Published on
Urgent message: Whether required due to a crushing blow or close contact with a sharp surface, proper initial care for fingertip and nailbed injuries is essential to good outcomes and can often be administered in the urgent care setting.
Scott M. Zimmer, MD
Fingertip injuries are one of the most common conditions seen in urgent care and emergency room settings. From door crush to table saw injuries, the proper initial care is vital in the long-term result.
The goal is a fingertip that has minimal pain, good sensation, and adequate soft tissue coverage. Treatments range from simple cleansing with healing by secondary intention to bone-shortening
and primary closure.
The goals of this article will be to foster understanding of fingertip and nailbed anatomy, common injury patterns, and proper initial care.
Anatomy
A simple understanding of the anatomy is necessary for proper initial treatment. In addition, it allows the urgent care physician to convey the nature and severity of the injury to the hand specialist. This communication is key to long-term success because, often, the urgent care physician will simply need to provide wound care and proper follow- up.
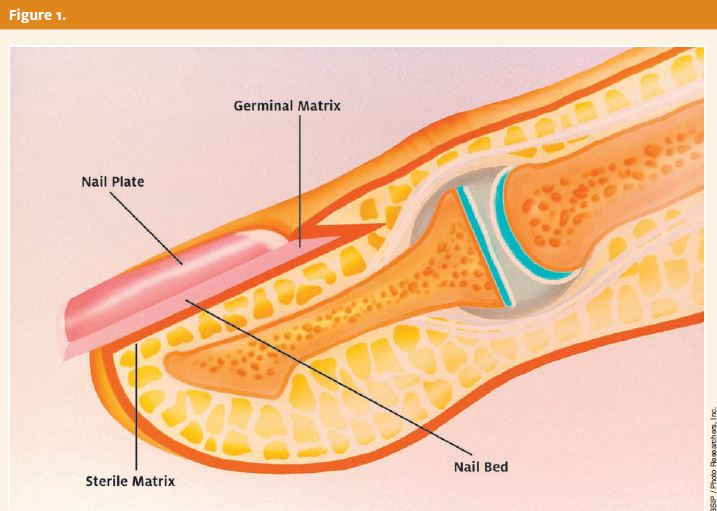
The pulp at the end of a digit is highly specialized tissue and consists of fibrous and fatty tissue that has septa extending from the skin to the distal phalanx. The nail unit is made up of the nail plate and the nailbed (Figure 1). Beneath the nail iplate, the nail bed is divided into the sterile matrix and the germinal matrix. The germinal matrix is the proximal region of the matrix demarcated by the crescent-shaped region seen at the nail base called the lunula. The germinal matrix produces over 90% of the nail but does not adhere to the nail plate.
The sterile matrix is distal to the lunula and is responsible for nail adherence. An important anatomical relation is the nail plate’s relation to the dorsal and ventral nail fold. Common injuries involve nail plate avulsion from this location. A mistake can be made by suturing the nail plate in place without replacing it in this anatomic location, causing pain and deformity with subsequent nail growth.
The terms hyponychium, paronychium, and eponychium refer to the regions of skin distal, on either side, and proximal to the matrix, respectively. A short course of cephalexin or clindamycin is appropriate. However, detailed discussion of this recommendation is beyond the scope of this article.
This type of initial treatment is effective even in severe fingertip injuries, as long as follow-up to a hand specialist is arranged within a few days.
The remaining sections of this article will detail treatment for various fingertip and nailbed injuries.
Nailbed Injuries
Controversy exists as to what constitutes a significant subungual hematoma. Traditional teaching states that a 50% or greater subungual hematoma warrants nail plate removal and inspection and possible matrix repair. A 1999 study3 revealed similar outcomes in children treated with and without nail plate removal and matrix repair regardless of the presence of fracture, size of subungual hematoma, or injury mechanism. In these patients, the nail plate was intact.
A lacerated nail plate almost always signifies a nail matrix laceration and the nail plate must be removed and the matrix repaired with 6-O absorbable suture. A simple soak, dressing, and antibiotic with a timely referral to a hand specialist is needed unless the physician has experience with this type of repair.
Subungual hematoma release is indicated for a significant hematoma greater than 25% to 50% that is associated with pain. No study has demonstrated a better outcome after evacuation (nail trephination), but it does decrease pain. This is performed by a twisting motion with an 11 blade scalpel or an 18 gauge needle piercing the nail plate over the hematoma.
