Published on
Urgent Message: Abdominal pseudohernia is a rare diagnosis with variable presentation. Urgent care clinicians who are familiar with the condition and its variable presentations can reduce the risk of diagnostic errors and unnecessary or inappropriate diagnostic testing.
Berkeley E Prewett, BSA; Stephen V Green, MD; Andrew L Juergens II, MD; Taylor K Ratcliff, MD
Citation: Prewett BE, Green SV, Juergens AL, Ratcliff TK. Abdominal Pseudohernia and Urinary Retention Due to Spinal Nerve Root Compression From Disc Herniation: A Case Report. J Urgent Care Med. 2024; 19(3)37-40
Key Words: abdominal pseudohernia, spinal nerve root compression, abdominal mass
Abstract
Introduction: Most patients presenting to urgent care (UC) with back pain, flank pain, and/or urinary symptoms do not have a serious diagnosis. However, in patients with worrisome associated symptomatology (eg, neurological deficits) a broader differential must be considered. Abdominal pseudohernia is a condition in which there is an outward bulging of a portion of the abdominal wall that resembles a hernia but without an actual anatomical fascial defect. Such pseudohernia, while rare in UC, may suggest serious underlying pathology.
Clinical Presentation: A 47-year-old man presented to UC with right flank pain and bulging of the abdomen for 2 days.
Physical Exam: The patient had normal vital signs. He had a soft, non-tender bulge of his right lower quadrant. He had no underlying mass or tenderness along the spine or costovertebral angle.
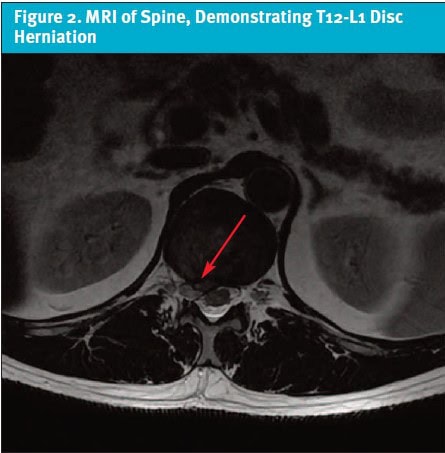
Diagnosis: He was referred to the emergency department (ED) where blood work, urinalysis, and a computed tomography (CT) scan of the abdomen and pelvis was interpreted as without significant abnormality. A right T12-L1 disc herniation was later noted on closer review of the CT and subsequent magnetic resonance imaging (MRI). The disc herniation was concerning for spinal nerve root compression causing the abdominal pseudohernia presentation.
Resolution: The patient’s symptoms spontaneously improved over time with resolution of the abdominal pseudohernia symptoms.
Conclusion: This case highlights the importance of considering both common and uncommon spinal pathology in patients with back pain, neurologic symptoms, and other less common findings, such as a new abdominal bulge. In particular, abdominal pseudohernia is a rare condition that can present with new onset abdominal bulging related to abdominal wall paresis.
Introduction
Acute low back pain is among the most common reasons for patients to seek acute unscheduled care in UC and ED settings, with a pooled estimated prevalence of 4.39%.1 The overwhelming majority of patients with acute atraumatic back pain will experience resolution without intervention, although it commonly will recur.2 Because the natural history of acute mechanical back pain is so often benign, both the American College of Radiology and the American Academy of Family Practice as part of the Choosing Wisely campaign recommend against spinal imaging in the first 6 weeks in the absence of red flag symptoms.3,4
UC clinicians typically will have familiarity with common red flag symptoms for concerning back pain presentations, including new or progressive neurologic symptoms such as bowel and bladder dysfunction. However, focal abdominal wall paresis, or abdominal pseudohernia (AP), is a less obvious nerve deficit.
AP is a rare clinical condition consisting of bulging of the abdominal wall that resembles a hernia, but without an underlying defect of musculature or fascia.5 It was first described by Loewe in 1936 after the injection of local anesthetic into the abdominal walls of guinea pigs caused bulging that resembled a hernia.6 Any pathology that causes neuromuscular disruption of the abdominal wall has the potential to cause AP. Reported etiologies include herpes zoster, diabetic neuropathy, rib fracture, and spinal surgery.5,7-14 Rarely, AP can occur due to direct spinal nerve root compression from spinal disc herniation, with only 10 reported cases in the existing literature.15 We present a case of AP secondary to herniation of the T12-L1 intervertebral disc.
Case Presentation
A 47-year-old male endurance athlete with no past medical history presented to UC with right flank pain since the prior afternoon. He reported that he developed unprovoked pain while attending a sporting event as a spectator. He was able to get some relief with ibuprofen, however, the right flank pain returned the following day and began radiating into the right lower abdomen. He also had complained of new urinary urgency. Additionally, he noticed a bulge to the right side of his abdomen, which ultimately prompted his decision to present for evaluation.
