Published on
Urgent message: Psoas (or iliopsoas) abscess, although rare, is a cause of back pain associated with high morbidity and mortality. Proper diagnosis requires the physician to recognize signs in the history and physical examination that are suggestive of a potentially serious spinal condition prompting further workup.
Fabrizia Faustinella, MD, PhD and L. Alexandre Frigini, MD
Citation: Faustinella F, Frigini LA. A common compliant with an unlikely diagnosis: psoas abscess in the urgent care center. J Urgent Care Med. 2023;17(4):17-21.
INTRODUCTION
Back pain is a common complaint in ambulatory centers, urgent care, and in emergency department; up to 84% of adults have back pain at some time in their lives.1,2
Back pain has a wide differential diagnosis, but is rarely due to grave medical conditions. Among patients who present with back pain to primary care settings, less than 1% will be diagnosed with a serious etiology such as cauda equina syndrome, metastatic cancer, and spinal infection (spinal epidural abscess, paraspinal abscess, septic discitis, vertebral osteomyelitis).3
Psoas abscess, a collection of pus in the iliopsoas muscle compartment, is one of the rare causes of back pain. A delayed diagnosis and inadequate treatment is associated with high risk for mortality due to septicemia.4-6
CASE PRESENTATION
A 62-year-old woman presented to our clinic with a complaint of 1 month of mid to low back pain, mainly on the right side of the spine. About 1 week after the pain had already started, she accidentally tripped and fell while doing housework. The patient denied direct injury to the back but reported worsening of pain after the fall.
At the time of the office visit, the pain which had rated 2 to 4 out of 10 at the onset of symptoms had progressively become 8 to 10 out of 10. The pain was constant and made it difficult for the patient to walk and rest at night.
There was radiation of pain to the right flank. She reported pain with right hip/leg movements, with no numbness/tingling in the lower extremities.
The patient denied saddle anesthesia, bowel/bladder incontinence/retention.
She also denied dysuria and urinary frequency. She reported fever and chills for the past few days prior to the office visit, and new-onset malaise and weakness.
Patient’s medical history was significant for major depression, anxiety disorder, degenerative joint disease, and hypertension.
Patient denied tobacco and alcohol use. No illicit drug use.
Patient’s medications at the time of the visit included Paxil, buspirone, ibuprofen, and propranolol.
Physical exam revealed a well-developed woman, alert, and cooperative, with:
- BP 109/56, HR 65, temp 97.7°F (36.5 °C), RR 19, SpO2 98%
- Head: Normocephalic
- Eyes: Conjunctivae/corneas/sclerae clear. Extraocular movements intact
- Neck: Neck supple, no adenopathy
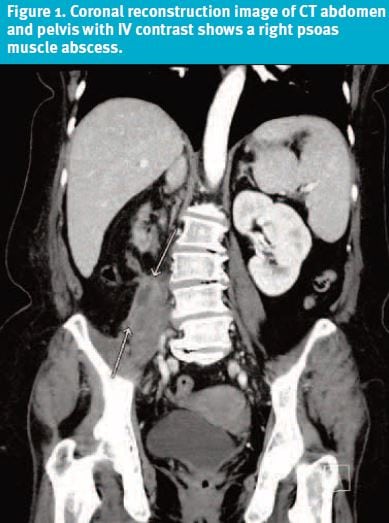
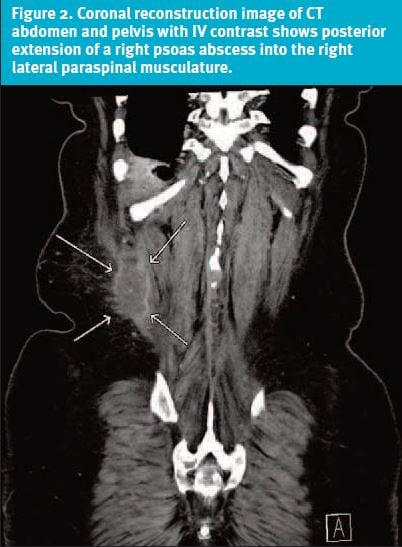
- Back: On inspection, there was a large mass at the mid-low back on the R side (Figure 1 and Figure 2). +TTP. Moderate to severe limitation of motion..
