Published on
Urgent Message: Diverticulitis is a prevalent condition characterized by localized inflammation most commonly of the sigmoid colon. It is often diagnosed with a computed tomography scan with intravenous contrast. Uncomplicated cases are most common and require only monitoring, however complicated cases can require hospitalization and emergent surgical intervention. Urgent care clinicians should be comfortable assessing patients with possible diverticulitis and recognizing features that suggest the possibility of more complicated disease.
Naushair Hussain DO; Shahmeer Hussain DO; Michael Weinstock MD
Citation: Hussain N, Hussain S, Weinstock M. Urgent Care Assessment of Patients with Possible Diverticulitis. J Urgent Care Med. 2024; 19(3): 29-34
Introduction
The most common presenting symptom of diverticulitis is left lower quadrant abdominal pain, with associated symptoms of fever, nausea, and a change in bowel habits.[1] About 20% of patients who experience diverticulitis will have at least 1 recurrence.[2] The incidence of diverticulitis increased over 60% from 1980-2007,[3] and as management guidelines have become increasingly conservative, the rate of emergent surgical intervention has steeply declined.2
Diverticular Disease vs Diverticulosis vs Diverticulitis
Diverticulitis and diverticulosis are related conditions involving diverticula, small herniations that can form in areas of weakness in the muscular layer of the wall of the bowel, most commonly the colon. Diverticulosis refers to the presence of these pouches without inflammation or infection. Diverticulosis is often asymptomatic and may be discovered incidentally during diagnostic tests for other conditions (eg, colonoscopy, computed tomography [CT] scan). In contrast, diverticulitis occurs when these pouches become inflamed or infected, leading to characteristic symptoms.1 Diverticulosis alone does not require treatment unless complications arise; diverticulitis, however, may necessitate medical intervention, including antibiotics, dietary modifications, and in severe cases, surgery.1
Causes of Diverticular Disease
The pathophysiology of diverticular disease is complex, multifactorial, and incompletely understood. Western nations experience higher rates of diverticular disease, which is hypothesized to be related to dietary factors primarily, such as low fiber intake. This leads to higher intracolonic pressure, which predisposes to herniations of the colonic mucosa through the muscular layer, resulting in the formation of diverticula. Fecal stasis in the colon increases the risk of diverticular inflammation, culminating in diverticulitis.2 Patients with diets rich in fiber, low in red meat (less than 51g/day), and higher levels of physical activity have lower rates of diverticulitis.[4],[5]
While dietary choices influence the likelihood of developing diverticular disease, environmental, microbiome, and genetic factors are also believed to play significant roles with a heightened prevalence of diverticular disease among obese individuals2 and smokers.5 This association may be attributed to the inflammatory effects induced by smoking and obesity. Diverticular disease affects men more often than women, and incidence peaks in the 6th decade of life. In elderly populations, diverticulitis becomes more common among women.2
Uncomplicated vs Complicated Diverticulitis Disease
It is important to distinguish between complicated and uncomplicated diverticulitis, as treatment differs considerably. Uncomplicated diverticulitis involves localized inflammation, whereas complicated diverticulitis—which represents <15% of cases of acute diverticulitis—involves progression to abscess, perforation, or phlegmon. Late complications include peritonitis, bowel obstruction, and fistulae formation.[6]
Clinical History and Physical Exam
In the urgent care (UC) setting, laboratory testing and advanced imaging is often not available, therefore bedside clinical assessment is important for assessing the likelihood of diverticulitis. Acute diverticulitis often involves a gradual onset of progressive lower abdominal pain.6 The presence of localized pain solely in the left lower quadrant is the most common symptom of diverticulitis with other possible symptoms including fever, change in bowel habits, and nausea without vomiting.1
Additional history gathering should include history of diverticulitis or diverticulosis, therapies attempted prior to evaluation (eg, acetaminophen, non-steroidal anti-inflammatory drugs [NSAIDs] etc.), exacerbating and relieving symptoms, history of past colonoscopy and any relevant findings, and unintentional weight loss. Other potentially helpful information may include comorbid conditions such as immunocompromise, known abdominal aortic aneurysm or history of kidney stones. Dietary habits, history of smoking, and family medical history may also be helpful to discuss.3
As with all UC presentations, objective assessment begins with reviewing the patient’s vital signs. The presence of fever, hypotension, and/or tachycardia in patients with lower abdominal pain significantly increase the likelihood of complicated diverticulitis.[7] Examination of the abdomen should include inspection for distention, surgical scars, hernias etc. Palpation of the abdomen should assess for areas of focal tenderness. Focal tenderness in the left lower quadrant is the most suggestive physical exam finding with a positive likelihood ratio of 10.4 when present.6 Presence of peritoneal signs such as rebound tenderness, Rovsing’s sign, and/or guarding should raise suspicion for other diagnoses or complicated diverticulitis.7 A screening genitourinary (GU) examination is also prudent to ensure there are no obvious hernias or other scrotal abnormalities.
