Urgent message: Knowing the mechanism of injury and presence of wound contamination is important in hand lacerations in order to avoid and anticipate skin and soft tissue infections and tissue necrosis, particularly in the setting of contaminated water sources.
Cayla Baker, PA-C and Christina Gardner, DHSc, MBA, PA-C
Introduction
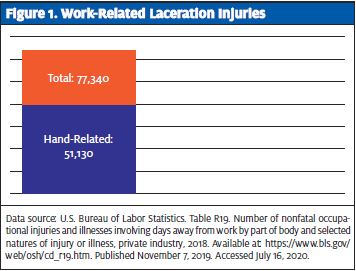
In 2018, the U.S. Bureau of Labor Statistics reported 77,340 work-related accidents resulting in lacerations, with 51,130 of those being to the hand.1 It is important to know the mechanism of injury as lacerations sustained in contaminated water sources are at higher risk for infection from gram-negative bacteria; antibiotics commonly prescribed for skin and soft tissue infections (SSTIs) may not be effective against gram-negative bacteria.
Case Presentation
A 47-year-old male with no significant past medical history presented to urgent care with a laceration sustained to the dorsum of his right hand after “falling into a sewer tank” at work which contained human wastewater. He did not sustain any other injuries. He was unsure of his tetanus immunization status.
Physical Exam
Focused examination revealed a 4 cm “T-shaped” laceration to the dorsum of the right hand. The laceration was approximately 2 mm deep and did not extend past the dermis. Hemostasis was achieved with direct pressure. Motor function and sensation remained intact. 2+ radial pulses were palpated bilaterally. There was no bone, ligament, or tendon involvement. No foreign bodies were visualized in the wound. Vitals were all within normal limits.
Initial Course and Treatment
The laceration was washed with Hibiclens and irrigated copiously with normal saline. It was then approximated with seven 4-0 Prolene sutures by simple interrupted technique. Tetanus immunization was updated and the patient was sent home on oral amoxicillin-clavulanate 875-125 mg twice daily for 10 days. He was educated regarding signs of infection, and given instructions to return immediately if any of these occurred.
The patient returned 3 days later with erythema and warmth with soft tissue swelling, tenderness, and clear drainage. There were no systemic signs of infection at that time. Motor function, sensation, and radial pulses were intact and equal bilaterally. A wound gram stain and culture were obtained. The patient was changed from amoxicillin-clavulanate to levofloxacin 750 mg orally once daily and clindamycin 300 mg orally four times daily for 10 days pending wound culture results and referred to an orthopedic hand specialist.
A wound culture grew 1+ Aeromonas hydrophila, 1+ Enterobacter asburiae and 1+ Aeromonas hydrophila STRAIN 2.
Five days later, before the outpatient hand specialist appointment could be made, the patient presented again, for concern of continued drainage and paleness around the infected site. He was seen by orthopedic surgery, who felt the wound was healing appropriately and that surgical debridement was not necessary. They removed the sutures and advised him to continue the antibiotic treatment prescribed at the urgent care. A follow-up appointment with an orthopedic hand specialist was made for the following week.
Discussion
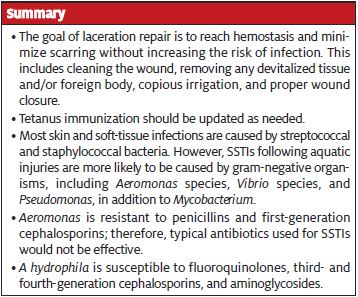
The goal of laceration repair is to reach hemostasis and minimize scarring without increasing the risk of infection.2 This includes cleaning the wound, removing any devitalized tissue and/or foreign body, copious irrigation, and proper wound closure. Tetanus immunization should also be updated as needed. Laceration repair of the hand with primary closure can be done if no underlying structural damage is suspected.2
Mechanism of injury and level of contamination play an important role in choosing the next steps. This patient was exposed to both an aquatic environment and human waste during his injury. The role of prophylactic antibiotics in the treatment of hand lacerations, or any laceration, is debated and their role for prevention of infection is unclear.
Most skin and soft-tissue infections are caused by streptococcal and staphylococcal bacteria.3 However, there are other organisms that more commonly cause SSTIs following aquatic injuries. These organisms are typically gram-negative and include Aeromonas species, Vibrio species, and Pseudomonas, in addition to Mycobacterium.4 Aeromonas hydrophila, as seen in this patient, is a commonly isolated organism in wound infections on an extremity following a traumatic aquatic injury.4 A hydrophila is an anaerobic, gram-negative bacillus found worldwide in freshwater environments. Infection typically occurs within 24 hours and can mimic a streptococcal or staphylococcal cellulitis, which often leads to incorrect treatment initially5.