Physical Exam
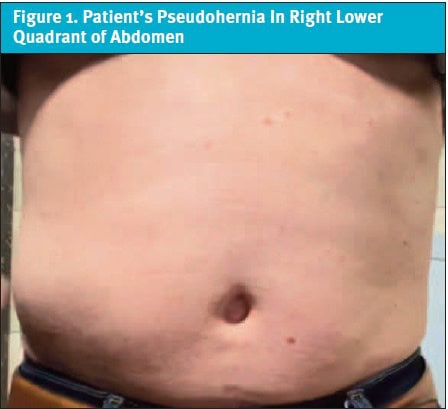
The patient was afebrile and had normal vital signs. A bulging of his right lower quadrant was noted on exam and was accentuated by Valsalva (Figure 1). The area and abdomen generally was soft and non-tender. No underlying mass was appreciated. While the patient endorsed right sided flank pain, he had no spinal or costovertebral angle tenderness. He was fully ambulatory and grossly neurologically intact.
Medical Decision Making
The UC clinician was concerned for a hernia or abdominal mass that might require surgical intervention. Additionally, with flank pain radiating to the right lower quadrant and the patient’s subjective urinary urgency there was concern for possible urinary tract pathology. The patient was, therefore, referred to the ED for further evaluation.
In the ED, he underwent computed tomography (CT) with intravenous contrast of the abdomen/pelvis and laboratory evaluation including a complete blood count, basic metabolic panel, liver function tests, and urinalysis. His CT was interpreted as normal and specifically there was no report of hernia, ureterolithiasis, hydronephrosis, or bladder distention. The laboratory tests also revealed no significant abnormality. Hence, he was discharged home with reassurance.
Differential Diagnosis
This patient presented with multiple complaints including flank pain and a bulge of the abdominal wall. Flank pain with urinary symptoms is suggestive of renal pathologies, including ureterolithiasis or upper urinary tract infections (ie, pyelonephritis). However, a new lateralized abdominal bulge or mass would be unexpected in the these cases.
True hernias and abdominal masses should be considered in patients presenting to UC with an abdominal bulge, particularly if they present with symptoms of ileus (eg, obstipation, vomiting), which might suggest a possible small bowel obstruction. Additionally, if suspected hernia is present, tenderness to the bulge—which might suggest incarceration or strangulation—also warrants immediate ED referral. Other causes of abdominal bulging should be considered, including intra-abdominal or abdominal wall tumors, cysts, abscesses, and hematomas. Other considerations include abdominal aortic aneurysm, diastasis recti, bladder distention from urinary retention, or organomegaly. Depending on the suspected etiology of the abdominal bulge, referral may be indicated for acute or routine workup.
Final Diagnosis and Case Conclusion
The patient’s symptoms persisted several days following his ED visit, so he self-referred to a general surgeon. At the follow-up visit, the surgeon reviewed his CT imaging and noticed a right T12-L1 disc herniation which was concerning for spinal nerve root compression causing the AP. Subsequently, an MRI without and with contrast of the thoracic and lumbar spine was ordered, which revealed spinal nerve root compression from a right T12-L1 disc herniation (Figure 2).
Disposition and Patient Perspective
The patient opted for expectant management of his condition. His presumed nerve impingement symptoms spontaneously improved over a matter of weeks with resolution of the AP symptoms. He has been asymptomatic with no abdominal pain or muscle wall weakness since.
Discussion
AP is a rare clinical condition causing bulging of the abdominal wall without an associated abdominal wall defect. The bulging is secondary to denervation of one or more lower thoracic nerve root resulting in abdominal wall paresis. Causes of AP include herpes zoster, complications of spine surgery, rib fracture, and diabetic neuropathy.5,7-14 Additionally, there are 10 cases of AP secondary to spinal disc herniation reported.15 AP are generally self-limited conditions, but autonomic dysfunction such as ileus and constipation have been reported in certain cases.10
Because most cases of AP resolve spontaneously, AP management generally focuses on symptom control. In cases of AP caused by disc herniation, initially deferring surgical therapy is reasonable, unless symptoms are causing significant gastrointestinal motility dysfunction.16 In the case presented, the patient’s symptoms followed the most common trajectory and resolved without any further intervention.
At the end of the first visit, this patient was initially reassured of the results of his workup. AP and its underlying etiologies should be considered if the patient endorses associated sensory deficits, dermatomal rash, and/or autonomic dysfunction. While an emergent condition may not be present, it is important to ensure patients are aware of red flag symptoms, which should prompt immediate reassessment and appropriate follow-up with primary care or an appropriate specialist.
Ethics Statement
The patient presented in this case provided verbal and written consent for the creation of this case report and discussion regarding his care. In the interest of patient privacy, certain patient details were omitted from this case.