Nailbed injuries with an associated displaced fracture represent a more difficult challenge. In the acute setting, simple care as described above still is sufficient if a quick referral is obtained, but digital block and fracture reduction with or without nailbed repair may be performed.
Initial Evaluation
Most fingertip injuries occur in children and young adults, which can make initial evaluation difficult.1 The history allows the physician to determine the forces involved and the degree of contamination. Young children with near amputations of the pulp with a small amount of nail should be considered for simple reattachment, since many times the nail acts as a composite graft and gives a desirable result.
Radiographs allow the determination of fracture, which often suggests a nail matrix laceration even if the nail plate is intact.
Digital block is often necessary to properly evaluate and cleanse the wound. Various techniques for the block have been described, but all can be a challenge in the young patient. One technique described by Chiu2 al- lows one injection into the flexor sheath as if giving a trigger injection and uses much less volume of anesthetic than circumferentially infiltrating the digit. A simple soak in a sterile normal saline and 4% povidone iodine or chlorhexidine bath (dilution at least 5:1) is an effective cleansing treatment and is often followed sim- ply by a non-adherent dressing of bacitracin, petroleum gauze, and 2x2s.
The nail plate is the best structure to place back over the matrix after repair, and even after partial avulsion. It has the best contour and often does not even need to be sutured in place. A new nail will begin to grow and push the replaced nail out in a few weeks.
The physician does not need to replace the nail plate if the dorsal and ventral nail fold region is not damaged. If the physician does not feel comfortable replacing the nail plate, then a simple dressing with abundant bacitracin/Neosporin will suffice. The matrix will dry out after a few days and become non-tender. It is better to leave the nail plate off if there is a laceration of the matrix and the physician is referring it for repair.
It is also important for the physician to align lacerations of the eponychium, hyponychium, and paronychium. These can be repaired with 4-O or 5-O nylon or Prolene and is necessary to guide the new growing nail in proper alignment.
One practical point is the technique for nail plate removal. Avoid using sharp scissors, as this may damage the matrix. A mosquito hemostat or a freer-elevator works well to slide under the nail plate and lift it off the matrix with minimal damage. The ability to remove the nail plate quickly with minimal trauma is needed not only in injury, but is necessary in acute paronychial infections where the region needs to be decompressed.
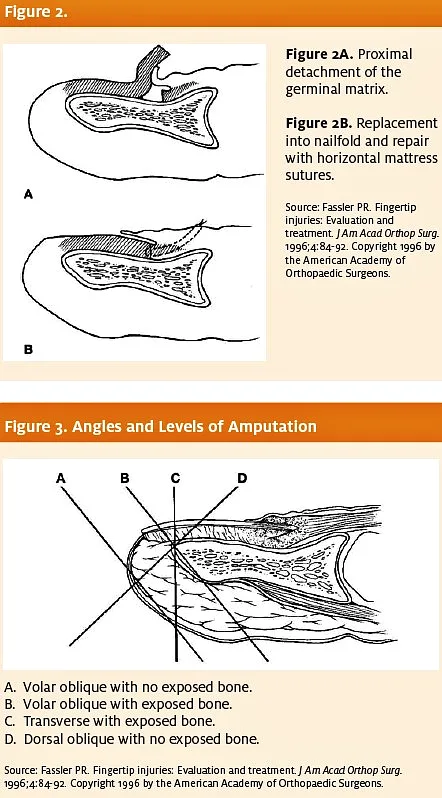
The germinal matrix may also become avulsed from its base and flip out in front of the eponychium (Figure 2). It is important to recognize this occurrence and re- place it in its anatomic location. Again, the key is recognition of different patterns of in- jury and the ability to convey the nature of the injury to a hand specialist.
Fingertip Amputations
Amputations can range from small pulp injuries to total amputation of the finger through the nail. In the majority of cases, the small amputated remnant is not able to be replanted. An exception is a small child in which case the tip can simply be sutured back in place if there is no significant contamination or tip destruction.
In any adult or child, if there is any skin bridge connecting the amputated part, simple suture closure may lead to unexpectedly excellent results. This treatment is certainly acceptable in an acute setting, especially if it is the nailbed that is still connected since this is a highly vascular structure.
