Published on
Urgent message: Acute stridor in pediatric patients is alarming to children, parents, and healthcare providers alike. Differential diagnosis is the key to initial evaluation and management of this worrisome symptom. Here is how to think it through.
JERRI A. ROSE, MD, FAAP
Stridor is an externally audible sound caused by abnormal air passage during breathing.1 It results from turbulent airflow through large airways. When a normal respiratory volume of air passes through narrowed airways, the normal laminar flow becomes turbulent. Therefore, stridor serves as a signal of partial airway obstruction.
Stridor occurs relatively commonly in pediatric patients. Its presence can be alarming to children, parents, and healthcare providers alike. Children presenting with stridor require a thorough and careful evaluation to determine the underlying cause of this worrisome symptom, and to promptly detect and address any life-threatening etiologies.
This article discusses differential diagnoses for acute stridor in children and offers guidance for the initial evaluation and management of children presenting acutely with stridor.
Pathophysiology
Stridor may be caused by pathology anywhere within the large airways, from the anterior nares to the subglottic region. The level of obstruction can be inferred based on the phase of respiration during which stridor occurs. Stridor arising from pathology in the extrathoracic region of the upper airway (including the nose, pharynx, larynx, and trachea) is more pronounced during inspiration, while stridor originating in the intrathoracic airways (tracheobronchial tree) is usually more prominent on exhalation. If upper airway obstruction at any level is critical and fixed, biphasic inspiratory and expiratory stridor can result. Of note, obstruction of the nares and nasopharynx generally results in low-pitched snoring or “snorting” sounds, often referred to as stertor.
Categorizing Potential Causes for Stridor
Stridor in pediatric patients may occur due to a wide range of disease processes involving the large airways. In considering the differential diagnosis for stridor, it is helpful to “divide” potential causes based on whether the onset is acute or chronic.1 This article focuses on the causes and management of acute stridor.
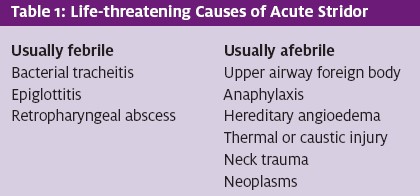
For stridor manifesting acutely, possible etiologies can be further divided into infectious (febrile) versus non-infectious (afebrile) causes. It must be emphasized that stridor can indicate life-threatening upper airway pathology; thus, life-threatening causes must be considered and addressed very early in the evaluation process (Table 1).
Causes of Acute Stridor in the Febrile Child
Differential diagnosis for stridor manifesting acutely in a febrile child includes croup, bacterial tracheitis, epiglottitis, retropharyngeal abscess, and peritonsillar abscess.
Croup
Viral laryngotracheitis (croup) is by far the most common cause of acute stridor in febrile children. Croup is a common childhood illness characterized by acute onset of rhinorrhea, fever, and a distinctive barky cough. It is typically accompanied by hoarseness, inspiratory stridor, and varying degrees of respiratory difficulty resulting from partial upper airway obstruction.
While many different viruses have been associated with croup, it is most commonly associated with parainfluenza type 1. Infection with respiratory viruses leads to generalized inflammation and mucosal edema in upper airway structures, including the larynx, trachea, and bronchi, accompanied by necrosis and shedding of mucosal epithelial cells. The anatomic hallmark of croup is tracheal narrowing due to mucosal edema in the subglottic region.
Croup primarily affects children between 6 months and 3 years of age, although it can occur in younger infants as well as in older children. Cases present throughout the year, but most occur in the fall and early winter months (September to December) in North America. Croup is generally a benign and self-limited illness with population-based studies demonstrating that less than 5% of patients require hospitalization.
Children with severe croup, however, may experience marked respiratory distress. Patients affected most severely may require admission to an intensive care setting and possibly even intubation or surgical airway management. Children with underlying narrowing of the upper airway structures at baseline (such as those with underlying subglottic stenosis from prior intubation) are at risk for significant upper airway obstruction from viral croup, as well as for experiencing recurrent bouts of croup.