- Cardiovascular: RRR, no tubs/gallop/murmurs. No ectopy
- Pulmonary: Normal breath sounds with no wheezing, rales, or rhonchi
- Abdomen: Abdomen soft, nontender
- Ext: No clubbing, cyanosis, or edema
- Neurologic: Mental status intact, antalgic gait
The presence of the back mass, associated with progressively worsening pain and recent onset of fever, chills, malaise and weakness, raised the suspicion for a serious, nonmechanical cause of back pain.
The patient was transferred to the ED for further evaluation. Labs and imaging studies were ordered.
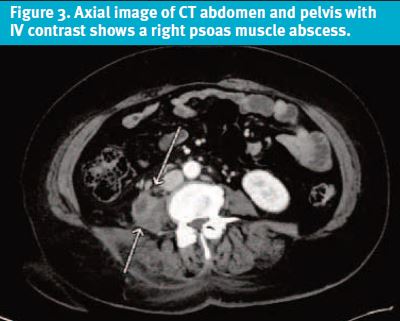
A CT abdomen/pelvis with contrast was ordered and showed the following results (Figure 3):
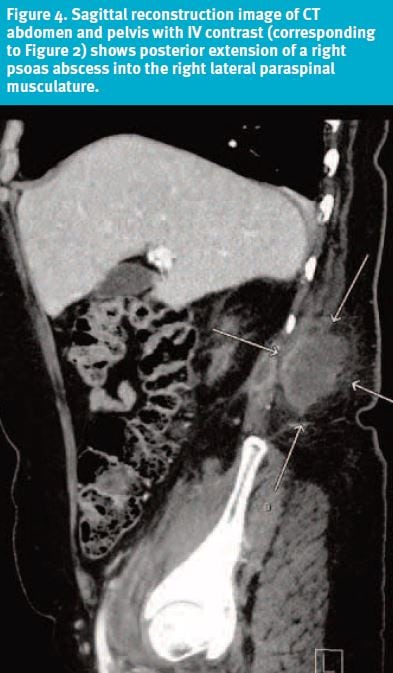
- Large/elongated right retroperitoneal abscess, centered within psoas muscle, extending posteriorly to the paraspinal soft tissues and inferiorly down to the pelvis and proximal right thigh.
- Atrophic right kidney with surrounding mild edema and a small collection, extending from the inferior pole, likely connecting to the above-mentioned abscess. Right pyelonephritis cannot be excluded.
DIFFERENTIAL DIAGNOSIS
In this particular case, what helped most in the decision-making process was the physical exam. Inspection, which refers specifically to what we can observe visually on the surface of the body, is a central aspect of the physical exam as it may lead to more accurate differential diagnoses and treatment.
The size of the mass found on physical exam pointed toward the presence of pathology of deeper organs and tissues. Wilms tumors of the kidney and perinephric abscesses may present as a mass in the back. Metastatic neoplasm and multiple myeloma of the spine may protrude from beneath the skin. Other neoplasms include large hemangiomas, neurofibromas, and lipomas.
In our patient, the more recent symptom of fever was suggestive of an infectious process. Pott disease of the spine and iliopsoas abscess were considered.
Pott disease, also known as tuberculous spondylitis, although possible, seemed less likely, as the patient denied any known exposure to tuberculosis in her life. In addition to that, the back pain was not chronic but more subacute in nature with a duration of about 4 weeks. Upon further questioning, our patient also denied recent skin infections, urinary tract infections, gastrointestinal symptoms, or any ailments requiring hospitalization or medical attention prior to the development of the back pain.
Vertebral osteomyelitis and abdominal/urologic disorders seemed also to be alternative diagnoses. The history of fall, although the back pain was present prior to that, made hematoma a possibility. Muscle spasm from back injuries can be significant enough to cause a mass, although the patient’s mass was too large to be attributed to lumbar strain and muscle spasm alone.
All of the above clearly pointed towards the immediate need for further workup with imaging studies such as computerized tomography. (Figure 4.)
COURSE AND TREATMENT
The patient was admitted to the Surgery Acute Care Unit. She underwent CT-guided aspiration and drainage catheter placement into the right psoas abscess. A 5-cc aspirate was obtained through the drain. The fluid was sent to microbiology for further evaluation. Culture and gram stain showed no organisms and no growth. Additionally, no anaerobes were isolated. This is not uncommon, as a definitive microbiological diagnosis for psoas abscess by infected fluid and blood culture has been reported to be 74.3% and 31.5%, respectively. 7
The patient was treated with IV vancomycin for 6 days and was discharged on oral Augmentin 875-125 mg BID for 14 days.
