Published on
Urgent message: Approximately one quarter of pediatric ambulatory visits result in antibiotic prescriptions, with over one third of those exceeding guideline-recommended durations. Factors that influence urgent care providers toward longer durations have not been studied previously.
Megan Hamner, MD; Amanda Nedved, MD; Holly Austin, MD; Donna Wyly, RN, MSN, CPNP-AC, PPCNP-BC; Alaina Burns, PharmD, BCPPS; Brian Lee, PhD, MPH; and Rana E. El Feghaly MD, MSCI
Citation: Hamner M, Nedved A, Austin H, Wyly D, Burns A, Lee B, El Feghaly RE. Antibiotic duration for skin and soft tissue infections in pediatric urgent care. J Urgent Care Med. 2022;17(3):27-32.
Keywords: cellulitis, abscess, duration, antimicrobial stewardship, pediatric urgent care
ABSTRACT
Objective: National guidelines recommend a 5–7-day course of antibiotics for most skin and soft tissue infections (SSTI)s. Our goal was to evaluate the baseline rate of oral antibiotic duration for SSTIs in our pediatric urgent care clinics (UCCs) and interrogate factors that influence providers towards longer durations.
Methods: We evaluated all patient encounters with a diagnosis of SSTIs from three pediatric UCCs between June 2019 and June 2020. Data included patient age, concomitant diagnoses, antibiotics prescribed, and their duration. We excluded encounters if the patient was younger than 3 months of age, transferred to the emergency department or admitted, no oral antibiotics were prescribed, or if there was a concurrent diagnosis requiring antibiotics. We also sent out a 22-question survey to urgent care providers to gain an understanding of prescribing habits, focusing on factors prompting longer antibiotic courses.
Results: We reviewed 2,575 encounters in our study period, out of which 2,039 (79.2%) met our inclusion criteria. Of those, 822 (40.3%) included an oral antibiotic prescription for greater than 7 days while 1,181 (57.9%) included an oral antibiotic prescription for 5-7 days. The survey was sent to 50 providers, with 27 responding (a 54% response rate). Barriers for shorter treatment courses included concern for acute rheumatic fever development, parental pressure, fear of complications, and accustomed antibiotic duration.
Conclusion: Forty percent of children with SSTIs seen in our UCCs received unnecessary long courses of antibiotics. Antibiotic duration would be a good target for future quality improvement interventions.
INTRODUCTION
Antimicrobial stewardship programs (ASPs) in the inpatient setting have successfully refined antibiotic prescribing habits leading to advances in patient safety and improved outcomes.1 Approximately one quarter of pediatric ambulatory visits result in antibiotic prescriptions2; over a third of these exceed guideline-recommended durations.3
In their joint statement, the American Academy of Pediatrics and the Pediatric Infectious Diseases Society identified outpatient pediatrics, including urgent care clinics, as an important target of ASP initiatives.4 Skin and soft tissue infections (SSTIs) are the second most common diagnosis leading to pediatric antibiotic prescriptions in the outpatient setting, after respiratory diagnoses.2 Multiple studies have shown that a short (5-7-day) course of antibiotics is sufficient for children with SSTI,5-8 and current guidelines recommend 5-7 days for most diagnoses9, 10; however over 75% of children diagnosed with SSTI received a prolonged >7 days of oral antibiotics.3, 9
In this study, we aimed to evaluate the antibiotic duration appropriateness for children seen in our pediatric urgent care clinics (UCCs) with SSTIs, and to explore factors that influence providers toward longer durations. In our effort to improve outpatient antimicrobial use in our institution, these data were used to determine whether SSTI antibiotic durations would be a good target for future quality improvement (QI) interventions.