Differential Diagnosis for Acute Lower Abdominal Pain
Gastrointestinal3
- Bowel obstruction
- Colitis
- Colon cancer
- Appendicitis
- Inflammatory bowel disease
- Irritable bowel syndrome
- Hollow viscus perforation
- Pancreatitis
Gynecologic3
- Ectopic pregnancy
- Endometriosis
- Ovarian cyst
- Pelvic inflammatory disease
- Ovarian torsion
- Tubo-ovarian abscess
Vascular3
- Abdominal aortic aneurysm
Urinary3
- Ureterolithiasis
- Cystitis
Diagnostic Evaluation
The UC assessment focuses on clinical assessment (ie, history and physical). Urinalysis can be helpful if considering GU diagnoses, such as urinary tract infection. Laboratory testing and imaging are not required for the diagnosis if history and exam are strongly suggestive of acute diverticulitis but may occasionally be suggestive of alternate diagnoses. A complete blood count (CBC), basic metabolic panel, liver function tests, lipase, and/or inflammatory markers can be considered, but it’s important to note that these lab tests are neither sensitive or specific for diverticulitis.6 For example, approximately 45% of patients with diverticulitis will not have leukocytosis3. A C-reactive protein (CRP) level can offer some augmentation of clinical assessment. A level exceeding 20mg/dL is suggestive of perforation, and a combination of CRP level above 5mg/dL with isolated left lower quadrant tenderness and absence of vomiting has a specificity of 93-98% for diverticulitis, albeit with a sensitivity of only 37%.3
A qualitative urine β-HCG for women of child-bearing age is an easy test and relatively reliable for excluding the possibility of pregnancy, including ectopic.[8] In cases where uncertainty persists or complicated diverticulitis is suspected, immediate imaging is warranted. Intravenous (IV) contrast-enhanced CT is the study of choice and has a sensitivity of 94% and specificity of 99%.3 Abdominal CT is not only helpful to “rule in” diverticulitis but is also highly sensitive and specific for alternative diagnoses that may require alternate management strategies (eg, appendicitis, ureterolithiasis).[9] Abdominal magnetic resonance imaging (MRI) is an alternative to CT and has similar sensitivity, however, obtaining rapid MRI is often more challenging in most clinical settings.[10] Ultrasound (US) as diagnostic modality relies heavily on the operator’s experience, and its ability to assess for free air or the extent of large abscess is limited. Additionally, US is unable to detect other pathologies as readily.1 In experienced hands, it may be reasonable to get an US if it is the only advanced imaging immediately available, as an emergency department (ED) study demonstrated sensitivity similar to that of CT (90% vs 95%).9 In cases of inconclusive US, CT is often necessary for patients with concerning signs and symptoms of complicated diverticulitis or other acute abdominal pathology that may necessitate intervention.9
Classification of Diverticulitis Based on the Hinchey Scale
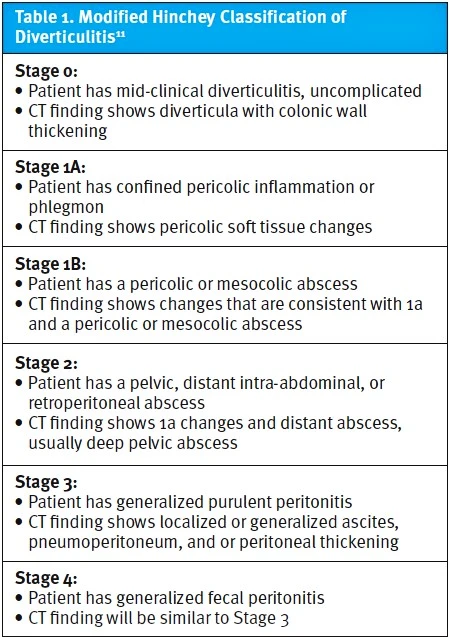
The Hinchey Scale has been the most widely utilized severity classification system for acute diverticulitis over the past 30 years.9 The modified Hinchey classification (Table 1), which includes CT findings, such as signs of inflammation, abscess, and perforation, may further help to risk stratify diverticulitis presentations and ensure appropriate treatment.[11] Recommendations for the management of uncomplicated diverticulitis (ie, modified Hinchey stage 0/1a) are for conservative treatment and discretionary use of oral antibiotics based on patient factors (eg, underlying health status, immunocompromise). Importantly, the American Gastroenterological Association (AGA) does not use the Hinchey Scale in their clinical practice guidelines updated in 2021 and favors grading severity from mild to severe. The AGA similarly advocates for selective use of antibiotics in mild, uncomplicated diverticulitis in immunocompetent patients.1 Complicated cases of diverticulitis, typically falling within modified Hinchey stage 1b-IV, require appropriate antibiotic therapy and often inpatient admission. Procedural intervention depends on evaluation from a surgeon to determine if abscess drainage or exploratory laparoscopic or open laparotomy may be indicated depending on severity of illness, patient factors, and the presence of peritonitis.[12]
