Differential Diagnosis
- Sinus bradycardia
- First-degree atrioventricular block
- Second-degree atrioventricular block, 2:1 conduction
- Second-degree atrioventricular block, Mobitz type I (Wenckebach)
- Second-degree atrioventricular block, Mobitz type II
- Complete heart block
Diagnosis
This patient was diagnosed with a second-degree atrioventricular block, 2:1 conduction. The initial ECG shows a ventricular rate of 36 BPM, with an atrial rate of 72 BPM. There are more P waves than QRS complexes, indicating the presence of an atrioventricular block. In this case, there are always two P waves for each QRS complex (Figure 1 and Figure 2).
Careful analysis of the rhythm reveals that P waves are conducted in a 2:1 ratio, with every other P wave “dropped,” or failing to conduct through the atrioventricular (AV) node. When P waves are conducted but intermittently dropped, it is referred to as second-degree AV block, which comes in two varieties: Mobitz I (or Wenckebach) and Mobitz II.
Mobitz I occurs when conduction is progressively delayed through the AV node and eventually fails. It is represented by progressively prolonging PR intervals followed by a dropped P wave. It does not always represent pathology, particularly when seen in younger or physically fit individuals with high vagal tone.
Mobitz II occurs when the infranodal conduction system intermittently fails, resulting in intermittently dropped P waves but consistent PR intervals when conducted. Mobitz II usually occurs with preexisting conduction disease (eg, combination of bundle branch and fascicular blocks), is always pathologic, and is more likely to progress to complete heart block.
When AV block occurs in a 2:1 ratio (Figure 2), it is impossible to distinguish between Mobitz I and Mobitz II; therefore, 2:1 AV block is simply referred to as “2:1 AV block.” When the QRS is narrow, as in this case, Mobitz I is more likely; however, it is prudent to assume the worst scenario (ie, Mobitz II) and transfer for an electrophysiology study and/or pacemaker placement unless more information suggests otherwise.1-3
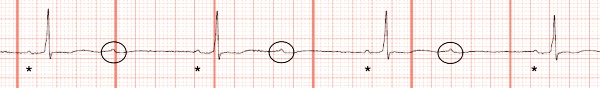
In this case, another ECG was performed after a short period of time, which revealed Mobitz I conduction (Figure 3 and Figure 4).
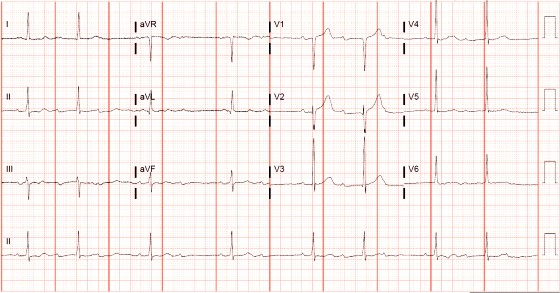
In Figure 3, there are periods of 3:2 block, where the PR interval prolongs before the QRS is dropped. This confirms the diagnosis of second-degree atrioventricular block, Mobitz type I (Wenckebach). This is illustrated again in Figure 4.

Although Mobitz I is often benign, this patient is 79 years old with known coronary artery disease and is symptomatic with nausea and vomiting. Therefore, he was transferred for pacemaker placement.
Learnings/What to Look for
- The presence of more P waves than QRS complexes should prompt consideration of an atrioventricular block
- In general, a first-degree AV block and second-degree Mobitz I block are unlikely to progress to complete heart block, especially in young and healthy patients
- It is impossible to distinguish between Mobitz I and Mobitz II with a fixed 2:1 ratio. Serial ECGs may help make the diagnosis
- With a fixed 2:1 AV block, it is safest to assume Mobitz II due to its high risk of progression to third-degree AV block
Pearls for Initial Management and Considerations for Transfer
- Consider patient demographics when analyzing AV nodal blocks; in a young patient, first-degree AV block is likely a benign finding. It may, however, represent serious pathology in an older patient with known heart disease and/or with preexisting conduction disturbances
- Patients with 2:1 AV block should be transferred to a facility capable of pacemaker placement
References
- Da Costa D, Brady WJ, Edhouse J. Bradycardias and atrioventricular conduction block. Br Med J. 2002;324(7336):535-538.
- de Pádua F, Pereirinha A, Marques N, et al. Conduction defects. In: Macfarlane PW, van Oosterom A, Pahlm O, et al, eds. Comprehensive Electrocardiology. London: Springer London; 2010:547-604.
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients with Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2019;140(8):e382-e482.

Read More
- A 46-Year-Old Man With ‘Burning’ Epigastric Pain Of Several Hours Duration
- A 60-Year-Old Woman With Hypertension, Diabetes, And Sudden Fatigue And Weakness