METHODS
Our organization has three pediatric UCCs located throughout a midwestern metropolitan area with over 90,000 encounters a year. The UCCs are staffed by board-certified general pediatricians and advanced-practice registered nurses. We conducted a retrospective chart review of all UCC visits with a final diagnosis of SSTI (Appendix 1) between June 2019 and June 2020. We collected patient and clinical demographics, including age, weight, concomitant diagnoses, antibiotics prescribed, dose, duration, and any return visits with a diagnosis of SSTIs within 14 days. These data were obtained from the electronic health record via International Classification of Diseases (ICD) 10 codes for common SSTIs and were then validated through chart review. We excluded encounters when patients were admitted or transferred to the emergency department, patients were <90 days of age or >21 years of age, no antibiotics or only topical antibiotics were prescribed, or patients had concomitant diagnoses that may require antibiotics.11
We reviewed return visits to determine the outcome of the visit. If a patient returned for an SSTI such as cellulitis or abscess and was prescribed a new antibiotic, both their original encounter and the return encounter were counted. If patients did not receive a new antibiotic prescription or were only prescribed a topical antibiotic, the return encounter was excluded.
In addition, we developed an anonymous 22-question provider survey using REDCap to better understand prescribing habits, particularly focusing on factors prompting administration of longer antibiotic courses (Appendix 2).
This survey included a mix of questions including evaluation of provider comfort level with diagnosing and treating SSTIs and with prescribing short courses of antibiotics for SSTIs, and evaluation of their current practice with antibiotic duration for SSTIs. We also provided free text boxes for providers to expand on factors that may prompt longer antibiotic durations. The survey was evaluated by four urgent care providers for clarifications and feedback before it was deployed by email to all UCC providers in mid-July 2020. We use descriptive statistics to share our results, and control charts to display month-to-month data.
This study received exempt status by our institutional review board.
RESULTS
During our study period, we reviewed 2,575 individual encounters. We excluded 536 (20.8%) patients; 66 were admitted or transferred to the emergency department, 15 were younger than 90 days of age, 68 received no antibiotic prescription, 328 only received topical antibiotic prescriptions, and 59 had concomitant diagnoses that may require antibiotics. Our final analysis included 2,039 encounters.
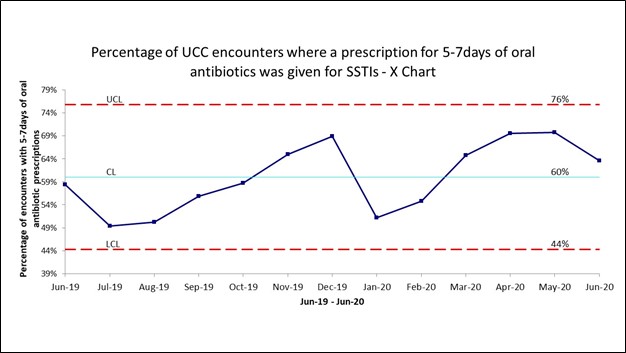
Most common antibiotics prescribed included cephalexin, clindamycin, and trimethoprim-sulfamethoxazole. Of those, 1,181 (57.9%) included an oral antibiotic prescription for 5-7 days with a monthly mean of 60% (control limits: 44-76%) on the control chart (Figure 1), while 822 (40.3%) included an oral antibiotic prescription for greater than 7 days with a mean of 38% (control limits 21%-55%). We observed some variation in our duration data, but no special cause variation was identified.
There were 27 (1.3%) total return visits to the UCCs for SSTIs over our study period. Of these, only 13 (0.6%) visits resulted in a change in antibiotics, most commonly with the addition of methicillin-resistant S aureus coverage (eg, switch from cephalexin to clindamycin for cellulitis).