Red Flag Symptoms
Red flag symptoms of diverticulitis warranting surgical intervention include but are not limited to peritoneal signs indicative of perforation. Additional concerning symptoms may involve fecaluria, pneumaturia, and pyuria, which raise suspicion for a colo-vesical fistula. Similarly, the presence of stool in the vagina may suggest a potential colo-vaginal fistula.1
Management
Uncomplicated Diverticulitis
Patients with uncomplicated acute diverticulitis who can tolerate oral intake should be placed on a clear liquid diet initially and then treated conservatively as outpatients with follow-up arranged within 7 days of diagnosis to ensure condition is improving.5,9
Antibiotics have traditionally served as the cornerstone of treatment for patients presenting with acute diverticulitis, whether complicated or not. However, recent research has cast doubt on their necessity, particularly in cases of uncomplicated diverticulitis. Multiple specialty societies, such as the American Society of Colorectal Surgery and AGA, have concluded that there is no obvious improvement in outcomes between patients treated with or without antibiotics.2,[13] In the DIABOLO trial, the long-term effects of managing patients without antibiotics in uncomplicated acute left-sided diverticulitis were assessed after 24 months, finding no difference in rates of recurrent diverticulitis.9 Similar findings were demonstrated in the Antibiotics Uncomplicated Diverticulitis (AVOD) trial where no difference in long-term outcomes were noted for patients treated with or without antibiotics.[14]
If antibiotic therapy is deemed clinically appropriate by the diagnosing clinician, it is also noteworthy that IV antibiotics have not been shown to be more effective than oral antibiotics, and oral antibiotics offer obvious advantages of decreased cost and outpatient treatment.9 A small randomized controlled trial comparing oral vs IV therapy with ciprofloxacin and metronidazole for clinically diagnosed uncomplicated diverticulitis showed no difference in resolution with all patients in both groups recovering without complication.7
It’s important to note that the recommended antibiotic therapies are broad spectrum to cover for gram-negative and anaerobic organisms. Either a fluoroquinolone plus metronidazole or amoxicillin-clavulanate at standard doses for as little as 4 days (or up to 7 days in higher risk patients) is acceptable.1 Given inherent risks of broad-spectrum antibiotic therapy (eg, C. difficile colitis, antibiotic-associated diarrhea) and neurologic toxicities associated with metronidazole and fluoroquinolones, as well as limited evidence of benefit of antibiotic therapy in uncomplicated diverticulitis, it is prudent to prescribe the shortest course of appropriate antibiotics to minimize risk of unnecessary harms.[15],[16]
Complicated Diverticulitis
Intra-abdominal abscess formation occurs in 15-40% of patients who present with acute sigmoid diverticulitis.13 All patients in which there is concern for complicated diverticulitis warrant immediate ED referral. Patients in whom complicated diverticulitis is confirmed are placed on complete bowel rest (NPO) and hydrated with IV fluids.5 Treatment options differ based on the size of the abscess. In cases where an abscess is >3cm, then antibiotics with image-guided percutaneous drainage is recommended.13
Immunocompromised Patients With Acute Diverticulitis
In immunocompromised patients, diverticulitis can become complicated rapidly as these patients are more likely to fail nonoperative treatment.9 Immunocompromised patients may present with more subtle findings even in complicated cases because of blunted responses to infection and inflammation (eg, fever, signs of peritoneal irritation).1
