- General Statistics of COVID-19
- Clinical Characteristics of COVID-19
- Characteristics of Healthcare Workers Infected with COVID-19
- A Simple Algorithm for Treatment of Nonpurulent Infections
- Topical Lidocaine for Oral Ulcers in Children
- Walking Boot vs Rigid Cast in Achilles Tendon Rupture
General Statistics of COVID-19
Key Point: The majority of patients with COVID-19 have mild symptoms; however, those with critical disease have a mortality rate of 49%.
Citation: Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. [Epub ahead of print February 4, 2020.]
Relevance: Mainstream media reports on mortality figures and the severity of COVID-19 are accurate in a “big picture” sense but are misleading and may be fueling panic among the public. Breaking down the data may be useful for clinicians in assessing risk and in educating patients.
Study Summary: Consideration of 72,314 cases shows that:
- Patients between 30and 79 years of age make up 87% of cases
- Patients age 20-29 and >80 years make up 8% and 3% of cases, respectively
- Mortality rate overall is 2.3%
- 81% of patients with COVID-19 experience mild disease
- 14% experience severe disease
- 5% experience critical disease with 49% mortality rate
Clinical Characterization of COVID-19
Key Point: COVID-19 is a novel disease with associated clinical, laboratory, and imaging characteristics.
Citation: Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
Relevance: The rate of infection with COVID-19 has outpaced data collection regarding the most relevant characteristics of infected patients. Early insights from Wuhan, China may inform patient assessment and diagnostic procedures.
Study Summary: The authors characterize clinical aspects of COVID-19 in 41 patients. Here are the most pertinent insights:
- The most common symptoms were fever, cough, and myalgia/fatigue
- Upper respiratory symptoms such as rhinorrhea, sneezing, and sore throat were not common
- Bilateral involvement on chest CT was seen on 98% of patients
- Lab findings include lymphopenia, elevated AST, D-dimer, troponin, and cytokines
- Median 7 days from symptom onset to hospital admission
- Median 10.5 days from symptom onset to mechanical ventilation
Clinical Characteristics of Medical Staff Infected with COVID-19
Key Point: The majority of medical staff infected with COVID-19 were not front-line workers, which include emergency providers.
Citation: Chu J, Yang N, Wei Y, et al. Clinical characteristics of 54 medical staff with COVID-19: a retrospective study in a single center in Wuhan, China. J Med Virol. [Epub ahead of print March 29, 2020.]
Relevance: Healthcare workers in general are at increased risk for infection with coronavirus. Identifying departments in which staff are at the greatest risk may provide rationale for allocating or adapting protective resources.
Study Summary: The authors characterize COVID-19 in 54 infected medical staff. Here are the most pertinent info:
- 4% of infected staff worked in first-line departments (emergency department, fever clinic, fever ward, respiratory and critical care department, and infection department)
- The majority (72%) of infected staff were from other clinical departments
- 19% of infected staff were from medical technology dept (examination and testing)
- 20% had “common type” symptoms
- 74% had “severe type” symptoms
- 6% had “critical type” symptoms
Improving Antibiotic Stewardship via Algorithm Implementation
Key Point: Implementation of an algorithm for treatment of nonpurulent skin and soft tissue infection led to decrease in hospital admission and treatment failure
Citation: Haran JP, Goulding M, Campion M, et al. Reduction of inappropriate antibiotic use and improved outcomes by implementation of an algorithm-based clinical guideline for nonpurulent skin and soft tissue infections. Ann Emerg Med. [Epub ahead of print February 13, 2020.]
Relevance: Antibiotic stewardship is a critical component of good clinical practice that can prevent over- or unnecessary exposure for patients, as well as growth of resistant organisms. This study looks at the effects of implementation of an algorithm that follows Infectious Disease Society of America guidelines in practice and outcomes. (See Figure 1 and Tables 1 and 2.)
Study Summary: In this year-long cohort study, 1,360 patients diagnosed with nonpurulent skin or soft tissue infection in two emergency departments were followed. Intervention included a pocket card summarizing a simple treatment algorithm that featured cephalexin as the recommended treatment option for uncomplicated infections. After implementation of a treatment algorithm, hospital admissions were reduced by 26% while risk of treatment failure was reduced by 46%. In addition, risk of readmission was reduced by 45%.