When untreated, these infections can go on to cause necrotizing fasciitis and osteomyelitis—again, illustrating the importance of knowing if the injury is water-related. Aeromonas is resistant to penicillins and first-generation cephalosporins; therefore, typical antibiotics used for SSTIs would not be effective. A hydrophila is susceptible to fluoroquinolones, third- and fourth-generation cephalosporins, and aminoglycosides. In patients with localized symptoms of erythema, edema, and purulent drainage, outpatient management with oral antibiotics is appropriate as long as there is no involvement beyond the skin and subcutaneous tissues.3,5
Patients who present with systemic symptoms require inpatient management with intravenous antibiotics and possible surgical debridement in the operating room.4-6 For patients who present without signs of infection but who sustained a traumatic injury in an aquatic environment, there is some debate about whether to initiate antibiotics. Noonburg5 reports that because water-related injuries create an entry for aquatic microbes, the injured site should be treated as already infected and antibiotic therapy should be initiated with proper antibiotics that target gram-negative microbes.
In addition, while most uncomplicated wounds do not require systemic antibiotics, they are generally recommended for patients with increased risk of infections such as those in immunocompromised hosts, bite wounds, puncture wounds, grossly contaminated wounds, wounds involving tendons or cartilage, crush injuries, and wounds with delayed presentation (>18 hours).7-9 In this case, the contamination with feces would constitute this wound as high risk.
Vibrio species is another common gram-negative organism found in saltwater environments, and can cause necrotizing skin infections. Vibrio can be treated with a third-generation cephalosporin or a fluoroquinolone plus doxycycline.4
Enterobacter species are not common causes of soft tissue infections.10 Similar to A hydrophila, they are anaerobic gram-negative bacilli and are typically resistant to penicillins and first-generation cephalosporins. Enterobacter asburiae, as seen in our patient, is a normal gastrointestinal tract organism, which could account for its presence in this patient due to his contact with human fecal matter. These organisms are treated similarly to A hydrophila, so it did not have a huge impact on the treatment of this patient.
Case Conclusion
The patient was reseen by the hand specialist in follow-up and was healing well with only residual stiffness of the right index finger, which subsequently resolved.
In summary, injuries sustained in and around water sources are at risk of infection by organisms that are resistant to penicillins and first-generation cephalosporins. On initial presentation, copious irrigation of the wound and removal of devitalized tissue should be done to decrease risk of infection. Prophylactic antibiotics should be considered on a case-by-case basis, but would likely be considered in a wound that is highly contaminated from a water source. If a patient presents with an infection of a wound sustained in an aquatic environment, it is important to cover for gram-negative bacteria such as A hydrophila. If sustained in seawater, Vibrio should also be covered. Hand infections, specifically, should be followed closely, and providers should have a low suspicion for referral to orthopedic surgery to avoid permanent disability, particularly with joint, muscle, or tendon involvement, deep infections, or infections that are not improving despite antibiotic treatment.
References
- U.S. Bureau of Labor Statistics. Table R19. Number of nonfatal occupational injuries and illnesses involving days away from work by part of body and selected natures of injury or illness, private industry, 2018. Available at: https://www.bls.gov/web/osh/cd_r19.htm. Published November 7, 2019. Accessed July 16, 2020.
- Forsch RT, Little SH, Williams C. Laceration repair: a practical approach. Am Fam Physician. Available at: https://www.ncbi.nlm.nih.gov/pubmed/28671402. Accessed June 10, 2020.
- Reruch CM, Ewing JT, Oppenlander KE, Cowan WC. Acute hand infections. Am Fam Physician. 2019;99(4):228-236.
- Diaz JH, Lopez FA. Skin soft tissue and systemic bacterial infections following aquatic injuries and exposures. Am J Med Sci. 2015;349(3):269-275.
- Noonburg GE. Management of extremity trauma and related infections occurring in the aquatic environment. J Am Acad Orthop Surg. 2005;13(4):243-253.
- Weber CA, Wertheimer SJ, Ognjan A. Aeromonas hydrophila—its implications in freshwater injuries. J Foot Ankle Surg. 1995;34(5):442-446.
- Abubaker AO. Use of prophylactic antibiotics in preventing infection of traumatic injuries. Dent Clin North Am. 2009;53(4):707-715.
- Moran GJ, Talan DA, Abrahamian FM. Antimicrobial prophylaxis for wounds and procedures in the emergency department. Infect Dis Clin North Am. 2008;22(1):117-143.
- Nakamura Y, Daya M. Use of appropriate antimicrobials in wound management. Emerg Med Clin North Am. 2007;25(1):159-176.
- Koth K, Boniface J, Chance EA, Hanes MC. Enterobacter asburiae and Aeromonas hydrophila: soft tissue infection requiring debridement. Orthopedics. 2012;35(6):e996-9.
Author affiliations: Cayla Baker, PA-C, Carilion Clinic. Christina Gardner, DHSc, MBA, PA-C, Carilion Clinic Advanced ACP Fellowship in Urgent Care and Rural Health; Jefferson College of Health Services. The authors have no relevant financial relationships with any commercial interests.