Takeaways for Urgent Care Providers
- Consider spinal pathologies of back and flank pain when accompanied by common and uncommon neurological deficits, such as focal abdominal wall paresis, as well as other associated symptoms like urinary retention and urgency.
- Though AP is a rare clinical condition, it is important to include in the differential diagnosis when working up patients presenting with abdominal bulging.
- In patients who present with symptoms consistent with an abdominal hernia or pseudohernia, referral from the UC to the ED, while not absolutely indicated, is often reasonable in order to rule out other potentially emergent pathologies in the differential diagnosis.
- AP is most commonly self-limited. Complications of autonomic or gastrointestinal dysfunction may occur and, if caused by mechanical spinal nerve root compression, surgical intervention may be warranted.
Manuscript submitted May 29, 2024; accepted October 10, 2024
References
- Edwards J, Hayden J, Asbridge M, Gregoire B, Magee K. Prevalence of low back pain in emergency settings: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2017;18(1):143. doi:10.1186/s12891-017-1511-7
- Heuch I, Foss IS. Acute low back usually resolves quickly but persistent low back pain often persists. J Physiother. 2013;59(2):127. doi:10.1016/S1836-9553(13)70166-8
- American Association of Family Physicians website. Imaging for Low Back Pain. Accessed September 26, 2024. https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/cw-back-pain.html
- American College of Radiology website. ACR Appropriateness Criteria Low Back Pain. Accessed September 26, 2024. https://acsearch.acr.org/docs/69483/Narrative/
- Butensky AM, Gruss LP, Gleit ZL. Flank pseudohernia following posterior rib fracture: a case report. J Med Case Rep. 2016;10(1):273. doi:10.1186/s13256-016-1054-9
- Loewe S. Pseudohernia, a visible manifestation of local anesthetic action. J Pharmacol Exp Ther. 1936;56:238-251.
- Ohno S, Togawa Y, Chiku T, Sano W. Postherpetic pseudohernia: delayed onset of paresis of abdominal muscles due to herpes zoster causing an ipsilateral abdominal bulge. BMJ Case Rep. 2016;2016. doi:10.1136/bcr-2016-215377
- Mizumoto J. Abdominal pseudohernia due to herpes zoster. Cleve Clin J Med. 2021;88(9):480-481. doi:10.3949/ccjm.88a.20178
- Tsukita K, Sakamaki-Tsukita H. Abdominal wall pseudohernia and colonic pseudo-obstruction as complications of herpes zoster. Clin Gastroenterol Hepatol. 2019;17(4). doi:10.1016/j.cgh.2018.04.051
- Lee TH. Unusual case of abdominal wall pseudohernia in a patient with acute constipation. Korean J Intern Med. 2021;36(1):228-229. doi:10.3904/kjim.2020.106
- Chiu HK, Trence DL. Diabetic neuropathy, the great masquerader: truncal neuropathy manifesting as abdominal pseudohernia. Endocr Pract. 2006;12(3):281-283. doi:10.4158/EP.12.3.281
- Chakraborty PP, Singha A, Bhattacharjee R, Chowdhury S. Abdominal pseudohernia: a manifestation of diabetic truncal radiculoneuropathy. BMJ Case Rep. 2016;2016. doi:10.1136/bcr-2016-215605
- Nadirov N, Vissarionov S, Khusainov N, Filippova A, Sazonov V. Abdominal pseudohernia in a child after surgical correction of congenital scoliosis: case report. Front Pediatr. 2024;11:1211184. doi:10.3389/fped.2023.1211184
- Yasukawa T, Ohya J, Kawamura N, et al. Abdominal pseudohernia after extreme lateral interbody fusion procedure: a case report. Spine Surg Relat Res. 2020;5(3):218-220. doi:10.22603/ssrr.2020-0085
- Cho WJ, Kim KW, Kim BH, Ryu JH. Monoradiculopathy-induced abdominal pseudohernia caused by T11-12 soft disc herniation: a case report and literature review. BMC Musculoskelet Disord. 2023;24(1):428. doi:10.1186/s12891-023-06536-1
- Fitzpatrick J, Birch N, Botchu R. Abdominal wall pseudohernia – One secondary to a thoracic extraforaminal disc herniation and other due to thoracic paracentral disc protrusion. J Clin Orthop Trauma. 2022;30:101897. doi:10.1016/j.jcot.2022.101897
Author Affiliations: Berkeley E Prewett, BSA, Baylor College of Medicine. Stephen V Green, MD, Baylor Scott & White Health. Andrew L Juergens II, MD, Baylor Scott & White Health. Taylor K Ratcliff, MD, Baylor Scott & White Health. Authors have no relevant financial relationships with any ineligible companies.
Download the Article PDF: Abdominal Pseudohernia and Urinary Retention Due to Spinal Nerve Root Compression From Disc Herniation: A Case Report
