- Projecting Outcomes in mTBI
- Concussion Recovery in Athletes
- A New Tool in Assessing Adolescent Concussion
- Head Injury in Patients Taking Warfarin
- Infants with Scalp Haematoma
- To CT or Not to CT Low-Risk Peds Head Injury?
- Posttraumatic Headache in Children
- Out-of-Hospital Cardiac Arrest
Ivan Koay, MBChB, FRNZCUC, MD
Identifying mTBI Patients with Long-Term Poorer Outcomes
Key point: Patients with a history of psychiatric disorder, racial minorities, and those with lower level of education are most likely to have ongoing functional disabilities after minor traumatic brain injury (mTBI).
Citation: Madhok DY, Yue JK, Sun X, et al. Clinical Predictors of 3- and 6-month outcome for mild traumatic brain injury patients with a negative head CT scan in the emergency department: a TRACK-TBI pilot study. Brain Sci. 2020;10(5):269.
Relevance: Identifying the predictors of negative outcomes for patients with mTBI can be helpful in informing emergency and urgent care management strategies and improve patient outcomes, decrease ED utilization, and bouncebacks to UC.
Study summary: This was a subset analysis from the TRACK-TBI pilot study conducted at three U.S. Level 1 trauma centers via convenience sampling from 2010 to 2012. Patients were assessed for ongoing functional disabilities—cognition, independence, employability, and social/community participation post-TBI and had a negative CT head at the time of ED visit. Three- and 6-month Glasgow Outcome Scale-Extended assessment was used to evaluate the participants. The authors found poorer outcomes in patients with a history of psychiatric disorder (anxiety, depression, PTSD, bipolar, schizophrenia, sleep disorders). Additionally, patients with fewer years of education were also more likely to have ongoing functional disabilities. Racial minority status (namely, Asian, Native American/Alaskan, Hawaiian or Pacific Islander) was also associated with poorer outcomes compared with Caucasians. These disabilities were noted to continue at the 6-month review, as well.
Limitations: This was a convenience sample study and may not be representative of all patients with mTBI. Attrition bias was evident in this study, as follow-up was reliant on patients returning. Both were acknowledged by the authors.
Do Athletes with Concussion Take Longer to Recover than Previously Suggested?
Key point: Athletes with sports-related concussion often take longer than 2 weeks to recover. Therefore, a staged return to play approach may be beneficial with longer projected return-to-play programs potentially necessary.
Citation: Kara S, Crosswell H, Forch K, et al. Less than half of patients recover within 2 weeks of injury after a sports-related mild traumatic brain injury: a 2-year prospective study. Clin J Sport Med. 2020;30(2):96-101.
Relevance: The ability to identify patients with concussions who will have longer recovery will enable clinicians to better prepare patients and families for realistic return-to-play timelines and, therefore, also inform the return-to-play protocols for them.
Study summary: This was a prospective observational cohort study looking at patients referred to a community-based sports concussion clinic in Auckland, New Zealand. Patients were initially assessed with SCAT-5 screening tool. Neurological and vestibular assessments were also performed. Subsequent follow-up with SCAT-5 screening was done along with assessment of any previous abnormal physical findings. Patients were educated regarding cognitive and physical loading after a prescribed period of rest. From January 2017 to December 2018, 594 patients were recruited and analyzed (out of a total of 822 participants who presented to the clinic.) Most of the patients were rugby athletes (54%) and the age spread was from 7 to 64 years (average 20.2 years).
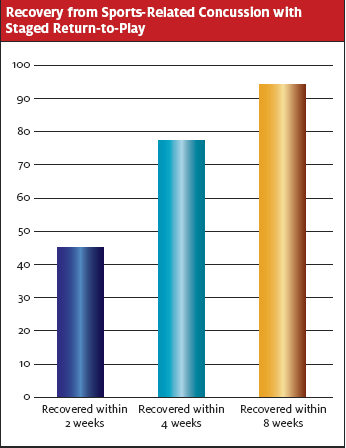
The investigators found that 45% of participants had clinical recovery within 2 weeks, 77% by 4 weeks, and 94% by 8 weeks. Female patients took longer on average to recover. There were similar timelines for recovery regardless of age. Vestibular, with or without cervical, rehabilitation was more likely required in adults. Results also suggested that patients seen earlier in the clinic tended to have a faster recovery.
Limitations: This was a single-center study with referrals from the community (therefore, with potential for selection bias). There was a high attrition rate due to incomplete data. The authors acknowledge the lack of pre-injury comparison neurocognitive scores and the discharge criteria used. It is unclear how well the patients did on returning to sports compared to their pre-injury state.
A New Biomarker for Concussion Assessment in Adolescents?
Key point: Pupillary light reflex metrics may be a suitable marker for identifying adolescents with concussion.