DISCUSSION
The psoas muscle is a muscle of the back. It originates from the lateral borders of the 12th thoracic to the 5th lumbar vertebrae in the retroperitoneal space and inserts at the lesser trochanter of the femur.
The fibers of the psoas muscle combine with those of the iliacus to form the iliopsoas, which functions as the chief flexor of the hip.
A psoas (or iliopsoas) abscess is a collection of pus in the iliopsoas muscle compartment and can be primary or secondary.
Primary psoas abscess is of unknown origin and caused by hematogenous or lymphatic spread from another distant origin. In the United States, up to 61% of psoas abscesses are primary. Primary psoas abscess occurs most commonly in patients with a history of diabetes, injection drug use, alcoholism, AIDS, renal failure, hematologic malignancy, immunosuppression, or malnutrition. 4,6 Our patient had a primary psoas abscess and no history of pertinent comorbid conditions.
Secondary psoas abscess is caused by direct spread of infection from adjacent structures like vertebrae, colon, urinary tract, and vascular system.7,8
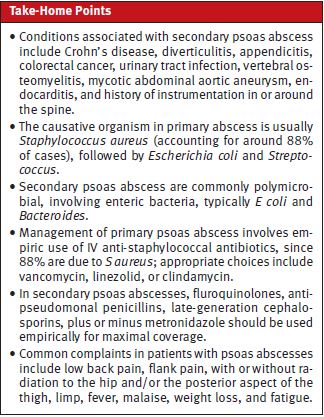
The causative organism in primary abscess is usually Staphylococcus aureus, which accounts for around 88% of the cases, followed by Escherichia coli and Streptococcus. Secondary psoas abscess are commonly polymicrobial, involving enteric bacteria, typically E coli and Bacteroides.9,10
Although the clinical presentation of a psoas abscess often lacks specificity, the presence of a large back mass in this particular case pointed to the presence of a serious disease process most likely arising from the deeper organs and/or tissues. This finding, associated with recent onset of fever and worsening back pain, prompted the initiation of further workup.
In our particular patient, the fluid cultures and blood cultures did not yield any microorganism.
Mycobacterium tuberculosis infection of the spine, known as Pott’s disease, is the most frequent cause of secondary psoas abscess in developing countries. Conditions associated with secondary psoas abscess include Crohn’s disease, diverticulitis, appendicitis, colorectal cancer, urinary tract infection, vertebral osteomyelitis, mycotic abdominal aortic aneurysm, endocarditis, and history of instrumentation in or around the spine.4,5,11 Bilateral psoas abscess occurs in 3% of all cases, primary or secondary.12,13
The most common complaints are low back pain, flank pain, with or without radiation to the hip and/or the posterior aspect of the thigh, limp, fever, malaise, weight loss, fatigue, inguinal mass. It is noteworthy that the presence of a back mass is not a typical finding in patients with psoas abscess. Limitation of hip movement is common due to pain triggered by stretching or extending the psoas muscle.
Our patient reported back pain, right flank pain, fever, malaise, and difficulty walking, although she never reported the presence of the back mass.
Laboratory tests are nonspecific and usually associated with high white blood cell count and elevated inflammatory markers.14
CT with contrast is the gold standard for the evaluation of patients for psoas abscess. The use of CT has increased the frequency of this diagnosis. Prior to computed tomography, most cases were diagnosed at postmortem.4
All patients with psoas abscess require hospitalization for IV antibiotics and surgical or percutaneous drainage of the abscess.
The management of psoas abscess involves the empiric use of IV anti-staphylococcal antibiotics since nearly 90% are due to S aureus with vancomycin, linezolid or clindamycin being appropriate choices. In secondary psoas abscesses, which frequently have a mixed flora of enteric pathogens, antibiotics need to have coverage for both gram-negative and anaerobic bacteria. Fluroquinolones, anti-pseudomonal penicillins, late-generation cephalosporins, plus or minus metronidazole should be used empirically for maximal coverage.14,15 The antibiotic regimen can later tailored to reflect the results of the culture and sensitivity profile and is usually continued for 2 weeks after abscess drainage.
CT-guided percutaneous drainage (PCD) or surgical drainage are the two definitive treatment modalities. PCD is less invasive and is currently the treatment of choice, especially in primary psoas abscess. Surgical drainage is indicated when PCD fails, or if there is a contraindication to PCD, or if there is abdominal pathology that requires such intervention.16-18
Complications associated with psoas abscess are sepsis, involvement of adjacent structures leading to septic arthritis, compression of surrounding structures leading to hydronephrosis, ileus, and deep venous thrombosis.
