Published on
Urgent message: The second part in a two-part series offers expert guidance on short and long-term management of the disease in the urgent care setting through the use of pharmacotherapy, protocols for treatment, and a written asthma action plan at discharge.
BRADLEY M. TURNER MD, MPH, MHA, FCAP, FASCP and JANET M. WILLIAMS, MD, FACEP
Introduction
Once the suspicion of an asthma exacerbation exists, short term management is focused on reducing the severity of the exacerbation, with the hopes of discharging the patient home for outpatient follow-up. This can be achieved through pharmacotherapy that reduces inflammation and relaxes the airway musculature, in hopes of reversing airflow obstruction. Long-term management is focused on prevention of future exacerbations through pharmacotherapy and education at discharge. Understanding the rationale behind short and long-term management of a suspected asthma exacerbation will lead to more efficient assessment and effective discharge of patients presenting to an urgent care center.
Pharmacotherapy
Pharmacotherapy for asthma generally can be divided into quick-relief short-term medications (short-acting beta2 agonists [SABAs], anticholinergics, and oral/systemic corticosteroids), and long-term controller medications (inhaled corticosteroids, long-acting B2 agonists [LABAs], leukotriene antagonists, and immunomodulators). Complementary and alternative medications (CAM) comprise another fast-growing subset of pharmacotherapy (acupuncture, chiropractic therapy, homeopathic and herbal medicine, breathing and relaxation techniques, and yoga). In the urgent care setting, quick relief medications are the mainstay of treatment.
Although this review focuses on several forms of specific quick-relief, short-term pharmacotherapy (Table 1), urgent care providers should be familiar with the various other treatment options, their appropriate use, and possible misuse. For example, a patient whose history suggests a severity classification of persistent asthma should be on an inhaled corticosteroid (unless contraindicated).1 A second example is the misconception patients often have (personal experience) about the use of LABAs during acute exacerbations. LABAs are not recommended in acute asthma exacerbations.1 Patients, however, may not be aware of that fact, and may attempt to use long-term controller medication for acute relief. Familiarity with these and other facts about the various long-term controller medications and CAM will facilitate more efficient assessment of the severity and control of a patient’s asthma, and help to create a more effective discharge plan. A patient who is noncompliant with medications or not on appropriate therapy is at increased risk of recurrent exacerbations and increased morbidity. A nice overview of long-term controller and CAM options can be found in the EPR-3 report (pages 216-235;242).
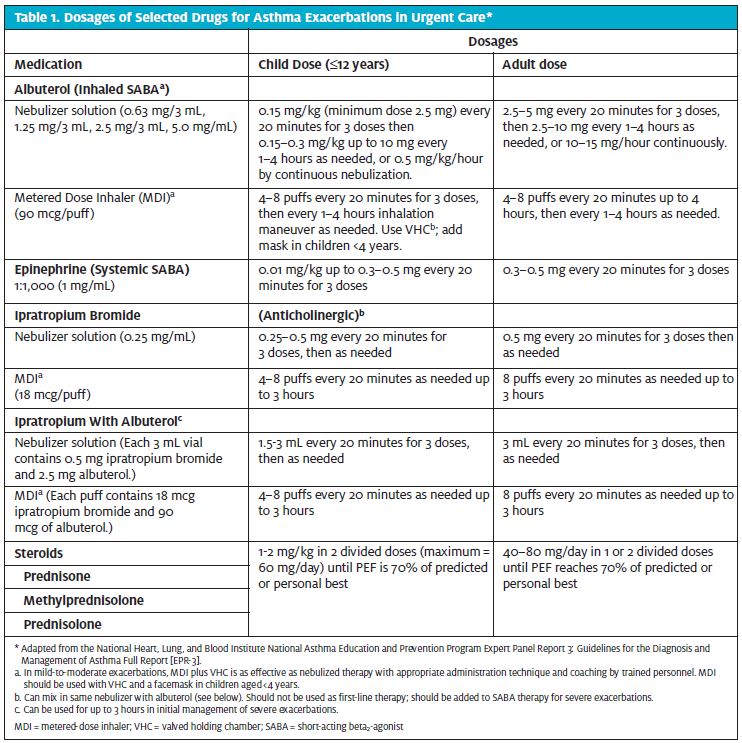
SABAs are the most effective asthma therapy for rapid relief of symptoms and reversal of airflow obstruction.1,2 The EPR-3 recommends using SABAs only when necessary for symptom relief (i.e they should not be used on a continuous daily basis), or before anticipated exposure to known asthma triggers. SABAs should be used in all patients with asthma exacerbation (unless contraindicated). The dosage and delivery mechanism will be dependent on the severity of the presentation (Table 1). Anticholinergics are not recommended as monotherapy for quick relief of asthma symptoms.1,2 They can be used in combination with SABAs in severe presentations. The use of steroids should be oral rather than intravenous (IV) in the urgent care setting unless a patient is unable to take oral medications, or is approaching impending respiratory failure. Oral administration of prednisone has been shown to have effects equivalent to those of IV methylprednisolone, and in the opinion of the EPR-3 expert panel, is usually preferred because it is less invasive. There is no known advantage for higher doses of corticosteroids in severe asthma exacerbations. The total course of systemic corticosteroids for an asthma exacerbation requiring an urgent care visit may last from 3 to 10 days. For corticosteroid courses of less than 1 week, there is no need to taper the dose. For slightly longer courses (e.g., up to 10 days), a taper can be considered; however, there probably is no need to taper, especially if patients are concurrently taking inhaled corticosteroids.
