Urgent message: As the population of seniors swells, more cases of senile dementia, delirium, and psychosis are apt to present in urgent care. Here is how to assess and manage altered mental status patients in the urgent care setting.
RAUL E. RODON, MD
Introduction
Evaluating patients presenting with altered mental status in the urgent care setting requires a modified skill set, one that varies from the assessment of patients with a similar profile in a hospital emergency department. Limited access to standard and immediate laboratory test results, including CT and MRI imaging in many urgent cares, often complicates the appropriate and complete evaluation of these patients.
“Altered mental status” is a term that denotes an undifferentiated assortment of disorders of mentation. These disorders may include impaired cognition, attention, awareness, and level of consciousness. Alterations may be transient, sustained, fluctuating, or progressive. Altered mental status is not an uncommon complaint in urgent care.
Perspective on Disorders of Cognition
Mental status impairment is particularly prevalent among elderly patients, and these patients may carry an increased risk for adverse outcomes subsequent to discharge. Patients with delirium often have acute underlying illnesses and have been shown to have higher morbidity and mortality rates than their counterparts without delirium.
Patients with dementia may have difficulty with medication and discharge instruction compliance, which can also result in increased morbidity and mortality. In addition, the presentation of impaired mental status in elderly individuals might be subtle and go unrecognized, making it a challenge for the unsuspecting physician to detect.
While a standard presented complaint in urgent care, altered mental status is also a common underlying condition in patients presenting with other primary complaints. Although alterations in mental status occur in patients of all ages, the elderly are at especially high risk. Other risk factors include prior cognitive impairment, underlying chronic disease, and systemic infection. One study showed altered mental status to be present in 40% of patients older than 70 years of age.1 Approximately 25% of patients with altered mental status had alterations in levels of consciousness; 25% had delirium, and 50% had cognitive impairment without delirium.
Signs and Symptoms
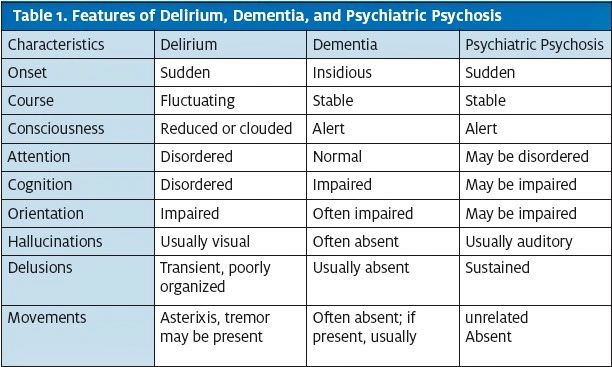
Delirium, dementia, amnesia, and certain other alterations in cognition are subsumed under more general terms such as mental status change (MSC), acute confusional state (ACS), or organic brain syndrome (OBS). Organic brain syndrome can be divided into two major groups: acute (delirium or acute confusional state) and chronic (dementia) (Table 1).
The final pathway for all forms of organic brain syndrome is an alteration in cortical brain function. This condition results from an exogenous insult or an intrinsic process that affects cerebral neurochemical functioning or physical or structural damage to the cortex. Some etiologies include trauma, mass lesions, hydrocephalus, stroke (ie, multi-infarct dementia), atrophy, infection, toxins, or dementing processes.
The prevalence of dementia doubles every five years between the age 60 to about age 90, with 1 percent of individuals 60-64 years old developing dementia and up to 30%-50% of individuals over 85 years old experiencing a decline in intellectual faculties. Approximately 60% of nursing home beds are occupied by patients diagnosed with dementia.
History
MSCs may evolve acutely, with rapid, fluctuating, and usually transient course (delirium), or they may advance insidiously and inexorably over months or years with gradual worsening or stuttering course (dementia).
Delirium
Delirium presents with acute onset of impaired awareness, easy distraction, confusion, and disturbances of perception, which may include illusions, misinterpretations, or visual hallucinations. Recent memory is usually deficient, and the patient is typically disoriented as to the present time and place. The patient may also appear agitated or obtunded and the level of awareness may fluctuate over brief periods. Speech may be incoherent, pressured, nonsensical, perseverating, or rambling, which may complicate a physician’s capacity to perform and obtain an accurate medical history from the patient or make it impossible. However, such a patient is most likely to present at an ED.
If you do get an individual with delirium, it is important to attempt to obtain a current and past history of the patient from other available resources, including family or friends of the patient and/or past medical records. The information should include time and acuity of onset, trauma (including falls), fluctuations of symptoms, course over time, and possible environmental exposure (eg, carbon monoxide). In addition, obtain information regarding associated symptoms, including headaches, fever, seizure, change in speech, and changes in the habits of daily living.
Specifically look for indications and signs of street drug, alcohol, and medication use and abuse; pre-existing endocrine disorders; and recent activities that may have resulted in exposure to toxins or environmental injury. It is also critical to inquire about prior psychiatric illness and similar episodes of confusion in the past.