Mortality rates are higher for secondary psoas abscess. 5,10
Death, most often from sepsis, is usually due to delayed or inadequate treatment, with mortality close to 100% in patients who did not undergo drainage.5,6,10,19
Since Staphylococcus aureus accounts for 88% of the microorganisms isolated from primary psoas abscesses and since our patient responded well to IV vancomycin and oral amoxicillin, we can speculate that the most likely causative bacteria was, in fact, Staphylococcus aureus. The reason our patient developed an iliopsoas abscess remains unclear. The source of the primary hematogenous of lymphatic spread was never identified, neither on history nor on physical exam.
CONCLUSIONS
- This case is a reminder of the critical importance of inspection and thorough physical in the evaluation of patients with back pain.
- The diagnosis of a psoas abscess should be suspected on clinical grounds and confirmed on imaging studies.
- Iliopsoas abscess should be considered in the differential diagnosis when evaluating a patient with back pain associated with the presence of a back mass, pain on ambulation, and fever.
REFERENCES
- Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028-2037.
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006;31(23):2724-2727.
- Refshauge KM, Maher CG. Low back pain investigation and prognosis: a review. Br J Sports Med. 2006;40(6):494-498
- Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J. 2004;80(946):459-462.
- Sato T, Kudo D, Kushimoto S. Epidemiological features and outcomes of patients with psoas abscess: A retrospective cohort study. Ann Med Surg (Lond). 2021;62:114-118.
- Thongngarm T, McMurray RW. Primary psoas abscess [letter]. Ann Rheum Dis. 2001;60:173–176.
- Lopez VN, Ramos JJ, Meseguer V, et al. Microbiology and outcome of iliopsoas abscesses in 124 patients. Medicine (Baltimore). 2009;88(2):120-130.
- Tabrizia P, Nguyen SQ, Greenstain A, et al. Management and treatment of iliopsoas abscesses. Arch Surg. 2009;144(10):946-949.
- Vandenberge M, Marie S, Kuipers T, et al. Psoas abscess: report of a series and review of the literature. Neth J Med. 2005;63:413–416.
- Lai YC, Lin PC, Wang WS, et al. An update on psoas muscle abscess: an 8-year experience and review of literature. Int J Gastroenterol. 2011;5(2):75-79.
- Riyad MN, Sallam MA, Nur A. Pyogenic psoas abscess: discussion of its epidemiology, etiology, bacteriology, diagnosis, treatment and prognosis-case report. Kuwait Med J. 2003;35:44–47.
- Lee YT, Lee CM, Su SC, et al. Psoas abscess: a 10 year review. J Microbiol Immunol Infect. 1999;32:40–46.
- Bresee JS, Edwards MS. Psoas abscess in children. Pediatr Infect Dis J. 1990;9:201-206.
- Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: case report and review of the literature. J Urol. 1992;147:1624-1626.
- Chern CH, Hu SC, Kao WF, et al. Psoas abscess: making an early diagnosis in the ED. Am J Emerg Med. 1997;15:83–88.
- Dinc H, Onder C, Turhan AL, et al. Percutaneous drainage of tuberculosis and nontuberculosis psoas abscess. Eur J Radiol. 1996;23:130–134.
- Dave BR, Kurupati RB, Shah D, et al. Outcome of percutaneous continuous drainage of psoas abscess: a clinically guided technique. Indian J Orthop. 2014;48(1):67-73.
- Hsieh M-S, Huang S-C, Loh E-W, et al. Features and treatment modality of iliopsoas abscess and its outcome: a 6-year hospital-based study. BMC Infect Dis. 2013;13:578.
- Taiwo B. Psoas abscess: a primer for the internist. South Med J. 2001;94:2–5.
Manuscript submitted August 2, 2022; accepted August 12, 2022.
Author affiliations: Fabrizia Faustinella, MD, PhD, Department of Family and Community Medicine, Baylor College of Medicine. L. Alexandre Frigini, MD, Department of Diagnostic and Interventional Radiology, Baylor College of Medicine. The authors have no relevant financial relationships with any commercial interests.
Read More
- Management Of Acute Exacerbation Of Chronic Low Back Pain In The Urgent Care Setting
- Lumbar Hernia: An Unusual Cause Of Back Pain