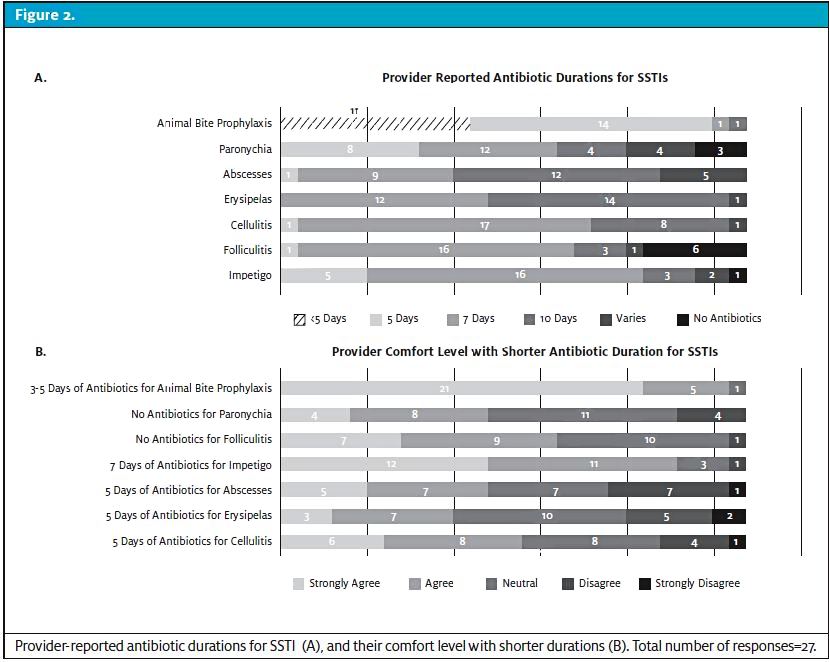
The survey was sent to 50 UCC providers, with 27 responding (54% response rate). Providers’ reported duration of antibiotic therapy for common SSTI and their comfort level with short durations are included in Figure 2. Only five (19%), seven (26%), and eight (29%) providers expressed being uncomfortable with a 5-day treatment course for cellulitis, erysipelas, and abscesses, respectively. Free text responses for barriers for shorter treatment courses included the following: four (15%) providers expressed most comfort with their accustomed antibiotic duration, two (7%) were concerned about treatment failures, two (7%) were concerned about parental pressure, and two (7%) were concerned about the development of acute rheumatic fever with shorter antibiotic courses.
DISCUSSION
At our pediatric UCCs, 40% of patients received inappropriately prolonged courses of oral antibiotics for SSTIs, placing them at risk for adverse drug events, development of multi-drug-resistant organisms, and increased healthcare costs.1
This is not unique to our institution; in fact, a broad evaluation of provider prescribing practices across the United States revealed that approximately 93% of pediatric patients receive >5 days of antibiotics for cellulitis.2 Other pediatric institutions have reported rates of more than 75% of antibiotic prescriptions with prolonged duration for SSTIs.12
Antimicrobial stewardship (AS) interventions have been shown to improve clinician antibiotic choice, dosing, and duration for respiratory diagnoses such as acute otitis media, upper respiratory tract infections, and pharyngitis;13 however, studies evaluating the effect of AS interventions on the treatment of SSTIs in pediatrics are not widely available. Schuler, et al were able to use QI methodology to improve the percentages of patients with SSTIs discharged from the inpatient setting with short courses of antibiotics from 23% to 74%,12 however there are no studies evaluating QI improvements in the ambulatory setting.
Our provider survey revealed interesting influences on selected antibiotic duration, such as parental pressure and fear of complications including perceived risk of rheumatic fever development.
Parental pressure is a frequently reported factor influencing clinician prescription decisions as seen in a 2015 systematic review.14 Specific provider concerns regarding parental pressure included fear of the potential for litigation, repeated visits, late night calls, desire for increased patient satisfaction, and avoidance of anxious and angry parents.14
The specific concern regarding the development of acute rheumatic fever in relation to Group A Streptococcus skin infections is largely unfounded as in developed countries this is a very rare phenomenon with only two cases reported in the literature.15 In addition, initial studies regarding prevention of acute rheumatic fever occurred in epidemic settings where the incidence of the disease was higher than it currently is in the United States.16 This suggests that provider education can be an important aspect of AS interventions.