One study examined 5 types of immunocompromised patient populations: chronic corticosteroid users; transplant patients; patients undergoing cancer treatment; patients with chronic kidney disease; and other immunosuppressant treatments. The results demonstrated that immunosuppressed patients had higher rates of emergency surgery and postoperative mortality.9 Since immunocompromised patients are at higher risk of more subtle and delayed presentation, antibiotic treatment is recommended for these patients, even in apparently mild cases.9 Caution should be exercised in relying on clinical assessment alone for such patients, and it is appropriate to have a lower threshold to refer these patients to an ED if CT imaging is not immediately available.1 Additionally, even in cases of mild or uncomplicated diverticulitis, the duration of antibiotic therapy recommended is longer (10-14 days), albeit similar agents can be used to ensure gram-negative and anaerobic coverage.1
Evaluation After Recovery From Acute Diverticulitis
The AGA best practice guidelines from 2021 reiterate the critical nature of colonoscopy after many cases of diverticulitis.1 Specifically, colonoscopy is recommended following the resolution of any episode of complicated diverticulitis or a first episode of uncomplicated diverticulitis, unless a full, high-quality colonoscopy was done in the prior year.1 The basis for this recommendation is that occult colonic neoplasms can be mistakenly diagnosed on CT as diverticulitis with relatively high frequency.1,13 To minimize the risk of procedure-related perforation, this evaluation is typically scheduled after 6-8 weeks from the acute episode.1
Elective Surgery for Recurrent Diverticulitis
In the landscape of diverticulitis management, elective segmental colectomy emerges as a strategy to temper rather than eliminate the risk of recurrence. Though surgical intervention has its merits, and some guidelines do recommend interval elective surgery, there is an emerging sentiment that a more conservative and personal approach may be safer.1 Insight from longitudinal studies underscores this point, revealing that at the 5-year follow-up interval, recurrent diverticulitis was documented in only 15% of patients who underwent elective surgery, in stark contrast to the 61% recurrence rate observed in those managed nonoperatively.1 However, despite the intervention, lingering symptoms following recovery from acute diverticulitis persist as a notable concern. Intriguingly, colectomy often falls short in addressing these symptoms, as indicated by findings from 2 separate studies where 22% to 25% of patients continued to grapple with ongoing abdominal discomfort post-surgery.1 From a UC perspective, clinicians should avoid any specific suggestion that surgery may or may not be appropriate and instead focus on ensuring timely referral to a colorectal surgeon who can outline the risks and benefits for the individual patient.
Diagnostic Case Scenarios
Case 1
- History and Physical Exam: A 40-year-old woman presented to UC with 3 days of dull, progressive, crampy left lower quadrant abdominal pain with intermittent episodes of nausea but no vomiting. She denied fever, dysuria or frequency, vaginal bleeding or discharge, blood in the urine or stool. Her past medical history was noncontributory. Her temperature was 37.5°C and heart rate (HR) was 95 beats per minute (bpm). Exam shows localized tenderness in the left lower quadrant with no rebound or guarding.
- UC Testing: Her dip urinalysis and urine human chorionic gonadotropin were negative.
- Diagnosis and Management: She was diagnosed clinically with uncomplicated acute diverticulitis and was managed with recommendations for a clear liquid diet until pain resolved. Through shared decision making, it was decided to defer antibiotics given the mild nature of her symptoms. She was discharged from the UC with recommendations to follow-up with primary care in a week to monitor for progression and discuss referral for colonoscopy as well as going to the ED for worsening pain or fever.
Case 2
- History and Physical Exam: A 55-year-old man with history of prior episodes of diverticulitis presented to UC with 2-3 days of generalized abdominal pain, which had started in the left lower quadrant. He reported nausea without vomiting. His temperature was 38.1°C with a HR of 103 bpm. He appeared uncomfortable, and his abdominal exam revealed moderate to severe generalized tenderness with associated guarding and rebound.