The onset of croup in children may be quite frightening for families due to the unexpected and rather unusual presentation.2 Symptom onset is typically abrupt and often happens at night, signaled by development of a harsh, barky cough and noisy breathing following a prodrome of non-specific upper respiratory symptoms. Symptoms increase in severity when children become agitated due to increased airflow turbulence. Children with croup are usually febrile (with temperatures most often ranging from 38 -39° C), but they do not drool or appear toxic.
Alternative etiologies should be considered if a child with stridor presents with drooling or toxic appearance. More than half of croup patients experience resolution of their cough and noisy breathing within 48 hours. A few, how- ever, may display these symptoms for up to a week.
Croup is a clinical diagnosis. Children presenting with the classic signs and symptoms do not require further laboratory or imaging studies to confirm the diagnosis. In cases where the diagnosis is in question, a child’s clinical course is atypical, an inhaled or ingested foreign body is suspected, a child is presenting with recurrent croup, and/or response to therapeutic measures does not occur as expected, plain radiographs of the neck soft tissues and/or chest may aid in confirming the diagnosis. In children with croup, an A-P radiograph of the neck and/or chest will reveal narrowing in the subglottic region, often referred to as the “steeple sign.” A lateral neck radiograph in croup patients may show over-distention of the hypopharynx during inspiration and subglottic haziness.9 The epiglottis should appear normal.
Bacterial tracheitis
Bacterial tracheitis can occur as a primary or secondary infection and may be confused with croup.3 In primary infections, children generally display acute onset of upper airway symptoms (which may include stridor, a painful cough, anterior neck pain, thick airway secretions, dysphagia, and drooling), along with high fever and a toxic appearance.
Secondary infections may rarely arise after acute viral respiratory tract infections, including croup. In cases of secondary infection, children may display symptoms of mild to moderate illness for a few days, followed by a worsening course with onset of high fevers, ill appearance, and increasing respiratory distress.
Children with bacterial tracheitis may develop thick, purulent tracheal exudates that contribute to upper airway obstruction along with concurrent airway inflammation and edema. Staphylococcus aureus is the most frequently isolated pathogen, though a number of other bacterial pathogens have been implicated.
Bacterial tracheitis should be considered as an etiology in any febrile child with acute stridor who displays a toxic appearance, dysphagia, drooling, or purulent upper airway secretions. Children with bacterial tracheitis do not respond as favorably to treatment with nebulized epinephrine as children with simple viral laryngotracheitis; this lack of clinical response thus serves as a further diagnostic clue.4 Bacterial tracheitis management involves airway support and broad- spectrum intravenous antibiotic coverage including coverage for S. aureus (including methicillin-resistant
- aureus). The optimal antibiotic regimen for bacterial tracheitis has not been studied in randomized con- trolled trials. Some experts recommend that initial therapy include coverage for the most commonly isolated pathogens, which include S. aureus, group A streptococcus, Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.10 Suggested broad-spectrum coverage for these organisms includes an anti-staphylococcal agent with coverage for MRSA (such as vancomycin or clindamycin) plus a third-generation cephalosporin.10 Cultures of tracheal secretions should be obtained when possible so that the child’s antibiotic regimen may be tailored as indicated.
Epiglottitis
Acute epiglottitis, an infection of the supraglottic airway structures, is a potentially life-threatening cause of acute stridor in febrile children. Once a relatively common pediatric respiratory emergency, the incidence of epiglottitis in children has plummeted to approximately 0.6 to 0.78 cases per 100,000 in the United States since introduction of the conjugate vaccine against H. influenzae type b (Hib), which caused the majority of cases.6 Despite this dramatic decrease, cases of epiglottitis still occur, even in immunized children. Additional bacterial causes of epiglottitis include other types of H. influenzae, streptococci, and S. aureus.
Children with acute epiglottitis typically appear ill and present with sudden onset of high fever and rapid progression of dysphagia, drooling, and respiratory dis- tress. Affected children generally do not have barking cough but can present with muffled speech, stridor, and a sensation of choking. To compensate for the airway obstruction caused by infection of supraglottic structures, epiglottitis patients may assume a “tripod” position, leaning forward with hyperextension of their necks and opening of their mouths.