Management of asthma exacerbations in the ambulatory/urgent care setting
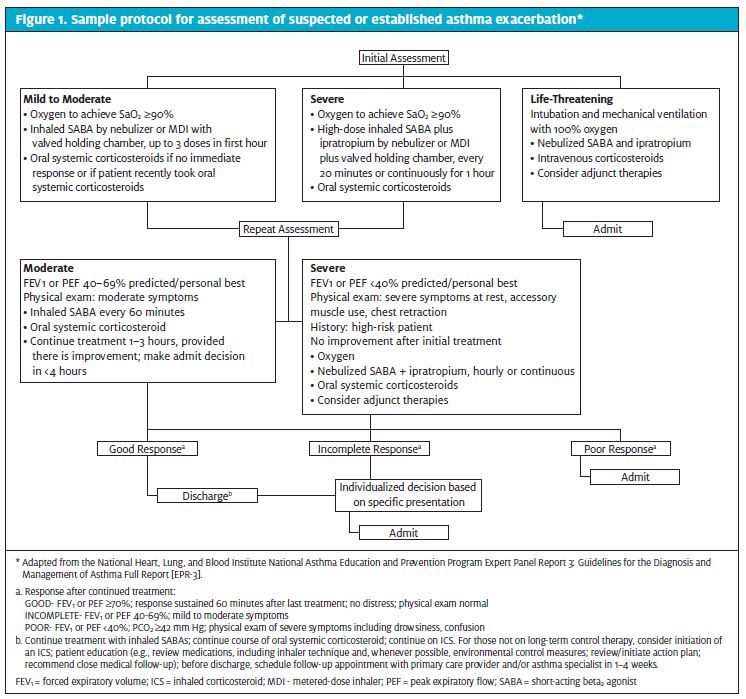
Establishing protocols for treatment based on current management guidelines can facilitate improved care of patients with asthma.1,3 A sample protocol is given in Figure 1. First-line treatment of suspected or diagnosed asthma exacerbations includes SABAs for all patients and oxygen, if necessary. Continuous administration of SABAs is the most effective means of reversing airflow obstruction.1 The onset of action for SABAs is less than 5 minutes and repetitive administration produces incremental bronchodilation. Most patients will have a significant response after the first dose. It is recommended that patients who have a rapid response be observed for 30 to 60 minutes after the most recent dose of bronchodilator to ensure stability of the response before discharge to home.1 After initial administration, the frequency of administration should be judged based on improvement in airflow obstruction, improvement of presenting signs and symptoms, and the occurrence of any side effects. Nebulizer therapy may be preferred for patients who are unable to cooperate effectively in using a metered-dose inhaler. Adding ipratropium bromide to a selective SABA produces additional bronchodilation, resulting in fewer hospital admissions, particularly in patients who have severe airflow obstruction.1 Administer supplemental oxygen to maintain an SaO2 >90%.