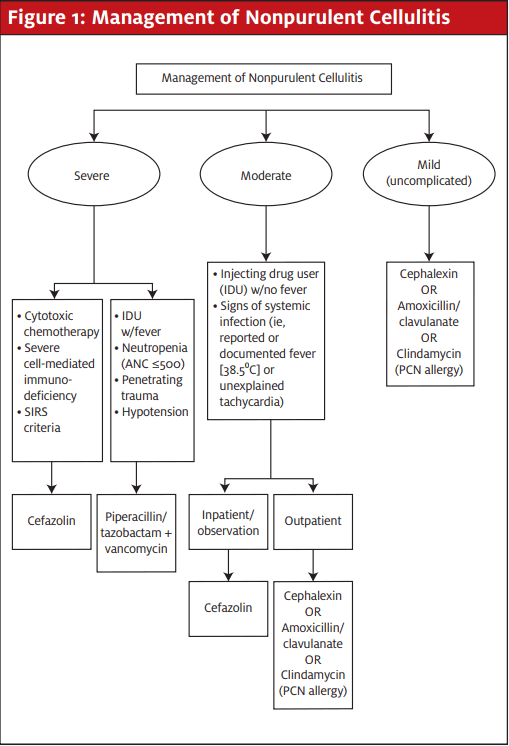
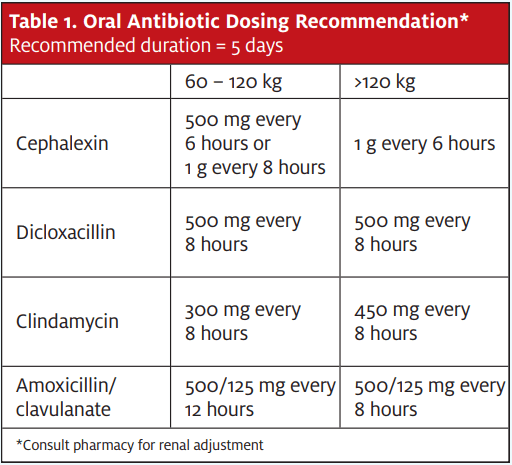
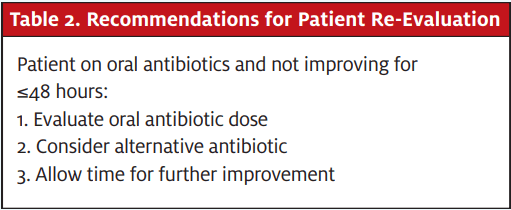
Algorithm and tables adapted from: Smith C. Resurrecting lowly cephalexin for non-purulent SSTI. JournalFeed. Available at: https://journalfeed.org/article-a-day/2020/resurrecting-lowly-cephalexin-for-non-purulent-ssti. Accessed April 9, 2020.
Topical Lidocaine Improves Pain in Children with Oral Ulcers
Key Point: Topical lidocaine improved pain in children with oral ulcers; however, it did not show increase in oral intake.
Citation: Daniel RMD, Jason SDO, Jeffrey SJ. BET 2: Does topical lidocaine improve oral
intake in children with painful mouth ulcers? Emerg Med J. 2020;37(2):113-114.
Relevance: Clinicians often use topical lidocaine for symptom relief in children with oral ulcers. However, it is unclear whether this treatment modality offers meaningful relief, such as improving their intake of food.
Study Summary: This was a review of two randomized controlled trials; one trial showed that topical lidocaine led to improved pain scores and the other found that there was no difference in oral intake after topical lidocaine was applied. When using topical lidocaine for symptom relief, it is important to bear in mind that the maximum dose should not be over 4.5 mg/kg/dose to prevent systemic toxicity.
Walking Boot vs Rigid Cast in Achilles Tendon Rupture
Key Point: Treatment of Achilles tendon rupture with walking boot or rigid cast resulted in similar outcomes and adverse events.
Citation: Costa ML, Achten J, Marian IR, et al; UKSTAR trial collaborators. Plaster cast versus functional brace for non-surgical treatment of Achilles tendon rupture (UKSTAR): a multicentre randomised controlled trial and economic evaluation. Lancet. 2020;395(10222):441-448.
Relevance: Patients with Achilles tendon rupture are typically treated with a cast for weeks. While casts offer maximum protection, this practice can lead to muscle atrophy and ankle stiffness, as well as the added burden of being non-weightbearing for the patient.
Study Summary: In this multicenter, randomized, controlled trial, patients were randomly assigned to receive a plaster cast or functional brace for 8 weeks. The authors found that there was no difference between patient-reported Achilles tendon rupture scores at 9 months. In addition, there was no difference in rate of tendon re-rupture (6% vs 5%, p = 0.40). Finally, the total cost for the plaster cast vs functional brace group was $1,465 vs $1,337.