Citation: Master CL, Podolak O, Ciuffreda KJ, et. al. Utility of pupillary light reflex metrics as a physiologic biomarker for adolescent sport-related concussion. JAMA Ophthalmol. 2020;24; e203466.
Relevance: Finding new and innovative biomarkers to assess concussion can improve our understanding, assessment, and management of the condition.
Study summary: This was a prospective observational study of the pupillary light reflex (PLR) in adolescents with sports-related concussion and control individuals recruited from a private suburban high school within the Philadelphia area. Measurements were conducted with a hand-held pupilometer device. Metrics measured were pupillary diameter, percent constriction, latency (time to maximum constriction in response to the light stimulus), peak and average constriction velocity, average dilation velocity, and T75 (time for pupil re-dilation from minimum diameter to 75% maximum diameter).
The authors found there were significant differences between athletes with concussion and controls for all PLR metrics except latency. Athletes with concussion had larger maximum pupil diameter, minimum pupil diameter, greater percentage constriction, higher average constriction velocity, peak constriction velocity, average dilation velocity, peak dilation velocity, and T75.
Limitations: The authors acknowledge limitations of a study where participants were only adolescents and affirm results cannot yet be extrapolated to adults. Diurnal changes in PLR were not considered. There were also no baseline measurements recorded for the participants.
Do All Patients Taking Warfarin with Head Injuries Require CT Head Scans?
Key point: Clinical decision rules are there as a guide for clinicians, however decisions regarding investigations should be tailored to the individual being treated.
Citation: Mason SM, Evans R, Kuczawski M. Understanding the management of patients with head injury taking warfarin: who should we scan and when? Lessons from the AHEAD study. Emerg Med J. 2019;36(1):47–51.
Relevance: Understanding which patients with head injuries who are also anticoagulated would benefit from head CT will support better decision-making and resource utilization. Most present clinical decision rules have not incorporated patients on anticoagulation in their analyses.
Study summary: This study was a review of the AHEAD study, a prospective observational study that recruited patients taking warfarin with head injuries across 33 EDs in England and Scotland. In the study, 3,534 adults taking warfarin who suffered nonpenetrating head injuries were recruited between September 2011 and March 2013. The investigators discovered that Glasgow Coma Scale (GCS) <15 was the strongest predictor of adverse outcomes. Patients with head injury-related symptoms such as loss of consciousness, vomiting, and amnesia were associated with adverse outcomes even if the presenting with a GCS of 15. The presence of headache in patients with a GCS of 15 was weakly associated with adverse outcomes. Patients with a GCS of 15 and no neurological symptoms were less likely to have adverse findings. The authors therefore suggest in this group, shared decision making regarding their management and investigations may be considered.
Limitation: Complexity of the topic means that there may not be a “one size fits all” approach, acknowledged by the authors. Therefore, clinical judgement and acumen do play a role in the management and investigation of these patients.
[Editor’s note: Should this paper change our practice? Probably not. Patients on oral anticoagulation with nonpenetrative head injury should still be considered high risk. Therefore, it still makes sense to recommend head CT for all patients taking anticoagulation who suffer blunt head injury.]
Do Infants with Scalp Haematoma All Need CT?
Key point: The Scalp Score is a potentially new risk-stratifying tool for the decision-making process when considering imaging of infants with scalp hematomas.
Citation: Schutzman SA, Nigrovic LE, Mannix R. The Infant Scalp Score: a validated tool to stratify risk of traumatic brain injury in infants with isolated scalp haematoma. Acad Emerg Med. July 16, 2020. Epub ahead of print.
Relevance: New ways to stratify risk of TBI in infants will enable better management strategies in treating patients presenting to UC with these injuries and enhance decision-making processes for clinicians.
Study summary: A group of patients from the PECARN data set, children <1 year of age with infant scalp haematoma (ISH), was assessed. ISH was defined as scalp hematoma without other clinical findings on initial ED history. A scalp score was then constructed based on the original recordings to more precisely risk stratify head-injured children. The scoring as cited:
| Risk Points | Patient’s Age (months) | Haematoma Size (cm) | Haematoma Location |
| 0 | >12 | 0 | Frontal |
| 1 | 6-11 | <1 | Occipital |
| 2 | 3-5 | 1-3 | Temporal/Parietal |
| 3 | 0-2 | >3 |
The researchers noted that no child with a score <5 had a clinically important traumatic brain injury (ciTBI) and no child with a score <4 had a radiographically evident TBI on CT. Scores >5 indicated increase risk of complications.
Limitation: The study was retrospective in nature and therefore has some inherent limitations related to its design. However, it is reasonable to incorporate a Scalp Score into the PECARN pediatric head injury decision aid if a scalp hematoma is the only concerning finding.
Reducing CT Head Use for Low-Risk Pediatric Head Injury Patients
Key point: Implementation of a head injury assessment tool with buy-in from clinicians, decreases the utilisation of head CT in low risk pediatric patients.