LIMITATIONS
Our study has limitations. First, encounters were restricted to UCCs of a single pediatric institution so results may not be generalizable to other locations. Second, we did not include virtual encounters, which have risen in utilization since the COVID-19 pandemic. Third, given its retrospective nature, accuracy of data relies on correct chart documentation. Additionally, our survey included a small number of providers and may not be reflective of all providers’ prescribing behaviors or influences.
CONCLUSION
Overall, our study illustrates the need for AS interventions aimed at improving antibiotic durations for pediatric SSTIs in the urgent acre setting. While we did see some variation in our numbers over the year of analysis, there is still opportunity for improvement in decreasing the duration of antibiotics. Based on these findings, we are embarking on a QI project to increase the percentage of patients receiving 5-7 days of oral antibiotics for SSTIs in our pediatric UCCs by addressing the specific barriers we identified via our provider survey.
References
- Klepser ME, Dobson EL, Pogue JM, et al. A call to action for outpatient antibiotic stewardship. J Am Pharm Assoc (2003). 2017;57:457-463.
- Yonts AB, Kronman MP, Hamdy RF. The Burden and Impact of Antibiotic Prescribing in Ambulatory Pediatrics. Curr Probl Pediatr Adolesc Health Care. 2018;48:272-288.
- King LM, Hersh AL, Hicks LA, Fleming-Dutra KE. Duration of Outpatient Antibiotic Therapy for Common Outpatient Infections, 2017. Clin Infect Dis. 2021;72:e663-e666.
- Gerber JS, Jackson MA, Tamma PD, Zaoutis TE, Diseases AAPCoI, Pediatric Infectious Diseases S. Policy Statement: Antibiotic Stewardship in Pediatrics. J Pediatric Infect Dis Soc. 2021;10:641-649.
- Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164:1669-1674.
- Holmes L, Ma C, Qiao H, et al. Trimethoprim-Sulfamethoxazole Therapy Reduces Failure and Recurrence in Methicillin-Resistant Staphylococcus aureus Skin Abscesses after Surgical Drainage. J Pediatr. 2016;169:128-134 e121.
- Daum RS, Miller LG, Immergluck L, et al. A Placebo-Controlled Trial of Antibiotics for Smaller Skin Abscesses. N Engl J Med. 2017;376:2545-2555.
- Talan DA, Mower WR, Krishnadasan A, et al. Trimethoprim-Sulfamethoxazole versus Placebo for Uncomplicated Skin Abscess. N Engl J Med. 2016;374:823-832.
- Jaggi P, Wang L, Gleeson S, Moore-Clingenpeel M, Watson JR. Outpatient antimicrobial stewardship targets for treatment of skin and soft-tissue infections. Infect Control Hosp Epidemiol. 2018;39:936-940.
- Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis. 2014;59:e10-52.
- El Feghaly RE, Burns A, Goldman JL, Myers A, Purandare AV, Lee BR. Novel outpatient antibiotic prescribing report of respiratory infections in a pediatric health system’s emergency departments and urgent care clinics. Am J Infect Control. 2021;49:398-400.
- Schuler CL, Courter JD, Conneely SE, et al. Decreasing Duration of Antibiotic Prescribing for Uncomplicated Skin and Soft Tissue Infections. Pediatrics. 2016;137:e20151223.
- Gerber JS, Prasad PA, Fiks AG, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians: a randomized trial. JAMA. 2013;309:2345-2352.
- Lucas PJ, Cabral C, Hay AD, Horwood J. A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scand J Prim Health Care. 2015;33:11-20.
- O’Sullivan L, Moreland NJ, Webb RH, Upton A, Wilson NJ. Acute Rheumatic Fever After Group A Streptococcus Pyoderma and Group G Streptococcus Pharyngitis. Pediatr Infect Dis J. 2017;36:692-694.