- Diagnosis and Management: Due to concern of perforation or abscess, he was referred to the ED, where a CT of the abdomen/pelvis with contrast revealed a 2 cm abscess around the sigmoid colon. He was diagnosed with complicated diverticulitis and started on IV antibiotics. Drainage was not required due to the size of the abscess (<3cm). The patient’s pain improved over the next 2 days, and he was discharged on oral antibiotics, plus recommendations to follow up with primary care in 1 week. He had a normal colonoscopy 9 months earlier, and therefore he was not referred to gastroenterology.
Counseling For Patients With Acute Diverticulitis
Constipation and increased colonic intramural pressure contribute significantly to the risk of diverticular formation and diverticulitis.1 Contrary to prior dogmatic teaching, it does not appear that nuts, seeds, corn, or other forms of fibrous dietary intake contribute to the risk of diverticulitis. Patients should be encouraged that a diet high in natural sources of fiber from fruits, vegetables, and legumes is helpful for reducing recurrence risk.[17] Physical activity, similarly, significantly reduces the risk of diverticulitis recurrence.[18] Patients should be counseled to quit smoking, reduce meat consumption, and attempt to lose weight if these risk factors are present.1
Both opioids and NSAIDs increase the risk of diverticulitis recurrence, and as such, acetaminophen is the recommended first line analgesic option for pain management.1,[19] For patients with pain severe enough that acetaminophen offers insufficient analgesia, consider ED referral to ensure that the patient is not suffering from a more complicated episode of diverticulitis or other serious intraabdominal pathology.
Takeaway Points
- Diverticulitis is a common condition marked by inflammation or infection of small, herniated pouches of mucosa, diverticula, in the colon with incidence increasing with age, low-fiber diet, and microbiome/genetic predispositions.
- Management of diverticulitis centers around identification and risk stratification of acute episodes, identifying patients with signs and symptoms of complicated cases, and appropriate ED referral.
- Patients should be encouraged to adhere to a clear-liquid diet during the acute episode and monitor symptoms closely; counseling to seek immediate ED evaluation for increasing pain and/or fever is important for patients discharged from UC.
- Antibiotics are recommended selectively in patients with immunosuppression or more significant disease. In patients with mild, uncomplicated diverticulitis, antibiotics may be used selectively for a short duration (4-7 days), and risks vs benefits should be discussed with patients, ensuring that the shortest and lowest risk therapies are used when prescribing antibiotics for mild cases.
- Improving long-term outcomes and reducing risk of recurrence relies on counseling to increase dietary fiber intake and physical activity. NSAIDs, opioids, red meat consumption, and obesity all increase the risk of recurrence.
- In more severe/complicated cases, abscess formation, fistulae, or peritonitis may occur requiring surgical intervention.
- CT imaging with contrast is the study of choice in cases where there is diagnostic uncertainty or concern for complicated disease.
- Colonic neoplasms can be misdiagnosed as diverticulitis. Patients with diverticulitis who have not had a colonoscopy in the last year should be referred to a colorectal specialist to determine if colonoscopy and/or elective partial colectomy is indicated after the resolution of the acute episode.
Manuscript submitted September 30, 2024; accepted November 1, 2024.
References
- [1]. Peery AF, Shaukat A, Strate LL. AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review. Gastroenterology. 2021;160(3):906-911.e1. doi:10.1053/j.gastro.2020.09.059
- [2]. Strate LL, Morris AM. Epidemiology, Pathophysiology, and Treatment of Diverticulitis. Gastroenterology. 2019;156(5):1282-1298.e1. doi:10.1053/j.gastro.2018.12.033
- [3]. Bailey J, Dattani S, Jennings A. Diverticular Disease: Rapid Evidence Review. Am Fam Physician. 2022 Aug;106(2) 150-156. PMID: 35977135
- [4]. Garfinkle R, Sabboobeh S, Demian M, Barkun A, Boutros M; Management of Uncomplicated Diverticulitis (MUD) Collaborative. Patient and Physician Preferences for Antibiotics in Acute Uncomplicated Diverticulitis: A Delphi Consensus Process to Generate Noninferiority Margins. Dis Colon Rectum. 2021;64(1):119-127. doi:10.1097/DCR.0000000000001815
- [5]. Koprowski MA, Affleck A, Tsikitis VL. Emerging evidence and recent controversies in diverticulitis: a 5-year review. Ann Gastroenterol. 2022 Jan-Feb;35(1):8-16. doi: 10.20524/aog.2021.0677. Epub 2021 Nov 11. PMID: 34987283; PMCID: PMC8713340.
