Published on
What is the pacemaker mode?
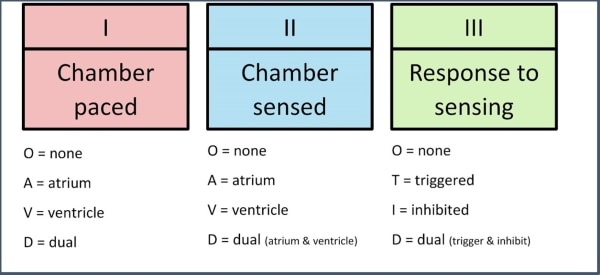
The mode is likely ventricular-sensed, ventricular-paced (VVI). Pacemaker spikes can be visualized in V4/5/6. The atrial contractions are ignored. Pacemakers are programmed with five variables, the first three of which are relevant to urgent care physicians (Figure 2).1,2
What are the indications for pacemaker insertion?
The following is an incomplete list of indications for pacing (either temporary or permanent as the situation warrants), compiled from the 2018 ACC/AHA/HRS guidelines on the evaluation and management of patients with bradycardia and cardiac conduction delay:3,4
- Sinus node dysfunction (Class I)
- Second-degree Mobitz II, high-grade, or third-degree atrioventricular block not attributable to reversible causes (Class I)
- Marked first-degree or second-degree Mobitz type I (Wenckebach) atrioventricular block with symptoms that are clearly attributable to the atrioventricular block (Class IIa)
- Syncope and bundle branch block with evidence of infranodal disease on electrophysiology testing (Class I)
- Alternating bundle branch block (Class I)
- Acute phase of myocardial infarction. Temporary pacing is indicated for refractory or hemodynamically significant bradycardia attributable to sinus node dysfunction or atrioventricular block (Class I). A waiting period is appropriate to determine the need for permanent pacing (Class I)
- Cardiac resynchronization therapy for severe systolic heart failure (Class I)
- Neuromuscular disease. Several neuromuscular diseases are associated with atrioventricular block, including myotonic muscular dystrophy, Kearns-Sayre syndrome, Erb’s dystrophy (limb-girdle), and peroneal muscular atrophy (Class I)
- Long QT syndrome. High-risk congenital long QT syndromes can be treated with pacemakers to prevent ventricular arrhythmias
See the video provided by ECG Stampede for detailed analysis
Pearls for Urgent Care Management
- The most common pacemaker mode is VVI, meaning the ventricle is paced, intrinsic ventricular activity is sensed, and the pacemaker is inhibited if present
- There are no specific urgent management needs if the patient is being paced as expected
- Pacemaker malfunctions include failure to pace, failure to sense, and failure to capture
- In general, patients in whom pacemaker spikes are not conducted resulting in bradycardia, or patients in whom pacemaker spikes are too frequent resulting in tachycardia, should be transferred to a higher level of care
References
- Wagner GS, Strauss DG. Marriott’s Practical Electrocardiography. 12th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014.
- Mulpuru SK, Madhavan M, McLeod CJ, et al. Cardiac pacemakers: function, troubleshooting, and management: part 1 of a 2-part series. J Am Coll Cardiol. 2017;69(2):189-210.
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;140(8):e382-e482.
- Dalia T, Amr BS. Pacemaker Indications. StatPearls Publishing; 2020.
A 100-Year-Old Female Presents with Right Foot Pain
1 2