Without treatment, epiglottitis can progress rapidly to cause life-threatening upper airway obstruction and respiratory arrest. Examination of children in whom epiglottitis is suspected should occur in a setting where the airway can be secured immediately, if necessary (ideally an operating room or intensive care setting, with personnel experienced in advanced airway management techniques readily available). Such children should be allowed to maintain their positions of com- fort, and any interventions that might precipitate agitation should be avoided.
Soft-tissue neck radiographs can aid in confirming the diagnosis of epiglottitis, although they are unnecessary in many cases. The classic radiographic finding in epiglottitis is the “thumb sign,” referring to the lateral view of the swollen epiglottis resembling the pad of a thumb. The thumb sign is subjective, however, and radiographs alone should not be used to rule out the diagnosis. Radiographs should be deferred if they will agitate the patient or delay definitive diagnosis and management. Children with suspected epiglottitis who need to be transported to the radiology department for imaging should be accompanied by a clinician skilled in airway management. If clinical suspicion is high, imaging should be deferred in favor of direct visualization of the airway under controlled circumstances.
Retropharyngeal abscess
A retropharyngeal abscess, which fills the potential space between the anterior border of the cervical vertebrae and the posterior esophageal wall, is another possible cause of acute stridor in the febrile child. These infections occur most commonly in children younger than 4 years and are usually caused by group A streptococci, anaerobic organisms, and S. aureus.
Children with retropharyngeal abscesses may develop a clinical picture similar to that seen with epiglottitis, with high fever, muffling of the voice, and a toxic appearance; onset is generally less abrupt, however. As purulent material collects in the retropharyngeal space, the abscess obstructs the larynx and esophagus, leading to stridor, voice changes, and drooling.5 Other findings may include sore throat, neck pain (which may decrease neck movement), and cervical lymphadenopathy. Inflammation surrounding the abscess may lead to meningismus; as a result, a number of children with retropharyngeal abscesses have initially been diagnosed with meningitis.
A high index of suspicion must be maintained to accurately identify children with retropharyngeal abscesses. Noting a midline swelling of the posterior pharyngeal wall on examination may help make the diagnosis, but this finding is often difficult to observe in the ill, uncooperative child. If the diagnosis is suspected and the patient’s airway is stable, a lateral neck radiograph and/or contrasted CT scan of the neck should be obtained to confirm the diagnosis. The lateral neck radiograph will show an increase in the width of the soft tissues anterior to the vertebrae and, occasionally, an air- fluid level. A neck CT will help to identify and localize any soft tissue swelling, and it will aid in localizing a retropharyngeal fluid collection. Definitive therapy for children with retropharyngeal abscesses involves intraoperative drainage and intravenous antibiotics to cover the common causative pathogens.
Peritonsillar Abscess
Peritonsillar abscess should be considered in children presenting with signs of upper airway obstruction, although most patients do not present with stridor. Peritonsillar abscesses typically affect adolescents. They are the most common deep infections of the head and neck, usually arising as a complication of bacterial tonsillitis. Pathogens most commonly isolated from these lesions are Group A streptococci, various anaerobic organisms, and occasionally S. aureus.
The findings of trismus, difficulty speaking, and drooling help to separate children with peritonsillar abscesses from those with simple pharyngitis, which is far more common. Examination of affected patients reveals pharyngeal erythema with unilateral tonsillar swelling, which often causes displacement of the uvula toward the unaffected side.5 The examiner may be able to palpate a fluctuant mass intraorally. Reactive cervical adenopathy is also commonly seen.
Peritonsillar abscesses are generally apparent on physical examination; therefore, imaging is not required to confirm the diagnosis. Most patients require admission for drainage, intravenous antibiotics, pain control, and intravenous hydration.5
Causes of Acute Stridor in the Afebrile Child
Differential diagnosis for stridor manifesting acutely in an afebrile child includes upper airway foreign body, thermal or caustic injury, spasmodic croup, anaphylaxis, hereditary angioedema, trauma, neoplasms causing air- way compression, and psychogenic stridor.
