Published on
Urgent Message: Proximal humerus fractures most commonly occur in older patients after a fall and can be sentinel events that offer an opportunity to identify undiagnosed medical conditions or unsafe home environments.
Lauren Schuermann, MS4; Shivani Kothari, MS4; W. Bradley Strauch, MD
Citation: Schuermann L, Kothari S, Strauch B. Urgent Care Recognition and Management of Proximal Humerus Fractures. J Urgent Care Med. 2024; 19(2): 13-19
Questions for the Clinician at the Bedside
- What are the common mechanisms for proximal humerus fractures?
- What complications may be encountered in patients with proximal humerus fractures?
- When is emergency department referral or surgery indicated?
- How should patients discharged from urgent care be managed?
Clinical Scenario
A 72-year-old, right-hand dominant man presented to urgent care (UC) with right shoulder and arm pain after a mechanical fall from standing earlier that day. He noted that he tripped on a rug and fell directly onto his right shoulder at home, striking the edge of a stair before he could brace himself. His pain is worsened with any attempts to move the shoulder. He denied neck pain, elbow and wrist pain as well as numbness or paresthesia anywhere in the arm. He denied hitting his head. He had no history of prior falls. His past medical history was significant for hypertension, depression, and hyperlipidemia. He was a daily cigarette smoker and drank alcohol frequently but was not intoxicated at the time of the fall or at the time of his UC presentation.
His vital signs were significant for an elevated blood pressure with mild tachycardia and tachypnea. He was alert, oriented, and appeared uncomfortable with his right arm held in abduction against his side. Any attempts at movement of the right shoulder passively caused obvious increases in his pain. He had a superficial abrasion on the lateral aspect of the right shoulder and generalized tenderness with palpation of the entire right shoulder, most significant laterally. He denied tenderness with palpation of the arm from the wrist to distal humerus, the entire clavicle, sternum, scapula, and cervical spine. There was no obvious deformity or empty sulcus sign. His sensation throughout the right hand, forearm, and lateral upper arm was intact, and he had normal movements of right hand and wrist. He could supinate and pronate his forearm without significant discomfort but refused to move his right shoulder actively due to pain. He had strong radial and ulnar pulses. Screening exam of the rest of his extremities, head, and torso revealed no concerning findings or evidence of trauma.
X-rays (XR) of the right shoulder were obtained which demonstrated a comminuted and minimally displaced fracture of the proximal humerus (Image 1).

Relevant Anatomy
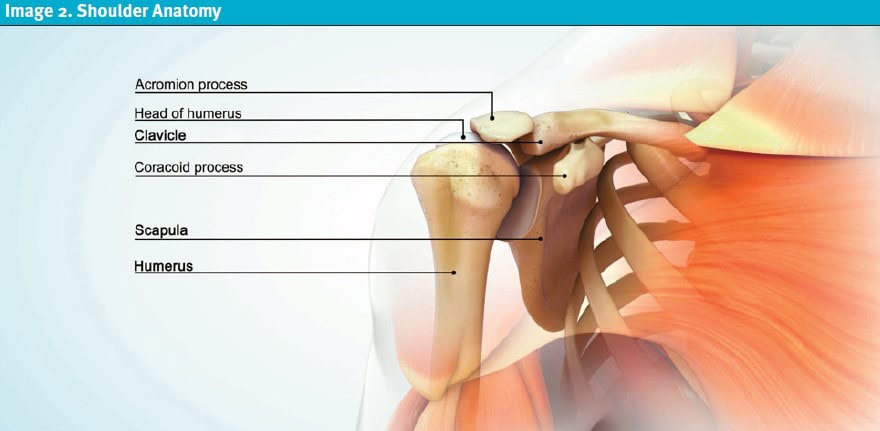
The humeral head articulates with the glenoid fossa of the scapula, forming the glenohumeral (shoulder) joint space. Other osseous structures in this region include the distal clavicle and acromion and coracoid processes of the scapula. The proximal humeral anatomy is divided into the anatomic neck (formed when the physis fuses in adolescence) and the surgical neck, a structurally weaker area located inferior to the humeral head. Due to this inherent weakness, proximal humerus fractures are most common at the surgical neck.[1]
