Urgent message: Acute rheumatic fever is not common but it does still occur, underscoring the need for head-to-toe examination in patients with vague symptoms that seem unconnected.
HEATHER VARLEY, PA-C, and WILLIAM GLUCKMAN, DO, MBA, FACEP
Introduction
Patients with fever, sore throat, and malaise often present in the urgent care setting and they typically are worked up quickly with a rapid strep test or given a diagnosis of a viral syndrome. The case described here is an example of how important it is to listen carefully to all patients with such straight-forward symptoms and to evaluate them head to toe in order to draw connections between a range of common symptoms. It highlights the importance of thinking outside the box and keeping in mind conditions that may not be as common today as they were 50 years ago. The condition described here is not often encountered in everyday medical practice in the United States as it used to be, but it is one that should always considered in order to make an accurate diagnosis and reduce adverse outcomes.
Case Presentation
EW is a 56-year-old male who presented to the urgent care with low-grade fever ranging from 99.0° F to 101.0°F for 10 days, accompanied by malaise, myalgia, and severe diffuse joint pain. His polyarthralgia was noted to be most severe in both knees and wrists. He reported noting a diffuse red raised rash on his chest, back, bilateral legs, arms, and hands that was neither pruritic not painful. He complained of moderate sore throat, intermittent headache, nasal congestion, and intermittent dyspnea on exertion as symptoms related to the current presentation. After further questioning, the patient revealed that he had noted a mild to moderate sore throat intermittently over the past 3 weeks but did not seek treatment. The remained of the history was found to be unremarkable. The patient reported no significant past medical history and no daily medications. Observation/Findings
Evaluation of the patient showed the following:
- T: 98.9°F
- RR: 18
- P: 96 bpm
- BP: 143/92
- O2: 96% RA
- Weight: 210 lb Height: 6’ 0”
Physical exam revealed a well-developed male in no acute distress. Positive exam findings included a diffuse maculopapular rash with mild superficial excoriation noted on bilateral arms, legs, hands, and trunk. Pharynx and tonsils were severely erythematous with mild swelling and no exudate (Figure 1). Submandibular and anterior cervical lymphadenopathy without tenderness was noted bilaterally. Examination of the extremities revealed mild swelling and erythema of the patient’s left wrist and bilateral knees, without significant tenderness, limited range of motion or decreased strength. The heart was normal s1s1 without murmurs or rubs. The patient’s lungs were clear bilaterally and there was no jugular venous distension. His abdomen was soft, nontender and without organomegaly.
Diagnostic Studies
Tests performed in the office included the influenza A/B test, which was negative, and the Rapid Streptococcus Type A antigen test, which was positive.
Diagnosis
Acute Rheumatic Fever
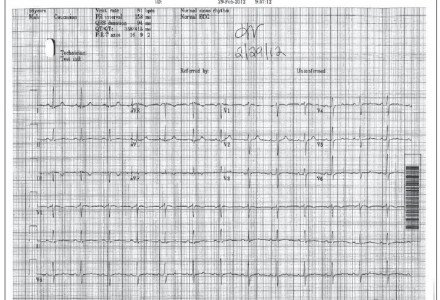
Based upon clinical suspicion for this diagnosis, further testing was completed in the office. An electrocardiogram (EKG) was performed which demonstrated a normal sinus rhythm, with no acute ST changes and no evidence of heart block (Figure 2). Blood was drawn and sent for a complete blood count (CBC) and measurement of C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), lyme antibody, apha-hemolytic streptococci (AH), antistreptolysin O (ASO), and antideoxyribonuclease b (ADB). The patient was given a prescription for an outpatient echocardiogram to rule out involvement of heart valves and to assess cariad output.
Lab results demonstrated an elevated white blood count (WBC) to 14.34 with bands, significantly elevated hsCRP to > 100.0, as well as elevated CRP, ASO, ESR, and rheumatoid factor.
An outpatient echocardiogram subsequently revealed normal systolic function, overall normal valve function with trace tricuspid and aortic insufficiency, and mild mitral regurgitation.

Course and Treatment
The patient was prescribed amoxicillin 875 mg twice daily for 10 days to treat the strep infection. He was put on a prednisone taper for 10 days in order to treat the generalized inflammatory process associated with this condition. Acetaminophen and hydrocodone was prescribed for severe joint pain. The patient was referred to both an infectious disease specialist and a cardiologist for further evaluation and management. His symptoms completely resolved within 2 weeks after initiation of therapy.
Discussion
Acute rheumatic fever (ARF) is a systemic autoimmune process that develops in response to an untreated group A streptococcal pharyngitis infection. Strep pharyngitis is the only streptococcal infection associated with ARF. Streptococcal infections in other parts of the body have not demonstrated the same connection with the onset and development of ARF. ARF is characterized by inflammatory lesions of the joints, heart, subcutaneous (SQ) tissue, and the central nervous system. The likelihood of developing ARF after an occurrence of strep pharyngitis has been estimated at about 0.3% to 3%.