Dementia
Individuals with dementia present with a history of chronic, steady decline in short-term and, later, long-term memory. Dementia is associated with difficulties in social relationships, work, and activities of daily life. In contrast to delirium, the sensorium is clear. However, an acute confusional state can be superimposed onto an underlying dementing process. The patient who presents with moderate to severe symptoms has usually been previously diagnosed. Such patients most commonly present in the urgent care setting, and most of the time, dementia is accompanied by other chief complaints.
Earlier states of dementia may appear understated in presentation, and patients may minimize or attempt to hide their impairments. Often, patients at this stage have an associated depression. Depression alone can present as a dementia-like condition in elderly patients. Of note, a recent study indicated dementia of relatively recent onset had higher likelihood of a potentially reversible etiology.2 It is essential to conduct a careful medical history of the patient—particularly noting signs of past or present drug or alcohol abuse, current medications, chronic or acute medical illnesses, and psychiatric disorders—to uncover a treatable or modifiable cause for the cognitive impairment.
Elderly patients with depressed mood, hopelessness, and suicidality may be suffering from “pseudodementia” (false dementia). When the depression is alleviated with treatment, the dementia-like condition fully resolves.
Examination Any patient who presents with an altered mental status needs a complete physical examination, with particular attention to general appearance, vital signs, hydration status, evidence of physical trauma, and neurologic signs. All patients should have an exam done in the urgent care even if they are being prepared for emergent transport to an ED. Evaluation and simple diagnostic tests could be performed while waiting for EMS to arrive.
General appearance (eg, unkempt and/or malnourished) may suggest the possibility of drug or alcohol abuse. Studies have shown a correlation between tattoos and substance use and abuse in adolescents.3,4 In the author’s experience, this correlation exists at all ages. Other trace marks for substance abuse include:
- Smell of alcohol, the musty odor of fetor hepaticus, or the fruity smell of ketoacidosis
- Icterus and asterixis point to liver failure with an elevation of the serum ammonia level
- Agitation and tremulousness suggest drug and alcohol withdrawal
Close attention to vital signs is essential. Vital signs are easy to overlook in the setting of extreme behavioral difficulties in a delirious patient.
The Mini-Mental Status Examination (MMSE) is a formalized way of documenting the severity and nature of mental status changes. The MMSE, modified from Folstein, is outlined below.5 The maximum score per item is indicated in parentheses.
- Orientation (five points): What are the year, date, day, and month?
- Orientation (five points): Where are we? State? Country? Town? Hospital? Floor?
- Registration (three points): Name three objects. Ask the patient to repeat the names of these three objects
- Attention and calculation (five points): The serial seven test (counting down from 100 by sevens) awards one point for each correct answer. Stop after five answers. Spelling word backward is optional
- Recall (three points): Ask for the three objects from the registration test (item three in this list) to be recalled. One point is scored for each correctly recalled object
- Language (two points): Name a pencil and a watch
- Repetition (one point): Repeat the following: “No ifs, ands, or buts” Complex commands (six points): Follow a threestage command, such as: “Take a paper in your right hand, fold it in half, and put it on the floor”
- Complex commands (three points): Read and follow these printed commands: “Close your eyes” (one point); “Write a sentence” (one point); and “Copy a design” (one point)
Causes
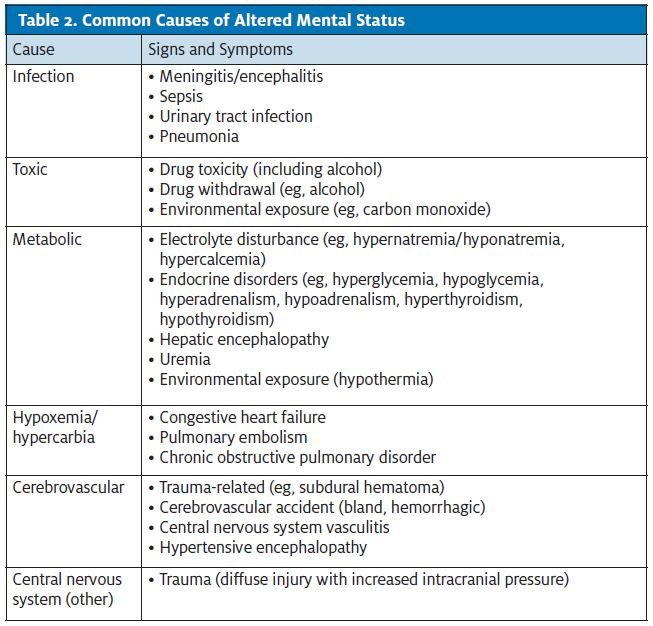
Common causes of altered mental status include infection, toxic reactions, metabolic disturbances, hypoxia/ hypercarbia, cerebrovascular conditions, and central nervous system conditions (Table 2).