The shoulder joint, relative to other ball-and-socket joints (eg, the hip) sacrifices stability for greater mobility and range of motion. Unlike the acetabulum, the humeral head is held in place predominantly by tendonous insertions of the rotator cuff musculature (Image 2).[2] The rotator cuff is comprised of 4 muscles and their myotendinous attachments. Teres minor, supraspinatus, and infraspinatus all attach to the greater tuberosity of the humerus; the subscapularis alone inserts on humerus’ lesser tuberosity.2
The axillary nerve is the most commonly injured nerve associated with proximal humerus fractures.1 In most individuals, the axillary nerve travels deep to the deltoid muscle in close approximation to the proximal lateral humerus, making it particularly vulnerable to injury in surgical neck fractures. The blood supply of the proximal humerus is highly variable, but most commonly it is supplied by the anterior humeral circumflex artery, which most often originates from the axillary artery. Arcuate arteries form anastomoses with the surrounding vessels, including the posterior humeral circumflex artery, which serves as the primary blood supply to the humeral head in most individuals. This leads to a common phenomenon of retrograde perfusion supplying the small penetrating intraosseous vessels.[3]
Proximal Humerus Fractures
Proximal humerus fractures are relatively common, comprising 4-6% of all adult fractures.1 They predominantly affect women and the elderly most commonly after low-energy trauma, such as in the clinical scenario presented. In such cases, these are often termed “fragility fractures,”1 which alludes to injuries associated with increasing patient fragility. Falls from standing are the most common mechanism for fragility fractures. Multifactorial aspects of fragility contribute to the risk of such falls, such as generalized weakness, osteopenia, impaired balance and/or vision, low body mass index, and female gender. Concurrent substance use disorder increases the risk of fragility fractures.[4]
Proximal humerus fractures do occur in younger individuals, but usually this involves a higher energy trauma mechanism. Younger patients are also much more likely to suffer glenohumeral dislocations rather than proximal humeral fractures with blows to the upper arm.
In certain cases of dislocation, there can be impaction of the humeral head from impact with the glenoid rim resulting in a Hill-Sachs deformity. While technically a fracture of the proximal humerus, the Hill-Sachs deformity differs significantly from other proximal humerus fracture as it is usually evident in cases of glenohumeral dislocation.[5] Approximately 50-65% of proximal humerus fractures are minimally displaced injuries to the greater tuberosity or surgical neck, while 20-30% are comminuted fractures of the surgical neck.2 Proximal humeral fractures, since they occur predominantly in elderly and frail individuals, are frequently associated with clinically significant injuries to the head, neck, clavicle, elbow, and/or wrist.1
History
As with all trauma presentations, understanding the mechanism of injury is critical to ensuring an appropriate differential diagnosis and work-up plan are formulated. Additionally, it is important to assess locations of significant pain and what exacerbates the pain, assessing for sensation or motor changes, which may indicate a neurovascular injury. If there is disruption of the skin, it is worthwhile to inquire about the patient’s tetanus vaccination history.