Treatment of any amputation begins with determining the level of amputation and its obliquity (Figure 3).
A main determinant is the amount of exposed bone. A misconception is that no exposed bone is allowed and that the bone must be shortened at the initial evaluation. Fingertip amputations with a small amount of exposed bone can be treated open by healing with secondary intention, with excellent results.4-8 In the urgent care or emergency room setting, the physician does not need to feel that he or she must shorten the bone and get primary closure. Appropriate care would consist, again, of soak, bacitracin/
Neosporin, and dressing with referral in two to three days. Figure 4 demonstrates an amputation of the nail plate and nailbed with a small amount of exposed bone five days after injury. The wound will be allowed to simply heal in by secondary intention with daily dressing changes.
An important point to understand is the role of the distal phalanx in supporting the nailbed. If there is no bone supporting the nail matrix, then the nail will “hook” over the end of the digit. Bone should only be trimmed back to the edge of the nail matrix to prevent this deformity.
The decision to perform an immediate revision amputation in the urgent care or emergency department setting is discouraged unless the physician has considerable training in this area. In many rural settings, there may be a need to perform this procedure acutely, but several key points need to be addressed. An amputation just distal to the distal interphalangeal joint will be used as an example.
A common mistake would be to trim back the bone far enough to get closure. Two important factors must be considered. First, the closer one gets to the joint, the greater the chance that the distal insertions of the extensor and flexor tendons may be disrupted. If only a small amount of distal phalanx is left, then removal of this small remaining fragment may be best. The flexor and extensor tendons should never be repaired to the ends of the bone because this will alter function at the metacarpophalangeal and proximal interphalangeal joints. Simply pull on the tendon and cut it, then allow it to retract into the wound.
The more common problem seen is that a good portion of the germinal matrix is left at the nail base. The nail must be completely ablated by excising the entire matrix prior to end closure. If the matrix is left, a painful nail cyst will develop. Care must be taken not to release the terminal extensor tendon when excising the matrix.

Summary
Fingertip and nailbed injuries are among the most common injuries seen in urgent care and emergency department settings. The following summary points may serve as guidelines in directing care in the acute setting:
- Initial evaluation with radiographs and exam will allow the physician to determine appropriate care and convey the injury to the hand
- Acute cleansing for all fingertip injuries can be a soak of diluted 4% povidone iodine/chlorhexidine and saline solution, followed by bacitracin/Neosporin nonadherent dressing with splint or bulky
- A three-day course of cephalexin or clindamycin is
- The majority of partial amputations can heal by secondary
- A nail plate laceration is indicative of a matrix injury, and repair is
- Definitive treatment is rarely needed in the urgent care setting, and quick referral within three days is usually acceptable. This will be dependent on the practices and expectations of the local hand surgeon.
References and Suggested Reading
- Zook EG, Guy RJ, Russell. A study of nail bed injuries: causes, treatment, and prognosis. J Hand Surg. 1984;9A:247-252.
- Chiu Transthecal digital block: Flexor tendon sheath used for anesthetic injection. J Hand Surg. 1990;15:471.
- Roser SE, Gellman Comparison of nail bed repair versus nail trephination for subungual hematomas in children. J Hand Surg. 1999;24A(6):1166-1170.
- Mennen U, Wiese Fingertip injuries management with semi-occlusive dressing. J Hand Surg. 1993;18(B):416-422.
- Williamson DM, Sherman KP, Shakespeare The use of semi-permeable dressings in fingertip injuries. J Hand Surg. 1987;12(B):125-126.
- Buckley SC, Scott S, Das Late review of the use of silver sulfadiazine dressings for the treatment of fingertip injuries. Injury. 2000;31:301-304.
- Ipsen T, Frandsen PA, Barfred Conservative treatment of fingertip injuries. Injury. 1987;18:203-205.
- Lamon RP, Cicero JJ, Frascone RJ, et Open treatment of fingertip amputations. Ann Emerg Med. 1983;12:358-360.
- Berger RA, Weiss Hand Surgery. Philadelphia, PA: Lippincott, Williams, and Wilkins, 2004:1101-1118.
- Fassler Fingertip injuries: Evaluation and treatment. J Am Acad Ortho Surg. 1996;4(2):84-92. Figures 4 and 5.