- [6]. Laméris W, van Randen A, van Gulik TM, et al. A clinical decision rule to establish the diagnosis of acute diverticulitis at the emergency department. Dis Colon Rectum. 2010;53(6):896-904.
- [7]. Al-Saadi H, Abdulrasool H, Murphy E. Evaluation of Clinical Assessment in Predicting Complicated Acute Diverticulitis. Cureus. 2023;15(2):e34709. Published 2023 Feb 6. doi:10.7759/cureus.34709
- [8]. Larraín D, Caradeux J. β-Human Chorionic Gonadotropin Dynamics in Early Gestational Events: A Practical and Updated Reappraisal. Obstet Gynecol Int. 2024;2024:8351132. Published 2024 Mar 7. doi:10.1155/2024/8351132
- [9]. Sartelli M, Weber DG, Kluger Y, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15(1):32. Published 2020 May 7. doi:10.1186/s13017-020-00313-4
- [10]. Jerjen F, Zaidi T, Chan S, et al. Magnetic Resonance Imaging for the diagnosis and management of acute colonic diverticulitis: a review of current and future use. J Med Radiat Sci. 2021;68(3):310-319. doi:10.1002/jmrs.458
- [11]. Andeweg CS, Mulder IM, Felt-Bersma RJ, et al. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30(4-6):278-292. doi:10.1159/000354035
- [12]. Tochigi T, Kosugi C, Shuto K, Mori M, Hirano A, Koda K. Management of complicated diverticulitis of the colon. Ann Gastroenterol Surg. 2017;2(1):22-27. Published 2017 Sep 28. doi:10.1002/ags3.12035
- [13]. Hall J, Hardiman K, Lee S, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis Colon Rectum. 2020;63(6):728-747. doi:10.1097/DCR.0000000000001679
- [14]. American College of Surgeons website. Evolving Approaches to Diverticulitis Give Surgeons a Gut Check in Management Options. Bulletin of the American College of Surgeons. 2023; 108(11). Retrieved from https://www.facs.org/for-medical-professionals/news-publications/news-and-articles/bulletin/2023/november-december-2023-volume-108-issue-11/evolving-approaches-to-diverticulitis-give-surgeons-a-gut-check-in-management-options/
- [15]. Morales D, Pacurariu A, Slattery J, Pinheiro L, McGettigan P, Kurz X. Association Between Peripheral Neuropathy and Exposure to Oral Fluoroquinolone or Amoxicillin-Clavulanate Therapy. JAMA Neurol. 2019;76(7):827–833. doi:10.1001/jamaneurol.2019.0887
- [16]. Quickfall D, Daneman N, Dmytriw AA, Juurlink DN. Metronidazole-induced neurotoxicity. CMAJ. 2021;193(42):E1630. doi:10.1503/cmaj.201671
- [17]. Strate LL, Liu YL, Syngal S, Aldoori WH, Giovannucci EL. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300(8):907-914. doi:10.1001/jama.300.8.907
- [18]. Strate LL, Liu YL, Aldoori WH, Giovannucci EL. Physical activity decreases diverticular complications. Am J Gastroenterol. 2009;104(5):1221-1230. doi:10.1038/ajg.2009.121
- [19]. Humes DJ, Fleming KM, Spiller RC, West J. Concurrent drug use and the risk of perforated colonic diverticular disease: a population-based case-control study. Gut. 2011;60(2):219-224. doi:10.1136/gut.2010.217281
Author Affiliations: Naushair Hussain, DO, Indiana University School of Medicine, Indianapolis, Indiana. Shahmeer Hussain, DO, Adena Health Systems, Chillicothe, Ohio. Michael Weinstock, MD, Adena Health System; Wexner Medical Center at The Ohio State University; The Journal of Urgent Care Medicine. Authors have no relevant financial relationships with any ineligible companies.
Download the Article PDF: Urgent Care Assessment of Patients with Possible Diverticulitis