Upper airway foreign body
Foreign body aspiration is a relatively common and potentially life-threatening etiology of acute stridor in afebrile children. The majority of cases occur in children younger than 3 years, with the peak incidence between 1 and 2 years of age. At this age, most children can walk, have the fine motor skills to place small objects into their mouths, and possess the developmentally nor- mal tendency to explore their world via the oral route; however, they lack the dentition to chew food adequately and the respiratory effort to clear an aspirated object.7
Young children are at highest risk for significant air- way obstruction from aspirated foreign bodies because of their small airway diameters. In older children, neurodevelopmental disorders, impaired level of consciousness, and substance abuse increase the risk of foreign body aspiration. Food items—including nuts, seeds, popcorn, and hot dog pieces—are the most common items aspirated by infants and toddlers. Non-food items—such as coins, pen caps, paper clips, and small toys—are more commonly aspirated by older children. The presentation of foreign body aspiration varies, depending on whether the event was witnessed by a caregiver, the patient’s age, the size and type of object aspirated, degree of resulting airway obstruction, and the object’s location within the tracheobronchial tree.7 Swallowed foreign bodies that become lodged in the esophagus may also cause stridor and other respiratory symptoms due to compression of adjacent upper airway structures.
Children presenting with abrupt onset of complete upper airway obstruction with severe respiratory distress, cyanosis, and altered mental status have a true airway emergency that mandates rapid recognition of the problem, life support, and immediate removal of the foreign body.7 In less emergent situations (which, fortunately, are much more common), physical examination may reveal stridor, localized wheeze, increased work of breathing, cough, decreased breath sounds, and/or hemoptysis.
Clinicians in the urgent care setting should maintain a high index of suspicion for foreign body aspiration in afebrile children presenting with sudden onset of stridor without preceding symptoms of illness. Caregivers should be directly questioned about any history of choking, as well as about the child’s activities (ie, playing with toys, eating, unsupervised activity) prior to the onset of symptoms. While to elder-aged children are at highest risk for foreign body aspiration, non-ambulatory children may aspirate small objects placed inadvertently into their immediate surroundings or offered to them by older siblings; this possibility should be explored during the history- gathering process as well.
Plain radiographs of the neck and/or chest may or not be helpful in establishing the diagnosis of foreign body aspiration, depending on whether the object is radiopaque and whether airway obstruction is present. The majority of objects aspirated by children are radiolucent (food particles, plastic objects), and are not detected with plain radiographs. Therefore, a normal chest radiograph cannot rule out foreign body aspiration.
In children with suggestive presentations but normal standard chest radiographs, an expiratory chest radiograph (or lateral decubitus radiograph for younger children) or fluoroscopy may be helpful. If foreign body aspiration is highly suspected clinically, with or without confirmation by radiographs, bronchoscopic evaluation of the child’s tracheobronchial tree should be arranged. Rigid bronchoscopy is the ultimate diagnostic tool for foreign body aspiration and is almost always successful in removal of aspirated objects.
Thermal or caustic injury
Both ingestion and inhalation of caustic or thermally damaging substances may result in injury to upper air- way structures and result in stridor. This diagnosis should be considered in any child developing stridor following exposure to a hot or caustic substance.5 Cases of thermal epiglottitis caused by swallowing scalding hot fluids or foods are rare but have been reported in the literature. Symptoms of airway compromise may present up to several hours after an offending exposure. Any child with evidence of significant and/or rapidly progressive upper airway obstruction from a thermal or caustic injury should undergo immediate endotracheal intubation. Delay in securing a definitive airway will only permit further development of airway edema and increase the difficulty of securing the airway.
Spasmodic croup
Spasmodic croup is a variant of croup that lacks the typical viral prodrome (runny nose, low-grade fever). Symptoms start suddenly, often in the middle of the night, and resolve quickly. Symptoms may recur for several nights in a row. The etiology of spasmodic croup is unknown.
