Differential Diagnosis:
- Brugada syndrome
- Left ventricular hypertrophy
- ST-Elevation myocardial infarction (STEMI)
- Wellens syndrome
- Hypokalemia
Diagnosis The ECG illustrates a normal sinus rhythm at 98 bpm. The biphasic T waves with terminal negativity in V2 and V3, minimal ST segment elevation, lack of precordial Q waves, and preserved R wave progression (R wave >3 mm in V3) suggest the presence of Wellens syndrome in this patient with a history of angina who is currently denying chest pain.
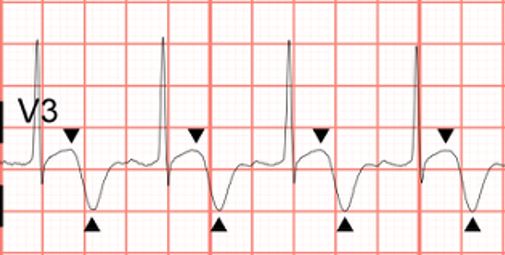
In the correct clinical context, Wellens syndrome represents an ECG pattern seen in patients with critical stenosis of the proximal left anterior descending artery (LAD). The finding of biphasic T waves (type A) or deeply inverted and symmetric T waves (type B) in the anterior precordial leads (V2 and V3) are seen when patients are chest pain-free. These patients are at risk for sudden occlusion of their proximal LAD, and should be considered for urgent catheterization. The T waves are similar in appearance to those seen upon reperfusion by percutaneous coronary intervention (so-called “reperfusion” T waves), leading some to hypothesize that these patients may have had sudden occlusion followed by spontaneous reperfusion. If the artery re-occludes, the patient will develop symptoms and the ECG will first show “pseudonormalization” of the T wave, where it becomes upright and prominent. A persistent re-occlusion will evolve into an anterior ST-elevation myocardial infarction.
The stuttering pain experienced by the patient in our case could have been due to intermittent re-occlusion followed by rapid and spontaneous reperfusion. She was sent to the emergency department where initial testing was negative. The following day, she was taken to the cath lab, where a 99% proximal LAD stenosis was identified and successfully stented.
Learnings/What to Look for:
- Biphasic (type A) or deeply inverted (type B) T waves in V2-3, which may extend to V1-6
- Minimal or no elevation of the ST segment
- Lack of precordial Q waves
- Preserved R wave progression
- Recent history of chest pain, but chest-pain free on evaluation
- May have normal or minimally elevated cardiac enzymes
Pearls for Urgent Care Management and Considerations for Transfer
- Patients with Wellens syndrome have an impending anterior wall myocardial infarction and must be transferred for admission for urgent cardiac catheterization
- Stress test should be avoided, as it may precipitate an acute infarction
- If these patients develop another episode of chest pain while awaiting transfer, repeat their ECG and look for an anterior STEMI or “pseudonormalization” of the anterior T waves—this means they are experiencing an acute re-occlusion of the LAD
Resources
- de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-736.
- Hanna EB, Glancy DL. ST-segment depression and T-wave Inversion: classification, differential diagnosis, and caveats. Clev Clin J Med. 2011;78(6):404–414.
- Mead NE, O’Keefe KP. Wellen’s syndrome: an ominous EKG pattern. J Emerg Trauma Shock. 2009;2(3):206–208.
- Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens syndrome. Am J Emerg Med. 2002;20(7):638-643.