Because proximal humerus fractures occur most commonly in elderly patients after a fall, a common pitfall is to focus on the injury without inquiring about the circumstances surrounding the fall. Inquiring about the possibility of loss of consciousness can lead to identification of seizure or syncope, which may necessitate an entirely separate differential and work-up. While syncope often occurs due to benign causes (eg, orthostasis, vasovagal episodes), the possibility of cardiogenic causes increases with increasing age and comorbidities such as congestive heart failure (CHF) or coronary artery disease. It’s important to note that pre-syncope and syncope have the same differential diagnoses, and even patients who did not fully lose consciousness may have had a serious cause for their lightheadedness. They warrant careful history of the symptoms preceding the fall, review of vital signs, and electrocardiogram at a minimum.[6],[7]
Seizure is an alternate cause for sudden loss of consciousness and falls that should be considered. Unlike syncope, patients with seizures often have prolonged rhythmic jerking and are amnestic to the event. Tongue biting, urinary incontinence, and a preceding aura are also more common with seizure, but presence or absence of these signs and symptoms does not confirm or refute the diagnosis of seizure. However, the presence of a postictal state (ie, slow return to normal awareness) is strongly associated with seizure. Clinically, distinguishing between seizure and syncope, even with inquiry into all the mentioned features, may not always be possible, and neurologist referral and electroencephalogram are sometimes required.[8] Collateral history from bystanders who witnessed the fall can be very helpful as well. Additionally, assessing for symptoms that preceded the fall, such as headache, nausea, vomiting, weakness, numbness, or visual changes, can be helpful in distinguishing if events, such as cerebrovascular accidents (CVA), may have precipitated the fall.
Additionally, chest pain, shoulder pain, or back pain prior to the fall should be assessed as this may represent acute coronary syndrome (ACS), pulmonary embolism (PE), or aortic dissection (AD). If the patient is having shortness of breath, again ascertaining if it predated the fall may suggest PE or CHF, for example, whereas similar symptoms after the fall might be more suggestive of thoracic injuries such as rib fractures or pneumothorax (PTX).
In the cases where a medical event is not suspected as causative of the fall, the term “mechanical fall” is often used. It is critical to note, however, that elderly patients who fall for reasons not related to a preceding medical event still benefit from additional data gathering. A 2016 retrospective ED study of patients who presented after a fall showed that there was no difference in 30-day ED revisit, hospitalizations, or death between groups who fell for mechanical and non-mechanical reasons.[9] In other words, falls in the elderly appear to be a marker for frailty and risk for short term poor outcomes, regardless of etiology. Moreover, mechanical falls may be due to some aspect of the home environment that is unsafe and needs to be remedied to mitigate the risk of future falls. It is crucial to inquire about things like stairs, lighting, and the presence of assistive equipment (eg, grab bars) in home bathroom facilities to identify sources of risk for falling again.[10]
Determining the patient’s dominant hand and level of assistance at home also will be helpful for minimizing risk of additional morbidity associated with their shoulder injury given the necessary loss of use of 1 arm and likely use of potentially sedating medications for pain.[11] While not a medical necessity, some patients may require temporary placement in a nursing home or rehab facility when there are doubts about the safety of their ability to function independently without the use their arm.
Ultimately, because the most important aspect of history gathering in patients with suspected proximal humerus fracture surrounds the circumstances that led to the injury, falls in the elderly are often sentinel events that reveal undiagnosed medical conditions and/or unsafe home environments.9
Physical Exam
Physical examination of the shoulder should focus on evaluating the integrity of the skin, identifying areas of tenderness, noting ecchymoses and/or deformities. A gentle assessment of both active and passive range of motion (ROM) at the shoulder is appropriate, but pain and spasm often limit this in the acute setting. Inability to tolerate any significant shoulder ROM should be expected. Inspect for the “sulcus sign” characterized by increased inferior translation of the humerus below the acromion on the lateral aspect of the shoulder, which may indicate inferior glenohumeral instability.[12] Examine the elbow, forearm, and wrist for associated injuries and the other extremities for painful ROM, swelling, and deformity.
Evaluate the vascular status by palpating the radial and ulnar pulses and check nailbed capillary refill. Assess axillary nerve function by checking sensation over the lateral deltoid.
