Differential Diagnosis
- Hyperkalemia
- ST-elevation myocardial infarction (STEMI)
- Atrial flutter
- Hypokalemia
- Digoxin use
Diagnosis
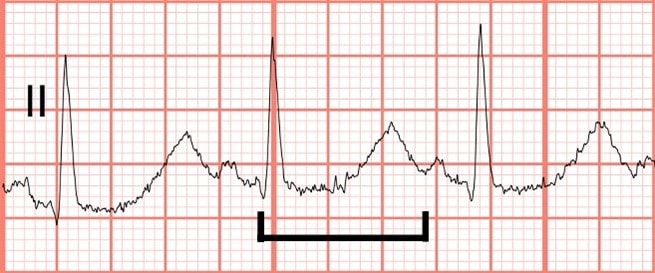
This patient was diagnosed with hypokalemia.The ECG reveals some baseline artifact, a narrow-complex sinus rhythm at a rate of 78 beats per minute, and a normal axis. There are no ST-changes to suggest acute ischemia. The QT interval is prolonged, with a QTc of approximately 660 msec.
Hypokalemia (as well as other electrolyte abnormalities, including hypocalcemia and hypomagnesemia, hypothermia, and many drugs) can cause prolongation of the QT interval. Other changes due to hypokalemia include prolongation of the PR interval, ST depressions, T-wave flattening/inversion, and U-waves. In this example, the T waves in V2 and V3 are likely inverted and fused with U waves, creating the appearance of a biphasic T wave with terminal positivity.
ECG changes due to hyperkalemia include peaked T-waves, P-wave flattening, prolonged PR interval, widened/abnormal QRS morphology, bradyarrhythmias, and a sine wave appearance (see the January 2023 issue of JUCM, pages 47 and 48, for an ECG demonstrating hyperkalemia).
Downsloping, “scooped” ST-segments resembling Salvador Dali’s mustache, are a finding seen in digoxin use but does not necessarily imply toxicity.
Discussion
Hypokalemia, hypomagnesemia, and hypocalcemia can all cause a prolongation of the QT interval. While hypokalemia and hypomagnesemia both delay the repolarization phase (phase 3) of the of the cardiac action potential (creating wide-based T waves, U waves, or a fusion of both), hypocalcemia prolongs the QT interval by way of extending the plateau phase (phase 2) of the cardiac action potential (lengthening the ST segment but with a normal T wave).
Tachycardia is protective in patients with hypokalemia because as the heart rate decreases, the QT interval lengthens. With profound bradycardia and a long QT interval, the heart may depolarize while still in the repolarization phase. We call this an R-on-T phenomenon, and it may cause patients to go into torsades de pointes, a special type of polymorphic ventricular tachycardia. Treatment includes electrolyte replacement, removal of the offending drug, and potentially overdrive pacing at a rate fast enough to eliminate the risk of R on T phenomenon.
Learnings/What to Look for
- With moderate-severe hypokalemia, look for:
- Increased width and amplitude of the P wave
- Prolonged PR interval
- T-wave flattening or inversion
- ST depression
- Prominent U-waves
- Long QT interval
- In severe hypokalemia, patients develop ectopic beats, supraventricular tachyarrhythmias, and eventually ventricular arrhythmias (particularly torsades de pointes)
Pearls for Urgent Care
- Hypokalemia is often accompanied by hypomagnesemia; don’t forget to check and replace both to decrease the risk of ventricular arrhythmias
- Treatment of hypokalemia involves oral supplementation in the urgent care setting, as well as identification and treatment of the underlying cause of the electrolyte disorder
- Transfer for parenteral potassium administration is indicated when the QT interval is >500 msec, as these patients are at risk for torsades de pointes
- In patients with ECG and laboratory findings consistent with hypokalemia, consider transfer to telemetry capable facilities
Resources
- Diercks DB, Shumaik GM, Harrigan RA, et al. Electrocardiographic manifestations: electrolyte abnormalities. J Emerg Med. 2004;27(2):153–160.
- Glancy DL, Wiklow FE, Rochon BJ. Electrocardiogram after 2 weeks of diarrhea. Proc (Bayl Univ Med Cent). 2010;23(2):173–174.
- Levis JT. ECG diagnosis: hypokalemia. Perm J. 2012;16(2):57.