Anaphylaxis
Sudden onset of stridor in an afebrile child without associated trauma or choking, especially in the presence of urticaria, facial swelling, pruritus, and/or wheezing, suggests upper airway obstruction resulting from anaphylaxis. This diagnosis may be suggested by history of exposure to an offending allergen prior to symptom onset. Patients with this clinical picture should receive immediate airway, breathing, and circulatory support in conjunction with prompt administration of intramuscular epinephrine and antihistamines.5 The addition of corticosteroids should also be considered. Children presenting with anaphylaxis should be admitted to the hospital for further observation and management.
Hereditary angioedema
Though rare, hereditary angioedema may present in childhood, and exacerbations may cause acute stridor secondary to laryngeal edema. Patients often have a family history of this condition. Attacks can result in painless swelling of the upper airway, extremities, face, and/or genitalia that is not associated with urticaria. Although a new medication is available to correct the underlying deficiency of C1 esterase inhibitor in hereditary angioedema patients, fresh frozen plasma may also be used to treat acute attacks.
Trauma
Blunt or penetrating trauma to the neck may result in mucosal lacerations, laryngeal or tracheal hematomas, vocal cord paralysis, or fractures of the thyroid and cricoid cartilages.1 Patients with traumatic injuries to upper airway structures often present with varying
degrees of neck pain, stridor, hoarseness, hemoptysis, and respiratory distress. Physical examination of children with blunt trauma may reveal anterior neck tenderness, crepitus, tracheal deviation, and absence of the normal prominence of the thyroid cartilage. Proper treatment of upper airway injuries requires prompt recognition and stabilization of the airway. For children with suspected upper airway injuries, an otolaryngologist or similarly skilled specialist may be needed to evaluate the upper air- way structures and to intervene with intubation, establishment of a surgical airway, and/or definitive surgical management of any injuries present. Children with penetrating neck injuries may require angiography or magnetic resonance imaging (MRA/MRV) to evaluate for potential vascular injury.
Neoplasms Causing Airway Compression
Mediastinal neoplasms may present with respiratory symptoms, including stridor, secondary to airway obstruction or erosion. At least one-third of all mediastinal masses occur in children younger than 15 years of age. Patients may display cough, wheezing, recurrent respiratory infections, hemoptysis, chest pain, and even syncope or sudden death. Children with neoplasms impacting the airway should be hospitalized to undergo urgent evaluation, as these tumors and their associated mass effect may be potentially life-threatening.
Psychogenic Stridor
Though uncommon, psychogenic stridor may be a potential etiology of acute stridor in older children. Most cases have been reported in adolescents, with girls diagnosed more commonly than boys. Many children with psychogenic stridor meet diagnostic criteria for another psychiatric disorder. Patients typically display stridor that manifests acutely, but without the expected amount of associated respiratory distress. The stridor may be triggered by a distressing event and characteristically improves when the patient is unaware of being observed. Diagnosis may be confirmed by direct laryngoscopy in the symptomatic child, which reveals vocal cord adduction during inspiration.
Evaluation and Management of Acute Stridor
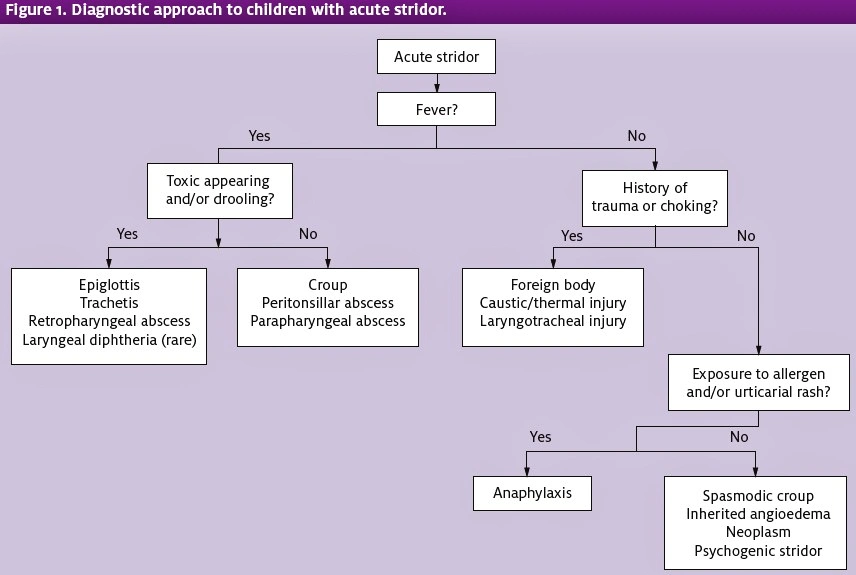
The initial priority in evaluating and managing any child presenting with acute stridor is ensuring the adequacy of the airway, breathing, and circulation and promptly instituting resuscitative measures as necessary. Once the ABC’s are determined to be adequate and stable, further evaluation and treatment may continue in a systematic fashion (Figure 1).