Assess for the possibility of associated head, neck, and thoracic trauma. Inspect for swelling and ecchymoses. Palpate the cervical spine assessing for midline tenderness and, if present, use appropriate neck immobilization until a cervical spinal (c-spine) fracture can be excluded. It is important to note that neither NEXUS, nor the Canadian C-spine clinical decision rule allow for clearance of patients over age 65 with midline c-spine tenderness. Trauma expert guidelines recommend computed tomography (CT) of the c-spine over XR in elderly patients.[13] In UC, this often will necessitate an ED referral by ambulance. Palpate the chest assessing for crepitus and tenderness that might suggest the possibility of rib fracture, chest wall contusion, and need to obtain imaging to assess for PTX or hemothorax.
Finally, do not lose sight of the cause of the patient’s injury. Assess the safety and stability of the patient’s gait. If there is concern for an acute medical condition (eg, syncope, ACS, PE, CVA) contributing to a fall based on the history, perform appropriate physical examinations to assess for the presence of the underlying conditions in the differential.
Radiography
The primary imaging modality for diagnosing proximal humerus fractures is plain radiography (ie, XR). It is recommended to obtain a true anteroposterior (AP) view of the glenohumeral joint, an axillary view, and a scapular-Y view as the patient can tolerate which assesses both the glenohumeral joint and the proximal humerus.[14] Provide oral analgesia, such as acetaminophen, and an ice pack prior to obtaining XRs to allow for maximal patient comfort and the most appropriate positioning.
Although XR are the initial imaging of choice, occasionally CT may be obtained if operative repair is considered.14 Point-of-care ultrasound (POCUS) can be utilized as a complementary imaging modality and has high sensitivity and specificity in the hands of experienced operators in diagnosing long bone fractures and determining fracture characteristics. However, POCUS is not commonly available in UC settings, and XR usually is able to identify most proximal humerus fractures (Image 3).[15] While magnetic resonance imaging (MRI) is rarely indicated, it may ultimately be considered by a specialist seeing the patient for follow-up if there is concern for associated rotator cuff injuries.14
Two main classification systems exist to categorize proximal humerus fractures: the Neer classification; and the AO (Arbeitsgemeinschaft für Osteosynthesefragen) classification.14
- The Neer classification categorizes fractures based on the number of separated anatomical segments. Separation is defined as angulation greater than 45° or displacement >1 cm. This system accounts for deforming forces, vascular status of the fragments, and continuity of the articular surface.14
- The AO classification divides proximal humeral fractures into 3 groups (A-C) based on the number of fracture parts, with further subgroups specifying the anatomic location of the fractures.14 This system also assesses the risk of avascular necrosis, with group A having the lowest risk and group C the highest.14

Management in Urgent Care
Provide analgesics, a shoulder sling, and ice pack immediately as able and obtain appropriate imaging as discussed. After identifying a proximal humerus fracture on XR and clinically excluding significant other injury or acute underlying medical issues that would require immediate ED referral, it is appropriate to focus on treatment of the patient’s shoulder injury. The immediate treatment of proximal humerus fractures depends on the severity and type of fracture as well as the presence of complications. Open fractures and those with neurovascular involvement, though rare, should be immediately referred to an ED.[16] ED referral is also warranted if there is suspicion for elder abuse.