- McMurray K, Garber M. Taking Chances With Strep Throat. Hosp Pediatr. 2015;5:552-554.
Manuscript submitted April 4, 2022; accepted July 18, 2022.
Author affiliations: Megan Hamner, MD, Pediatrics, Children’s Mercy Kansas City. Amanda Nedved, MD, Pediatrics, Children’s Mercy Kansas City; University of Missouri Kansas City. Holly Austin, MD,Pediatrics, Children’s Mercy Kansas City; University of Missouri Kansas City. Donna Wyly, RN, MSN, CPNP-AC, PPCNP-BC, Pediatrics, Children’s Mercy Kansas City. Alaina Burns, PharmD, BCPPS,Pharmacy, Children’s Mercy Kansas City; University of Missouri Kansas City. Brian Lee, PhD, MPH, Health Services and Outcomes Research, Children’s Mercy Kansas City; University of Missouri Kansas City, Rana E. El Feghaly MD, MSCI, Pediatrics, Children’s Mercy Kansas City; University of Missouri Kansas City. The authors have no relevant financial relationships with any commercial interests.
Appendix 1. ICD-10 Codes Utilized to Capture Patients with a Final Diagnosis of SSTIs
L08.9- Local infection of the skin and subcutaneous tissue, unspecified
L03.90- Cellulitis, unspecified
L03.319- Cellulitis of trunk
L03.113- Cellulitis of right upper limb
L03.114- Cellulitis of left upper limb
L03.115- Cellulitis of right lower limb
L03.116- Cellulitis of left lower limb
L03.317- Cellulitis of buttock
L02.91- Cutaneous abscess, unspecified
L02.419- Cutaneous abscess of limb, unspecified
L02.415- Cutaneous abscess of right lower limb
L02.416- Cutaneous abscess of left lower limb
L02.413- Cutaneous abscess of right upper limb
L02.414- Cutaneous abscess of left upper limb
L02.214- Cutaneous abscess of groin
L02. 215- Cutaneous abscess of perineum
L02.219- Cutaneous abscess of trunk, unspecified
L02.31- Cutaneous abscess of buttock
L01.00- Impetigo, unspecified
L01.03- Bullous impetigo
L01.01- Non-bullous impetigo
L73.9- Follicular disorder, unspecified
L02.12- Folliculitis/Furuncle of neck
L02.22- Folliculitis/Furuncle of trunk
L02.42- Folliculitis/Furuncle of limb
L02.32- Folliculitis/Furuncle of buttock
L03.0- Cellulitis and acute lymphangitis of finger and toe/paronychia
L03.031- Cellulitis of right toe
L03.032- Cellulitis of left toe
L03.011- Cellulitis of right finger
L03.012- Cellulitis of left finger
L03.019- Cellulitis of unspecified finger
L03.039- Cellulitis of unspecified toe
A46- Erysipelas
S061.459A- Open bite of unspecified hand, initial encounter
S71.159A- Open bite, unspecified thigh, initial encounter
S51.859A- Open bite of unspecified forearm, initial encounter
S91.059A- Open bite, unspecified ankle, initial encounter
S01.95XA- Open bite of unspecified part of head, initial encounter
S61.451A- Open bite of right hand, initial encounter
S61.452A- Open bite of left hand, initial encounter
S51.851A- Open bite of right forearm, initial encounter
S51.852A- Open bite of left forearm, initial encounter
S81. 859A- Open bite, unspecified lower leg, initial encounter
S91.051A- Open bite, right ankle, initial encounter
S91.052A- Open bite, left ankle, initial encounter
S81.851A- Open bite, right lower leg, initial encounter
S81.852A- Open bite, left lower leg, initial encounter
W50.3XXA- Accidental bite by another person, initial encounter
S60.479A- Other superficial bite of unspecified finger, initial encounter
Appendix 2
Confidential
Page 1 Pre-Intervention UC Provider Survey
Please complete the survey below. Thank you!