Because stridor serves as a sign of partial upper airway obstruction and can arise from life-threatening causes, children with stridor should be approached as gently as possible to avoid agitation, particularly during the early stages of evaluation while airway adequacy is being ascertained. Young children should be allowed to stay with their caregivers, and all patients should be allowed to remain in their preferred positions of comfort.
Interventions causing agitation in the stridorous child may lead to further airway compromise and/or worsening respiratory distress. During the initial assessment of a child with stridor, the clinician should note the child’s position of comfort and ease of movement; reluctance of the child to move out of a certain position may serve as a “red flag” of significant upper airway obstruction. For example, a child with significant upper airway obstruction may hyperextend his or her neck and lean forward to straighten the upper airway and maximize air entry (“sniffing position”). If such a finding is noted, the child should be kept as calm as possible in his or her preferred position until a clinician skilled in airway management is present and preparations have been made to secure the child’s airway in a controlled manner, if necessary.
As with all other pediatric complaints, a history and physical examination are invaluable aids in identifying the underlying cause for stridor. For children with acute stridor, the history should focus on associated symptoms such as fever, duration of illness, change in voice, drooling, rhinorrhea, cough, urticaria, and any history of choking. Immunization status should be verified, especially vaccination against Hib.
In addition to a careful respiratory examination focusing on adequacy of air movement and the child’s work of breathing, the physical examination should include inspection of the nares and oropharynx, with particular attention to increased secretions, drooling, uvular deviation, visible bulging/masses, and abnormal phonation. Regional findings such as adenopathy, neck masses, meningismus, bruising, and other evidence of trauma should also be noted. As noted earlier in the section on pathophysiology, several characteristics of stridor—including its pitch, length of respiratory phase, and associated phase of respiration—can aid in deter- mining the level of airway obstruction.
Emergency management of children with acute stridor depends on the underlying etiology and degree of associated respiratory compromise. Recommended strategies for management of various pathologies causing stridor were briefly discussed earlier. A more in-depth discussion of two common pediatric conditions causing acute stridor croup and foreign body aspiration—is provided here.
Management of Acute Laryngotracheitis (Croup)
Most children with croup can be managed successfully as outpatients. Three major goals for acute croup therapy are to decrease airway inflammation and edema, provide respiratory support, and maintain adequate hydration.
The mainstays of acute croup management are corticosteroids and nebulized epinephrine. Corticosteroids have a well-established history of use in children with croup, with clear evidence for their effectiveness.2 A
compilation of clinical trial data reveals significant ben- efits for croup patients treated with corticosteroids, including decreased clinical croup scores, lower risk of intubation, and reduced duration of symptoms, even in patients with mild illness. The standard recommended corticosteroid regimen for children with croup is single- dose dexamethasone 0.6 mg/kg, which may be given orally, intramuscularly, or intravenously. Repeat corti- costeroid doses have no proven benefit for croup patients and are not routinely recommended.