Fractures with mild and even moderate displacement are typically treated nonoperatively.[17] The 2015 ProFHER (PROximal Fracture of the Humerus: Evaluation by Randomisation) trial, a randomized multi-center study of 250 patients with displaced proximal humerus fractures, compared surgical and non-surgical treatments and found no significant difference in functional outcomes between surgical and non-surgical groups. However, the surgical group experienced more medical complications compared to those treated conservatively, suggesting risks beyond surgical complications need to be considered in this generally frail group of patients who often have multiple co-morbidities.17
Conservative management consists of the use of a simple shoulder sling for 4-6 weeks and early physical therapy (PT). Pendulum and passive range of motion exercises should begin as soon as pain allows to maintain ROM and prevent stiffness.[18] The sling can generally be removed for bathing and hygiene. Active ROM and strengthening exercises will be guided by PT and orthopedics. The main risks of nonoperative management include osteonecrosis, non-union or malunion, joint stiffness, and rotator cuff dysfunction.[19]
For patients that can be safely discharged from UC, ensuring adequate home support and analgesia are primary considerations. Oral opioid analgesics (eg. hydrocodone, oxycodone etc.) have been considered integral to the treatment of pain associated with fractures. However, increasing awareness of opioid use disorders has prompted consideration for opioid sparing strategies for post-traumatic pain management.[20] Further caution is warranted when prescribing opioids to older patients, particularly those who may have fallen due to balance issues and/or intoxication, as opioid use can exacerbate fall risk. Non-steroidal anti-inflammatory (NSAID) agents (eg, naproxen and ibuprofen) are effective analgesics, but concerns in the orthopedic community have been raised regarding NSAID use and impaired fracture healing. However, there is growing evidence that NSAID use likely does not impair bone healing to a clinically relevant degree, with a 2020 observational study even showing a greater risk of malunion among patients taking opioids and not among those taking non-selective NSAIDs.[21],[22] This has led to adoption of a recommendation for use of NSAIDs as a primary analgesic class for treatment of acute fracture related pain by the Eastern Association of Surgeons for Trauma (EAST) in their updated 2023 guidelines.20 It is important to assess for contraindications for NSAIDs, especially in elderly patients, and use the safest agent, at the lowest dose, for the shortest duration possible.[23] The preponderance of current evidence supports a multimodal analgesia (ie, combining classes of analgesics for synergy) strategy as the most safe and effective for fracture pain management.[24] This strategy complements a tiered approach which emphasizes initial pain management strategies should be non-pharmacologic (eg, ice, sling) and then adding pharmacologic agents in order of their safety profiles.[25]
In proximal humerus fractures, for example, such a pain management strategy could consist of using ice or heat liberally with acetaminophen 1,000mg every 8 hours. Naproxen 250-500mg once or twice daily could then be added if necessary followed by a low dose of oxycodone (eg, 2.5-5mg) as needed for breakthrough pain for the first 3-5 days after injury. Patients discharged from UC should be urgently referred for outpatient orthopedic evaluation and PT. Additional pain management can be deferred to the orthopedist as they would ideally be seeing the patient for follow-up within 5 days. This is also the best setting for further discussions surrounding any need for additional imaging and the risks and benefits of surgical fixation.
Disposition and Outcome
The patient was able to ambulate safely and felt comfortable going home with his daughter. He was placed in a simple shoulder sling, prescribed hydrocodone for breakthrough pain, and referred to orthopedics. Two days later, his daughter found him on the floor and minimally responsive. He was intubated for airway protection and taken to the local ED where a stat head CT demonstrated a large subdural hemorrhage. He also had laboratory evidence of rhabdomyolysis with evidence of acute renal failure. His blood ethanol level was found to be 0.15% at the time of his presentation. After a prolonged inpatient course involving neurosurgical intervention and aggressive intravenous fluid administration, his acute kidney injury resolved and his mental status improved. He remained confused, however, and therefore was discharged to a skilled nursing and rehabilitation facility.
His proximal humerus fracture was treated nonoperatively. He remained in a sling for 4 weeks and received progressive PT to gain strength and ROM while in the facility.
Takeaways for Urgent Care
- Proximal humerus fractures most commonly occur in older patients after a fall onto their shoulder.
- Assess the shoulder and remainder of the upper extremity for associated injuries.
- The axillary nerve is the most likely neurovascular structure to be injured in the setting of proximal humerus fracture. Screening for axillary nerve injury can be accomplished by assessing sensation over the lateral deltoid.
- Both displaced and nondisplaced proximal humerus fractures are typically managed conservatively with a simple shoulder sling, early passive ROM, and physical therapy.
- XR imaging can usually confirm the presence of a proximal humerus fracture. Additional imaging is rarely indicated in the acute setting.
- If the injury is caused by a fall, consider acute medical issues and substance use that can affect balance and evaluate as appropriate based on history and physical exam.