Overall, the incidence of ARF in developed nations has declined significantly over the past 50 years. This can be attributed to improved hygiene and aggressive treatment of strep pharyngitis, a clinical condition commonly encountered in the urgent care setting. ARF is most commonly noted in children aged 5 to 14 years, and is less common in those over 35. The symptoms of ARF typically begin to develop 2 to 3 weeks after the onset of pharyngitis, carditis, chorea, erythema marginatum, fever, and sore throat. Signs include heart murmurs, cardiomegaly, rash, indications of congestive heart failure or pericarditis. The most detrimental sequelae of ARF is rheumatic heart disease. Rheumatic heart disease is the condition responsible for much of the morbidity and mortality caused by this disease process.
The Jones Criteria have classically been used to make a diagnosis of ARF. Makor criteria include carditis, polyarthritis, chorea, erythema marginatum, and/or SQ nodules located over bones or tendons. Minor criteria include fever, arthralgia, previous rheumatic fever or rheumatic heart disease, acute phase reactions (leukocytosis, elevated ESR/CRP), and/or prolonged P-R interval on EKG. For diagnosis of ARF using the Jones Criteria, two major and two minor criteria must be met, in addition to evidence of a recent strep infection. It should be noted that if a strong clinical suspicion remains, and not all criteria have been satisfied, an appropriate work-up and treatment plan should still be implemented. It is important to keep this diagnosis in mind of a patient presents with any of the above signs or symptoms, even if the patient cannot clearly remember having a sore throat prior to the onset of the presentation.
The work-up for a patient with possible ARF includes measures to diagnose the condition, as well as those to exclude and identify the potential complications associated with the disease process. A throat culture should be performed; however it should be noted that only 25% of patients have a positive throat culture at the time of diagnosis of ARF. Blood culture should be drawn to include CBC, ASO titers, deoxyribonuclease B, and anti-hyaluronidase lab tests. An EKG should be performed in the office to evaluate for cardiomegaly or potential heart block. AN echocardiogram is essential to evaluate the heart valves and rule out rheumatic heart disease. The most common abnormal findings on echo noted in EHD are mitral regurgitation and aortic insufficiency.
Penicillin is the treatment of choice for treating the underlying streptococcal pharyngitis associated with ARF, because of its narrow spectrum of activity and the decreased likelihood of Group A Streptococcus resistance. For penicillin-allergic patients, a narrow-spectrum cephalosporin, clindamycin or a macrolide can be used. Anti-inflammatories including nonsteroidal anti-inflammatories or steroids are used to treat the inflammatory response in ARF. Aspirin and other non-opiate or opiate analgesics are used to reduce joint pain, which can be severe. If a patient presents with chorea, valproate sodium or haloperidol can be administered. The rash and SQ nodules sometimes associated with the condition are usually self-limited and don’t require treatment, however, antihistamines can be used if there is any associated pruritus. A patients’ immediate family and close contacts should have throat culture appropriate antibiotic treatment if they test positive.
Acute attacks usually last about 12 weeks and usually leave no long-term damage to the brain, joints or skin, but cardiac effects may persist. ARF patients who develop endocarditis usually require short-term follow up with an infectious disease specialist, and long-term follow up with a cardiologist. Patients who have had ARF need to be counseled on the need for prophylaxis during future illnesses and medical procedures in order to decrease the likelihood of recurrence of the condition. People who have had ARF in the past are much more likely to develop ARF with future episodes of group A streptococcal pharyngitis.
ARF can have a very variable presentation and be difficult to diagnose because of the lack of a specific diagnostic confirmative test. ARF is a strong example of the importance of taking a detailed history and performing a thorough head-to-toe exam when a patient presents with vague, seemingly unconnected symptoms. The patient here presented with a range of symptoms, and eliciting a history of a sore throat intermittently over the course of a few weeks was important in bringing the possibility of a diagnosis of ARF to the forefront. Strong clinical suspicion based on signs and symptoms, and appropriate work-up to identify and treat potential complications associated with ARF are necessary when managing a patient with this complex condition.
References
- Gerber M, Baltimore R, Eaton C, et al. Prevention of rheumatic fever and diagnosis and treatment of acute streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translation Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics Circulation. 2009; 119(11): 1541-1551.
- Gibofsky A, Zebriskie J. http://www.uptodate.com/contents/epidemiology-and-pathogenesis-of-acute-rheumatic-fever?source=search_result&search=rheumatic+fever&selectedTitle=3-83 Accessed June 22, 2012.
- Ferrieri P. Proceedings of the jones criteria workshop. Circulation. 2002; 106: 2521-2523.
- Meador R. Acute rheumatic fever. Medscape website. Available at: http://emedicine.medscape.com/article/333103-overview. Accessed June 22, 2012.
- Mirkinson L. The diagnosis of rheumatic fever. Pediatr Rev. 1998; 19(9): 310-311.

