Differential Diagnosis
- Ventricular pacing
- Ventricular preexcitation (Wolff-Parkinson-White)
- Accelerated idioventricular rhythm
- Bifascicular block
- Hyperkalemia
Diagnosis
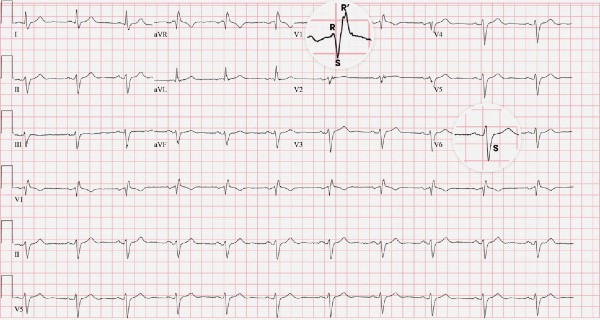
The ECG shows a normal sinus rhythm at a rate of 66 bpm. There is leftward axis deviation with normal PR/QT intervals and a widened QRS complex (>120ms). There are no overt signs of ischemia.
This patient was diagnosed with a bifascicular block.
When evaluating the cause of the widened QRS, we note an RSR’ in the anterior precordial leads (V1, V2), as well as a deep S-wave in the lateral leads (I, V6) suggestive of a right bundle branch block (RBBB) (Figure 2). This finding does not, however, explain the leftward axis deviation as isolated right bundle branch blocks maintain normal activation of the left ventricle (the predominant contributor to the QRS axis). Other causes of leftward axis deviation are absent: 1) There is no left bundle branch block or paced rhythm; 2) no q-waves are identified to suggest inferior myocardial infarction; 3) no criteria for left ventricular hypertrophy are met; and 4) there are no signs of ventricular preexcitation (WPW).
In this case, the leftward axis deviation points to the disruption of another infranodal conduction pathway—the left anterior fascicle.
The normal infranodal conduction divides into the right and left bundles; the latter is further subdivided into anterior and posterior divisions or “fascicles” (Figure 3). Disruption of both fascicles produces the familiar left bundle branch block (LBBB) pattern, but each fascicle can be affected independently, resulting in either left anterior fascicular block (LAFB) or left posterior fascicular block (LPFB).
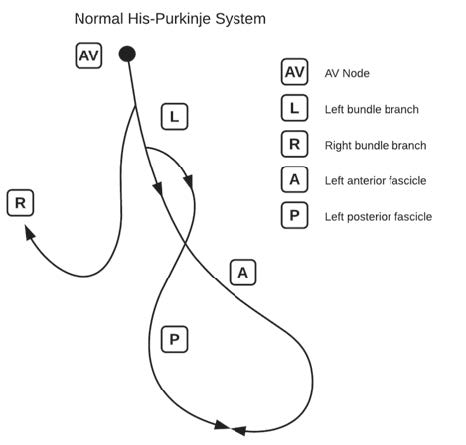
When the left anterior fascicle is disrupted, current passes along the posterior fascicle and the left ventricle is depolarized in a leftward/upward direction, producing left axis deviation (and often an extreme left axis deviation, ie, more than 45° of leftward deviation). Conversely, an LPFB results in depolarization in a rightward/downward direction and produces right axis deviation.
Our patient’s ECG demonstrates disruption of two fascicles, the right bundle and the left anterior fascicle, and is termed a “bifascicular” block. While theoretically a left bundle branch block affects two fascicles, the term is reserved for the combination of an RBBB with LAFB or LPFB.
The clinical significance of bifascicular blocks is heavily dependent on the clinical context. As discussed previously, infranodal conduction disturbances can suggest structural heart disease. However, the rates of progression to dysrhythmias warranting intervention (eg, complete heart block requiring permanent pacemaker placement) are low—particularly in asymptomatic patients.1
Learning/What to Look for
The combination of a right bundle branch block with otherwise unexplained axis deviation suggesting corresponding left anterior or posterior fascicular block defines bifascicular block.
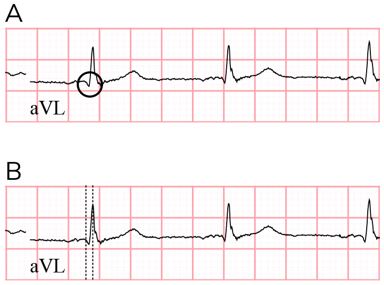
In isolation, left anterior fascicular block (LAFB) are defined by:2
- QRS <120ms
- Left axis deviation (Figure 4)
- qR complexes in leads I, aVL (Figure 5A)
- Prolonged R wave peak time in aVL > 45ms (Figure 5B)

Pearls for Urgent Care Management
For asymptomatic patients with incidental identification of bifascicular blocks, no further evaluation or therapy is indicated. Symptomatic patients (presyncope, syncope) should be transferred for telemetry monitoring, echocardiography, and possible electrophysiologic evaluation.
References
- McAnulty JH, Rahimtoola SH, Murphy E, et al. Natural history of “high-risk” bundle-branch block: final report of a prospective study. N Engl J Med. 1982;307(3):137-143.
- Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association electrocardiography and arrhythmias committee, council on clinical cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the international society for computerized electrocardiology. J Am Coll Cardiol. 2009;53(11):976-981.