- Specifically evaluate for associated head and c-spine injuries. Elderly patients are at risk for intracranial hemorrhage and c-spine fractures with relatively low-mechanism trauma. Have a low-threshold for ED referral if there is associated head trauma or c-spine tenderness.
- Treat patients with tiered, multimodal analgesia and limit opioid prescriptions to a short-course for breakthrough pain.
- Proximal humerus fractures can be sentinel events for elderly and frail individuals that offer an opportunity to identify undiagnosed medical conditions or unsafe home environments. A diligent assessment of the patient’s baseline status, function, and home environment after can reduce subsequent morbidity and mortality.
Manuscript submitted September 18, 2024; accepted October 3, 2024.
Author Affiliations: Lauren Schuermann, MS4, Ohio University Heritage College of Osteopathic Medicine. Shivani Kothari, MS4, Ohio University Heritage College of Osteopathic Medicine. Bradley Strauch, MD, Adena Regional Medical Center. Authors have no relevant financial relationships with any ineligible companies.
References
- [1]. Khmelnitskaya, E., et al., Evaluation and management of proximal humerus fractures. Adv Orthop. 2012: p. 861598.
- [2]. Rudran B., et al., Proximal humerus fractures: anatomy, diagnosis and management. Br J Hosp Med. 2022. 83(7): p. 1-10.
- [3]. Keough N, Lorke DE. The humeral head: A review of the blood supply and possible link to osteonecrosis following rotator cuff repair. J Anat. 2021;239(5):973-982. doi:10.1111/joa.13496
- [4]. Migliorini F, Giorgino R, Hildebrand F, et al. Fragility Fractures: Risk Factors and Management in the Elderly. Medicina. 2021;57(10):1119. Published 2021 Oct 17. doi:10.3390/medicina57101119 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8538459/
- [5]. Jeong JY, Stead T, Kwon J, Carman M, Ganti L. Hill-Sachs Deformity. Orthop Rev. 2022;14(1):31927. Published 2022 Mar 6. doi:10.52965/001c.31927
- [6]. Runser, L.A., R.L. Gauer, and A. Houser, Syncope: Evaluation and Differential Diagnosis. Am Fam Physician. 2017. 95(5): p. 303-312.
- [7]. Vinson DR, Engelhart DC, Bahl D, Othieno AA, Abraham AS, Huang J, Reed ME, Swanson WP, Clague VA, Cotton DM, Krauss WC, Mark DG. Presyncope Is Associated with Intensive Care Unit Admission in Emergency Department Patients with Acute Pulmonary Embolism. West J Emerg Med. 2020 Apr 13;21(3):703-713. doi: 10.5811/westjem.2020.2.45028. PMID: 32421523; PMCID: PMC7234693.
- [8]. Galizia, E.C. and H.J. Faulkner, Seizures and epilepsy in the acute medical setting: presentation and management. Clin Med. 2018. 18(5): p. 409-413.
- [9]. Sri-on J, Tirrell GP, Lipsitz LA, Liu SW. Is there such a thing as a mechanical fall? Am J Emerg Med. 2016;34(3):582-585. doi:10.1016/j.ajem.2015.12.009
- [10]. Kim GS, et al. Understanding the Home Environment as a Factor in Mitigating Fall Risk among Community-Dwelling Frail Older People: A Systematic Review, Health & Social Care in the Community, 2023, 8564397. 2023. https://doi.org/10.1155/2023/8564397
- [11]. Court-Brown CM, Garg A, McQueen MM, et al. The epidemiology of proximal Humeral fractures. Acta Orthop Scand 2001; 72:365–71
- [12]. Cadet ER. Evaluation of Glenohumeral Instability. Orthopedic Clinics of North America. 2010. 41(3): p. 287-295.
