Differential diagnosis:
- Diffuse subendocardial ischemia
- Hypokalemia
- Left ventricular hypertrophy (LVH) with strain
- ST-Elevation myocardial infarction (STEMI)
- Ventricular tachycardia
Diagnosis
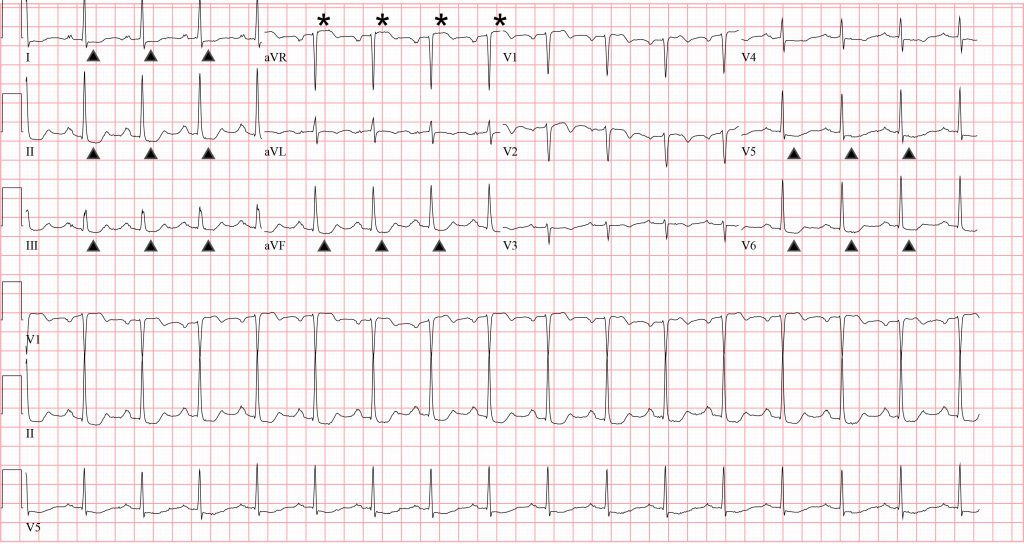
The ECG reveals a regular, narrow-complex, sinus rhythm at a rate of 96 beats per minute. There is a normal axis and normal intervals. There are diffuse ST-segment depressions (identified by the arrows) in the inferolateral leads and >1 mm ST-segment elevation (see asterisks) in aVR. This patient was diagnosed with ST-elevation myocardial infarction (STEMI).
The pattern of diffuse ST-segment depressions with ≥ 1 mm ST-segment elevation in aVR suggests left main coronary artery or triple-vessel disease.1,2 The most recent European Society of Cardiology guidelines recommend emergent reperfusion strategies for these patients in the setting of symptoms consistent with acute coronary syndrome.3
The challenge with this ECG pattern is that it can also be seen in patients not presenting with symptoms of acute coronary syndrome. In one study, 142 ECGs with this pattern were collected and only 28% where associated with acute coronary syndrome.4 Essentially any disease processes that leads to global subendocardial ischemia can present with ECG findings of diffuse ST-segment depressions with ≥ 1 mm ST-segment elevation in aVR, often secondary to supply/demand mismatch in the absence of acute coronary syndrome. Several can’t miss diagnoses can present with this pattern, including pulmonary embolism,5 severe anemia, hypoxia, and shock.4 This pattern can also be seen in tachydysrhythmias where resolution of the ST segment changes is expected after conversion. A similar pattern can also be seen with left ventricular hypertrophy and metabolic disorders, like hypokalemia.6
Learnings/What to Look for
- In the setting of acute coronary syndrome, diffuse ST-segment depressions with ≥1 mm ST-segment elevation in aVR are suggestive of left main coronary artery or significant multivessel disease
- Global subendocardial ischemia can result from any disease process that creates a supply/demand mismatch, including pulmonary embolism, severe anemia, hypoxia, and shock
- This pattern can also be caused by tachydysrhythmias, left ventricular hypertrophy, and hypokalemia
- Compare to a prior ECG when available
Pearls for Initial Management and Considerations for Transfer
- In the setting of acute coronary syndrome, diffuse ST-segment depressions with ≥1 mm ST-segment elevation in aVR warrant emergent transfer to percutaneous coronary intervention capable center
- Consider alternative diagnoses when the patient’s complaint is not consistent with acute coronary syndrome
References
1. Wagner GS, Macfarlane P, Wellens H, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram. Part V: electrocardiogram changes associated with cardiac chamber hypertrophy. Circulation. 2009;53(11):1003-1011.
2. Kosuge M, Ebina T, Hibi K, et al. An early and simple predictor of severe left main and/or three-vessel disease in patients with nonst-segment elevation acute coronary syndrome. Am J Cardiol. 2011;107(4):495-500.
3. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39(2):119-177.
4. Knotts RJ, Wilson JM, Kim E, et al. Diffuse ST depression with ST elevation in aVR: is this pattern specific for global ischemia due to left main coronary artery disease? J Electrocardiol. 2013;46(3):240-248.
5. Witkov RB, Cooper BL. An ominous ECG pattern. Ann Emerg Med. 2019;73(4):406-408.
6. Chua CE, Choi E, Khoo EYH. ECG changes of severe hypokalemia. QJM. 2018;111(8):581-582.