Evaluation and Treatment
Obtaining an accurate and thorough medical history of a patient with altered mental status is an essential component of the database that must be collected at a time when the patient is least able to provide it. In patients with an alteration in cognition, the alteration may be subtle and may not be evident to the physician on initial evaluation, making it fundamental to interview the patient’s family members, friends, care providers, etc., regarding the patient’s baseline for normality. For many patients with altered mental status, a timely history may not be available and practicable. In the absence of knowledge of the patient’s condition, it must be assumed to be an acute change from baseline. Even when information is available, it is imperative to not accept a predetermined diagnosis without adequate consideration of the medical history, physical examination, and selected diagnostic studies.
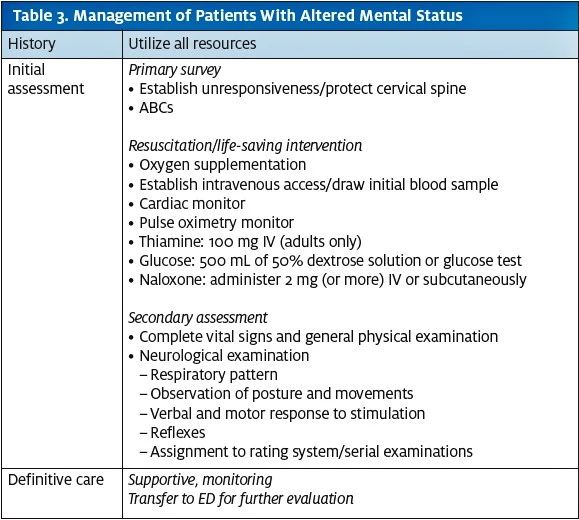
For all patients with altered mental status, initial consideration should focus on airway adequacy and potential for cervical spine injury. All patients also require rapid glucose determination/dextrose administration and oxygen saturation measurement, which should be available at any urgent care.
Of note, considerable controversy exists concerning routine use of the “coma cocktail” (thiamine, glucose, and naloxone), as the medical literature suggests that glucose may be detrimental to brain ischemia; routine use should be guided by the clinical situation and rapid glucose determination. Adverse effects of naloxone and thiamine are strongly outweighed by their benefits when there is reasonable suspicion of opioid overdose or nutritional deprivation (Table 3).
In the emergent evaluation of patients with altered mental status, the most available imaging study is currently non-contrast brain CT. Most urgent cares lack this imaging capability. Patients who require it should be transferred to an ED.
Disposition
The potential for serious clinical consequences in patients with mental status impairment is considerably high. Patients suffering from dementia and its associated symptoms may have difficulty accurately communicating their history of present illness and may sometimes omit important details that might lead to suboptimal care. The presence of dementia in the elderly patient can also affect medication and discharge instruction compliance, increasing the risk of morbidity and mortality after discharge.
Although less than 1% of all dementia is considered potentially reversible, individuals diagnosed with chronic and degenerative dementia may still benefit from a variety of treatment options that slow disease progression and prolong independence. Early referral of these patients for further evaluation and treatment may be beneficial. It is important to recognize that patients with dementia are also at increased risk for falls, which can possibly be prevented with vigilance and timely intervention (eg, medication reviews, home safety assessment, etc.) that might reduce this risk and possibly pre-empt further injury.
Delirium is an acute medical emergency. Strong consideration should be given for referral and admission of these patients to the ED.
Conclusion
Altered mental status has a long differential diagnosis that includes many life-threatening conditions. Medical history from both the patient and bystanders is the key diagnostic tool in urgent care to determine whether a patient requires further evaluation and treatment. Physical examination plays a role comparable to other ancillary testing available in urgent care, such as rapid glucose testing, chest x-ray, urinalysis, etc.
Most patients presenting with altered mental status need a thorough evaluation in the ED. If a life-threatening condition is suspected, patients should be transported immediately via the EMS system.
References
- Naughton BJ, Moran MB, Kadah H, et al. Delirium and other cognitive impairment in older adults in an emergency department. Ann Emerg Med. 1995;25(6):751-755.
- Geldmacher DS, Whitehouse PJ. Current concepts: evaluation of dementia. N Engl J Med. 1996;335(5):330-336.
- Roberts TA, Ryan SA. Tattooing and high-risk behavior in adolescents. Pediatrics. 2002;110(6):1058-1063.
- Brooks TL, Woods, ER, Knight JR, Shrier LA. Body modification and substance abuse in adolescents: is there a link? J Adolesc Health. 2003;32(1):44-99.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198.
Raul E. Rodon is owner of North Atlanta Urgent Care in Atlanta, Georgia (www.northatlantaurgentcare.com). He attended medical school at Universidad de Zulia in Maracaibo, Venezuela, and was trained as an emergency physician at Emory University in Atlanta. He is board certified in emergency medicine.
Citation: R Rodon. Altered Mental Status in the Urgent Care Patient. J Urgent Care Med. 2011; 6(3): 9-14.