- [13]. Garg B, Ahuja K. C-spine clearance in poly-trauma patients: A narrative review [published correction appears in J Clin Orthop Trauma. 2021 Oct;21:101559. doi: 10.1016/j.jcot.2021.101559]. J Clin Orthop Trauma. 2021;12(1):66-71. doi:10.1016/j.jcot.2020.10.020
- [14]. Root KT, et al. The Association between Race and Extended Length of Stay in Low-energy Proximal Humerus Fractures in Elderly Patients. JAAOS. 2024. 32(15): p. e759-e768
- [15]. Avci M, Kozaci N, Tulubas G, Caliskan G, Yuksel A, Karaca A, Doganay F, Etli I. Comparison of Point-of-Care Ultrasonography and Radiography in the Diagnosis of Long-Bone Fractures. Medicina. 2019 Jul 9;55(7):355. doi: 10.3390/medicina55070355. PMID: 31324028; PMCID: PMC6681284.
- [16]. Lim PK, et al., Management of Open Fractures of the Extremities and Pediatrics. JAAOS. 9900: p. 10.5435/JAAOS-D-23-0057.
- [17]. Handoll H, Brealey S, Rangan A, et al. The ProFHER (PROximal Fracture of the Humerus: Evaluation by Randomisation) trial – a pragmatic multicentre randomised controlled trial evaluating the clinical effectiveness and cost-effectiveness of surgical compared with non-surgical treatment for proximal fracture of the humerus in adults. Health Technol Assess. 2015;19(24):1-280. doi:10.3310/hta19240.
- [18]. Schumaier A, Grawe B. Proximal Humerus Fractures: Evaluation and Management in the Elderly Patient. Geriatr Orthop Surg Rehabil. 2018;9:2151458517750516. Published 2018 Jan 25. doi:10.1177/2151458517750516.
- [19]. Baker HP, Gutbrod J, Strelzow JA, Maassen NH, Shi L. Management of Proximal Humerus Fractures in Adults-A Scoping Review. J Clin Med. 2022 Oct 18;11(20):6140. doi: 10.3390/jcm11206140. PMID: 36294459; PMCID: PMC9604576.
- [20]. Murphy PB, et al. Efficacy and safety of non-steroidal anti-inflammatory drugs (NSAIDs) for the treatment of acute pain after orthopedic trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma and the Orthopedic Trauma Association. Trauma Surg Acute Care Open. 2023 Feb 21;8(1):e001056. doi: 10.1136/tsaco-2022-001056. PMID: 36844371; PMCID: PMC9945020.
- [21]. Kim H, et al. Do Nonsteroidal Anti-Inflammatory or COX-2 Inhibitor Drugs Increase the Nonunion or Delayed Union Rates After Fracture Surgery?: A Propensity-Score-Matched Study. J Bone Joint Surg Am. 2021 Aug 4;103(15):1402-1410. doi: 10.2106/JBJS.20.01663. PMID: 34101675.
- [22]. George MD, Baker JF, Leonard CE, Mehta S, Miano TA, Hennessy S. Risk of Nonunion with Nonselective NSAIDs, COX-2 Inhibitors, and Opioids. J Bone Joint Surg Am. 2020 Jul 15;102(14):1230-1238. doi: 10.2106/JBJS.19.01415. PMID: 32675672; PMCID: PMC7508275.
- [23]. Bill H. McCarberg, NSAIDs in the Older Patient: Balancing Benefits and Harms. Pain Medicine. Volume 14, Issue suppl 1, December 2013, Pages S43–S44
- [24]. Hsu JR, Mir H, Wally MK, Seymour RB; Orthopaedic Trauma Association Musculoskeletal Pain Task Force. Clinical Practice Guidelines for Pain Management in Acute Musculoskeletal Injury. J Orthop Trauma. 2019;33(5):e158-e182.
- [25]. Amaechi O, Huffman MM, Featherstone K. Pharmacologic Therapy for Acute Pain. Am Fam Physician. 2021 Jul 1;104(1):63-72. PMID: 34264611.
Download the Article PDF: Urgent Care Recognition and Management of Proximal Humerus Fractures