Treatment of children with moderate to severe croup with nebulized epinephrine has been well-studied and found to reduce clinical croup severity and the need for invasive airway support.2 Thus, nebulized epinephrine is recommended for patients with moderate to severe croup, including those with stridor at rest and moderate to severe retractions. Racemic epinephrine has traditionally been utilized in croup management, but L- epinephrine 1:1,000 is as effective and safe. In most studies, the standard nebulized epinephrine dose used in children of all ages is 0.5 mL of 2.25% racemic epinephrine solution, or 5 mL of 1:1,000 L-epinephrine. Children demonstrating clinical improvement after administration of nebulized epinephrine must be observed for a minimum of 2-3 hours in the urgent care setting for occurrence of the “rebound phenomenon”— the tendency for patients’ symptoms to return as the effects of epinephrine wear off.
If the urgent care facility is unable to provide necessary observation, then transfer to an emergency facility should be initiated. The decision for patient transfer, however, should not delay initiation of treatment. The urgent care setting should therefore be comfortable with the administration of nebulized epinephrine, when indicated.
Those children failing to improve clinically after administration of nebulized epinephrine or demonstrating recurrence of moderate to severe symptoms during their periods of observation should be hospitalized.
Management of Foreign Body Aspiration
For any child presenting with complete obstruction of the upper airway by a foreign body, dislodgement of the object should be attempted using alternating cycles of back blows and chest compressions in infants, and abdominal thrusts in older children in accordance with the American Heart Association (AHA) guidelines.8 These maneuvers should not be used in children who are able to cough or speak as they may worsen the degree of airway obstruction. The use of “blind” mouth sweeps in an attempt to remove an aspirated object should also be avoided.
For children who become unresponsive despite dislodgement attempts, CPR beginning with chest com- pressions should be instituted immediately according to AHA guidelines.8 Emergent subspecialist consultation for removal of the foreign body by rigid bronchoscopy should be obtained. Endotracheal intubation may allow some ventilation until rigid bronchoscopy is possible, and oxygen and other basic life support measures should be provided until the obstruction can be relieved.7 If a foreign body is apparent to the urgent care clinician on visualization of the mouth or upper airway, forceps may be used to remove the object.
For stable children with suspected foreign body aspiration or ingestion, radiographic studies may be obtained to help confirm the diagnosis. Those in whom the diagnosis is highly suspect should undergo rigid bronchoscopy to identify and remove the foreign object. ■
REFERENCES
- Perry Stridor. In: Fleisher GR, Ludwig S, eds. Textbook of Pediatric Emergency Medicine. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:584-588.
- Bjornson CL and Johnson Croup. Lancet. 2008;371(9609):329-339.
- Cantor Upper Airway Emergencies. In: Strange GR, Ahrens WR, Lelyveld S, Schafer- meyer RW. Pediatric Emergency Medicine: A Comprehensive Study Guide. 2nd ed. Chicago, IL: McGraw-Hill; 2002:197-205.
- Kost Stridor. In: Selbst SM and Cronan K, eds. Pediatric Emergency Medicine Secrets. 2nd ed. Philadelphia, PA: Mosby Elsevier; 2008:179-183.
- Loftis Emergent evaluation of acute upper airway obstruction in children. Accessed June 15, 2011.
- Woods Epiglottitis (supraglottitis): clinical features and diagnosis. Available at: www.uptodate.com/contents/epiglottitis-supraglottitis-clinical-features-and-diagnosis. Accessed June 15, 2011.
- Ruiz Airway foreign bodies in children. Available at: http://uptodate.com/contents/air- way-foreign-bodies-in-children. Accessed June 15, 2011.
- Berg MD, Schexnayder SM, Chamedies L, et Pediatric basic life support: 2010 Amer- ican Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Car- diovascular Care. Pediatrics. 2010;126(5);e1345-e1360.
- Woods CR. Clinical features, evaluation, and diagnosis of croup. Available at: http://www.uptodate.com/contents/clinical-features-evaluation-and-diagnosis-of- croup?source=search_result&selectedTitle=2%7E58#H1. Accessed June 20,
- Woods Bacterial tracheitis in children: treatment and prevention. Available at: http://www.uptodate.com/contents/bacterial-tracheitis-in-children-treatment-and-prevention?source=search_result&selectedTitle=2%7E150#H13. Accessed June 20, 2011.