Citation: Puffenbarger MS, Ahmad FA, Argent M, et. al. Reduction of computed tomography use for paediatric
closed head injury evaluation at a nonpaediatric community emergency department. Acad Emerg Med. 2019;26(7):784-795.
Relevance: Pediatric patients with low-risk head injuries can be safely discharged home without imaging with appropriate anticipatory guidance and follow-up instructions. Implementation of this rule can be achieved with appropriate training for ED and UC clinicians and staff.
Study summary: This was a quality improvement study designed to reduce head CT use in a nonpediatric ED by the implementation of a pediatric closed head injury decision aid based on the PECARN assessment tool. Retrospective chart review was done pre-, during, and postimplementation of the assessment tool from March 2014 to August 2017. The ED was part of 13 partner regional hospitals spanning two states in the U.S. With the implementation of the tool following education of clinicians (physicians, physician assistants, and nurse practitioners), there was a significant decrease in head CT use for blunt head injury in children during the study, which persisted postimplementation. The largest decrease in usage was in the low-risk patients evaluated by physicians. The number of patients with high- and moderate-risk head injuries who underwent head CT did not decrease. There was also improvement in ED length-of-stay times after implementation. There were no ciTBIs missed with patient follow-up.
Limitation: This was a relatively small study involving a nonpediatric ED which may not be generalizable to other areas. The authors acknowledged potential selection bias due using physician assigned discharge diagnoses rather than ICD-10 coding in the EMR.
Post-Traumatic Headache in Pediatric Population—Review of Present Evidence
Key point: Post-traumatic headache (PTHA) is common post-mTBI in the pediatric population. Increased understanding of this condition can help UC providers educate and help patients in their recovery
Citation: Blume HK. Posttraumatic headache in pediatrics: an update and review. Curr Opin Pediatr. 2018;30(6):755-763.
Relevance: Mild head injury is a common presentation for pediatric to patients in the ED and UC centers. The ability to perform accurate assessments and knowledge of the current best evidence will help clinicians guide patients with their recovery and are crucial in prevention of long-term morbidity.
Study summary: This was a review article collating present definitions and recent research regarding posttraumatic persistent headache syndrome and the current treatment strategies in children. ED-based studies have examined PTHA, specifically after pediatric mTBI, and described rates of PTHA were 69% at 1 week, 25% at 1 month, 5% to 7.8% at 3 months, and 1.2% at 1 year after injury. Prior history of migraine may be associated with prolonged recovery, but neither ADHD nor learning disabilities nor injury characteristics (amnesia and loss of consciousness) were consistently associated with increased risk for PTHA.
Education about expected symptoms and symptom course following mTBI in the ED improved outcomes compared with those who did not receive education. Use of ibuprofen or other NSAIDs following mTBI is recommended once acute structural brain injury has been excluded. The role of “rest” in the management of acute concussion and postconcussion syndrome is evolving. Several studies demonstrated that “strict rest” in the days following head injury may be detrimental to recovery. Because repeated concussions in a short period of time are known to be dangerous, optimal levels of activity lie somewhere between full rest and full return to activity. Multidisciplinary care, with medical provider, psychologist, and other personnel is likely helpful for children with persistent symptoms.
Which Strategy is Best in Community Cardiac Arrests?
Key point: Continued on-scene resuscitation may have better outcomes compared with intra-arrest transportation.
Citation: Grunau B, Kime N, Leroux B, et. al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. JAMA. 2020 Sep 15;324(11):1058-1067.
Relevance: There is an ongoing dilemma regarding care for out-of-hospital cardiac arrest (OHCA) situations as to whether advisable to continue resuscitation efforts on scene or to transport the patient immediately to a medical facility where more equipment and staff are available.
Study summary: This is a secondary analysis from the Resuscitation Outcome Consortium (ROC) Cardiac Epidemiologic Registry-Cardiac Arrest OHCA registry based on a prospective population-based registry of 10 North American study sites that included consecutive EMS assessed nontraumatic OHCA between April 2011 and June 2015.
The authors found that survival to hospital discharge and favorable neurologic outcomes were lower among patients treated with intra-arrest transport compared with continued on-scene resuscitation. Intra-arrest transport was associated with a significantly lower probability of survival to hospital discharge within the subgroups of ALS first, ALS second, EMS witnessed, not EMS witnessed, initial shockable cardiac rhythm, and initial non-shockable cardiac rhythm. There was no significant association seen in the BLS-only and mechanical CPR-treated subgroups. Further subset analysis was performed for patients with potentially favorable situations (shockable rhythm and EMS witnessed events). There were consistent adverse outcomes for intra-arrest transport in these patients as well despite the smaller numbers analysed.
Limitation: There was no randomization of subjects and therefore the results may be affected by selection bias. The study population was based in North America and therefore may not be able to be generalized to all countries. The skills of the EMS staff may also differ from those available in other geographical locations.