1. What is your degree designation? MD/DO
APRN
Other
2. How many years have you been in practice? < 5
5-10
10-15
>15
3. At what UCC location(s) do you primarily work? Blue Valley Urgent Care
East Urgent Care
North Urgent Care
(Please check all locations you work at)
4. Have you practiced in a private setting? Yes, currently
Yes, in the past
No
5. How often do you work in the urgent care? Multiple shifts per week
Once a week
2-3 times per month
Once a month
Once every few months
Very comfortable Comfortable Neutral Uncomfortable Very
uncomfortable
6. How comfortable are you with
diagnosing skin and soft tissue
infections?
If you selected uncomfortable or very uncomfortable,
please explain why __________________________________
Very comfortable Comfortable Neutral Uncomfortable Very
uncomfortable
7. How comfortable are you with
treating skin and soft tissue
infections?
If you selected uncomfortable or very uncomfortable,
please explain why __________________________________
8. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for impetigo? 5 days
7 days
10 days
Varies
No antibiotics
07/17/2020 4:16pm projectredcap.org
Confidential
Page 2
If varies, please explain why
__________________________________________
9. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for folliculitis? 5 days
7 days
10 days
Varies
No antibiotics
If varies, please explain why
__________________________________________
10. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for cellulitis? 5 days
7 days
10 days
Varies
No antibiotics
If varies, please explain why
__________________________________________
11. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for erysipelas? 5 days
7 days
10 days
Varies
No antibiotics
If varies, please explain why
__________________________________________
12. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for abscesses? 5 days
7 days
10 days
Varies
No antibiotics
If varies, please explain why
__________________________________________
13. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for paronychia? 5 days
7 days
10 days
Varies
No antibiotics
If varies, please explain why
__________________________________________
07/17/2020 4:16pm projectredcap.org
14. What is the oral antibiotic duration you most Less than 5 days
commonly prescribe for animal bite prophylaxis? 5 days
7 days
10 days
Varies
No antibiotics
If varies, please explain why
__________________________________________
15. Are there any factors that would prompt you to
prescribe a longer duration for a patient? If yes,
please explain __________________________________________
Please consider the following statements and select your answer based on how strongly you
agree or disagree with the statement
Strongly agree Agree Neutral Disgree Strongly
disagree
16. I would feel comfortable with
prescribing only 5 days of
antibiotics for cellulitis
If you selected disagree or strongly disagree, please
explain why
__________________________________________
Strongly agree Agree Neutral Disgree Strongly
disagree
17. I would feel comfortable with
prescribing only 5 days of
antibiotics for erysipelas
If you selected disagree or strongly disagree, please
explain why
__________________________________________
Strongly agree Agree Neutral Disgree Strongly
disagree
18. I would feel comfortable with
prescribing only 5 days of
antibiotics for abscesses
If you selected disagree or strongly disagree, please
explain why
__________________________________________
Strongly agree Agree Neutral Disagree Strongly
19. I would feel comfortable with disagree
prescribing only 7 days of
antibiotics for impetigo
If you selected disagree or strongly disagree, please
explain why
__________________________________________
Strongly agree Agree Neutral Disagree Strongly
disagree
20. I would feel comfortable with
not prescribing antibiotics for
folliculitis
If you selected disagree or strongly disagree, please
explain why
__________________________________________
Strongly agree Agree Neutral Disagree Strongly
disagree
21. I would feel comfortable with
not prescribing antibiotics for
paronychia
If you selected disagree or strongly disagree, please
explain why
__________________________________________
Strongly agree Agree Neutral Disagree Strongly
disagree
22. I would feel comfortable with
prescribing only 3-5 days of
antibiotics for animal bite
prophylaxis
If you selected disagree or strongly disagree, please
explain why
__________________________________________

