Published on
Differential Diagnosis
- Pulmonary embolus
- Right ventricular hypertrophy
- Right bundle branch block
- Anterior STEMI
- Myocarditis
- Hyperkalemia
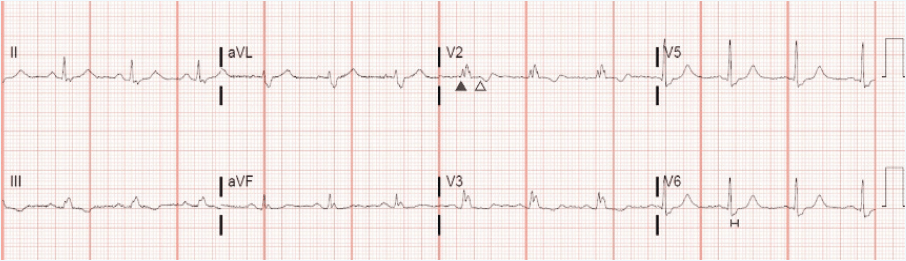
Anterior precordial lead V2 shows “M”-shaped RSR’ pattern (▲) (long arrows) and associated repolarization changes (∆). Lateral leads I and V6 show S-wave >40ms
Diagnosis
This patient was diagnosed with a right bundle branch block (RBBB). The ECG demonstrates normal sinus rhythm at a rate of 78bpm. The QRS duration is prolonged, measuring >120ms. The QRS appearance is “M”-shaped in the anterior precordial leads (V1-V3) and there is a slow, slurred S-wave with a duration exceeding 40ms in the lateral leads (I, aVL, V6).
These changes are caused by a right bundle branch block (RBBB). In a RBBB, the conduction of the left bundle branch is unaffected, resulting in a normal appearance of the early part of the QRS complex. Delayed right-ventricular activation results in a second R-wave (R’) in the anterior precordial leads (producing the RSR’ or “M”-shaped appearance) and also causes the slurred appearance of the S-wave in lateral leads.
As occurs with other depolarization disturbances, repolarization changes are common including ST-segment deviations (typically minimal and discordant with the QRS vector) and T-wave changes (similarly discordant) resulting in the T-wave inversions seen in anterior precordial leads.
RBBB can occur in normal hearts and is a benign finding in an otherwise healthy patient. However, the differential diagnosis includes ominous considerations such as processes resulting in acute or chronic elevations in right ventricular pressure (pulmonary embolus, pulmonary hypertension). Other causes include myocardial ischemia or inflammation (such as myocarditis), as well as intrinsic conduction system disease.
As a result, the clinical relevance of RBBB is variable. While the presence of an RBBB may be associated with increased rates of heart failure, pacemaker requirement, and even all-cause mortality over longer periods of time, in the urgent care setting the focus remains on the identification of an acute or progressive precipitant.1,2 For asymptomatic and otherwise-healthy patients, a careful history and physical examination to evaluate for causes of right ventricular strain (pulmonary embolus, pulmonary hypertension, or other cardiomyopathies) or features suggestive of cardiac ischemia is sufficient.
Learnings/What to Look for:3
- QRS duration >120ms
- RSR’ in V1 or V2
- S-wave of greater duration than R-wave or 40ms in leads I, V6
- An “incomplete” RBBB matches the same diagnostic criteria with a QRS duration between 110-120ms
Pearls for Urgent Care Management and Considerations for Transfer
- Evaluate for acute or progressive precipitant of right ventricular strain such as pulmonary embolus, pulmonary hypertension, cardiomyopathy or ischemia
- The presence of a RBBB does not interfere with the usual diagnosis of a myocardial infarction
References:
- Rasmussen P, Skov M, Ghouse J, et al. Clinical implications of electrocardiographic bundle branch block in primary care. Heart. 2019;105(15):1160-1167.
- Sumner G, Salehian O, Yi Q, et al. The prognostic significance of bundle branch block in high‐risk chronic stable vascular disease patients: a report from the HOPE trial. J Cardiovasc Electrophysiol. 2009;20(7):781-787.
- Surawicz B, Childers R, Deal B, Gettes L. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram Part III: Intraventricular Conduction Disturbances A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53(11):976-981.
