patients would have a very low risk of MACE. Also of note, these patients were typically studied in an ED setting, so it is difficult to definitively extrapolate these results to the urgent care.[11],[12],[13]
The cases of MACE observed in our study highlight the importance of continued vigilance and comprehensive follow-up in patients with moderate-risk HEART scores. While the majority of patients had favorable outcomes, a small proportion experienced significant events, emphasizing the importance of close follow-up. However, based on these results, it appears that stable patients without concerning ECG findings or positive troponins who have moderate-risk HEART scores would not derive sufficient benefit to justify hospital admission when close follow-up can be arranged.
Limitations
The study used a retrospective approach, thereby confining the investigators to chart review and telephone patient interviews. The study was set within 5 UC centers located in Las Vegas, Nevada, influencing the generalizability of its findings to broader healthcare contexts. Furthermore, the relatively modest sample size of 446 patients underscores potential limitations in statistical power and precision of estimations.
Despite efforts to track patient outcomes over a 6-week post-presentation period—the follow-up rate was 93% (395 patients)—we could not confirm outcomes in 7% of patients which may have had unknown adverse outcomes. Moreover, while a substantial proportion of patients underwent diagnostic assessment during cardiological follow-up, there was a disparity between ordered tests and tests that were actually completed.
Lastly, the study’s methodology lacks consideration for potentially confounding variables, including but not limited to comorbidities, socioeconomic status, and healthcare access, which could significantly influence the observed outcomes. It is imperative to recognize that not all healthcare settings possess the logistical capability to facilitate expedited follow-up consultations within the stipulated timeframe of 1-3 days. This assertion aligns with the clinical policy guidance articulated by ACEP in 2018, advocating for judicious consideration of further diagnostic measures or extended observation in instances where timely follow-up cannot be feasibly arranged within 1 to 2 weeks.6
Conclusion
Patients with a moderate-risk HEART score referred from urgent care for an expedited outpatient cardiology evaluation demonstrated a low rate of MACE and notably, no ischemic cardiac deaths attributable to delayed care. Implementing such pathways may not only improve patient outcomes but also optimize resource utilization by reducing unnecessary hospital admissions.
Manuscript submitted April 3, 2024; accepted July 10, 2024.
References
- [1]. Januzzi, J, McCarthy, C. Evaluating Chest Pain in the Emergency Department: Searching for the Optimal Gatekeeper. J Am Coll Cardiol. 2018 Feb, 71 (6) 617–619.
- [2]. Than M, Herbert M, Flaws D, et al. What is an acceptable risk of major adverse cardiac event in chest pain patients soon after discharge from the emergency department? Int J Cardiol. 2013;166(3):752-754. doi:10.1016/j.ijcard.2012.09.171
- [3]. Weinstock MB, Pallaci M, Mattu A, Berg C, Jhun P, Riddell J. Most Clinicians Are Still Not Comfortable Sending Chest Pain Patients Home with a Very Low Risk of 30-Day Major Adverse Cardiac Event (MACE). J Urgent Care Med. 2021;15(5):17-21
- [4]. Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008 Jun;16(6):191-6. doi: 10.1007/BF03086144. PMID: 18665203; PMCID: PMC2442661.
- [5]. Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013;168(3):2153-2158.
- [6]. Tomaszewski CA, Nestler D, Shah KH, Sudhir A, Brown MD. Clinical Policy: Critical Issues in the Evaluation and Management of Emergency Department Patients With Suspected Non-ST-Elevation Acute Coronary Syndromes. American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Suspected Non–ST-Elevation Acute Coronary Syndromes. Ann Emerg Med. 2018;72(5):e65-e106. doi:10.1016/j.annemergmed.2018.07.045.
- [7]. Kontos, M, de Lemos, J. et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov, 80 (20) 1925–1960.
- [8]. Spiegel R, Sutherland M, Brown R, Honasoge A, Witting M. Clinically relevant adverse cardiovascular events in intermediate heart score patients admitted to the hospital following a negative emergency department evaluation. Am J Emerg Med. 2021;46:469-475. doi:10.1016/j.ajem.2020.10.065
- [9]. Barbarash S, Lebron-Gallagher D, Julson H, Weinstock MB. There is a low rate of major adverse cardiovascular events in chest pain patients with a moderate risk heart score referred from urgent care for expedited outpatient cardiology evaluation: a multi-center study. Complex Issues of Cardiovascular Diseases. 2021;10(1).
- [10]. Barbarash S, Lebron-Gallagher D, Julson H, Weinstock MB. A Multicenter Study of the Rate of MACE in Chest Pain Patients with a Moderate HEART Risk Score Referred from Urgent Care for an Expedited Outpatient Cardiology Evaluation. J Urgent Care Med. 2020; 14 (11) 31-35.
- [11]. O’Rielly CM, Andruchow JE, McRae AD. External validation of a low HEAR score to identify emergency department chest pain patients at very low risk of major adverse cardiac events without troponin testing. CJEM. 2022;24(1):68-74. doi:10.1007/s43678-021-00159-y
- [12]. Todd F, Duff J, Carlton E. Identifying low-risk chest pain in the emergency department without troponin testing: a validation study of the HE-MACS and HEAR risk scores. Emerg Med J. 2022 Jul;39(7):515-518. doi: 10.1136/emermed-2021-211669. Epub 2021 Nov 9. PMID: 34753776.
- [13]. Khaleghi Rad M, Pirmoradi MM, Doosti-Irani A, Thiruganasambandamoorthy V, Mirfazaelian H. The performance of HEAR score for identification of low-risk chest pain: a systematic review and meta-analysis. Eur J Emerg Med. 2022;29(3):173-187. doi:10.1097/MEJ.0000000000000921
Download the Article PDF: Major Adverse Cardiovascular Events in Patients with Chest Pain And Moderate Heart Risk Scores Who Were Referred For An Expedited Outpatient Cardiology Evaluation: A Multi-Center Descriptive Study