Monitor SaO2 until a clear response to bronchodilator therapy has occurred. In patients who have not responded completely to initial SABA, systemic corticosteroids are recommended. These medications speed the resolution of airflow obstruction and reduce the rate of relapse and may reduce hospitalizations. 1 A short course (5-10 days) of oral corticosteroids should be given at discharge. Theophylline is not recommended for treatment in the urgent care setting because it does not appear to provide additional benefit. Antibiotics are generally not recommended, except as needed for co-morbid conditions that would require antibiotics. Other therapies not generally recommended include aggressive hydration, chest physical therapy, mucolytics, and sedation. In particular, anxiolytic and hypnotic drugs are contraindicated in severely ill asthma patients because of their respiratory depressant effect.
| Table 2. Risk Factors for Death From Asthma* |
Asthma history
|
Social history
|
Comorbidities
|
Other
|
| * Adapted from the National Heart, Lung, and Blood Institute National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Full Report [EPR-3]. |
Discharge
The response to initial treatment is a better predictor of the need for hospitalization than the severity of an exacerbation on presentation.4-13 Therefore repeat assessment should be the primary factor in the decision to discharge the patient home, versus admit to the hospital. In general, discharge is appropriate if forced expiratory volume (FEV1) or peak expiratory flow (PEF) has returned to 70% of predicted or personal best and symptoms are minimal or absent. Patients who have an incomplete response to therapy (FEV1 or PEF 50% to 69% of predicted or personal best) and with mild symptoms should be assessed individually for their suitability for discharge home, with consideration given to factors listed in Table 2 and Figure 1. Hospital admission is warranted if an incomplete or poor response persists. At discharge sufficient medications should be given for a patient to continue on the prescribed treatment until follow-up. Follow-up should be to either to the patient’s primary care provider or an asthma specialist. If an appointment can be scheduled prior to discharge, the likelihood that a patient will actually receive an appointment and follow up increases.14,15 A written discharge plan should be reviewed with a patient, including review of discharge medications and patient education on the correct use of an inhaler. Discharge is also an opportunity to inform or reinforce the signs of an asthma exacerbation, because studies show that some patients are unable to perceive signs of deterioration that would indicate a need to increase medication.16,17 This can be done through a written asthma action plan. Although the scientific evidence on written asthma treatment plans is inconclusive, studies do suggest that use of written plans may help patients improve control of their asthma, particularly with respect to prevention and management of asthma exacerbations, and they are recommended by the EPR-3.1,2 A written asthma action plan includes two important elements: daily management of medications and environmental triggers information on how to recognize (i.e. signs and symptoms) and handle (i.e. medications, emergency contacts) worsening asthma.
A very nice example of a written asthma action plan for an adult and child can be found in the EPR-3 report (page 117-119).1 A written asthma action plan is the most appropriate method to provide concise instructions on managing asthma symptoms in the ambulatory care setting.1,2
Conclusion
In a previous issue (Part 1), we discussed the pathogenesis of airway inflammation in asthma, key indicators for a diagnosis of asthma on history and examination, and key risk factors suggesting worse outcomes in patients with asthma exacerbations. In Part 2, we reviewed the short and longer-term management of these patients through the use of pharmacotherapy, protocols for treatment, and a written asthma action plan at discharge.
As we enter an era of health care in which decisions about treatment are increasingly patient-driven, urgent care centers will become a first choice for many patients seeking health care advice. The prevalence of asthma is increasing, and current trends suggest that an increasing number of patients with acute asthma exacerbations will present to urgent care centers for treatment. Understanding the underlying pathogenesis of asthma will help the urgent care provider in doing an adequate medical history and examination in order to elicit risk factors associated with worse outcomes. Understanding the various pharmacotherapy and treatment options, and the development of protocols for short-term management of asthma, will improve the efficiency and efficacy of treatment for asthma exacerbations in the urgent care setting. A written asthma action plan can contribute to improved long-term control of asthma through prevention and management of asthma exacerbations, leading to decreased health care costs and improved long-term outcomes.
References
- US Department of Health and Human Services, National Institutes of Health, National Heart Lung and Blood Institute. National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma; 2007: 1-417
- Myers T, Tamasio L. Asthma: 2015 and Beyond. Respiratory Care. 2011; 56(9):1389-1410.
- Self T, Usery J, Howard-Thompson A, Sands C. Asthma Treatment Protocols in the Emergency Department: Are they Effective? Journal of Asthma 2007; 44: 243-248.
- Cham GW, Tan WP, Earnest A, Soh CH. Clinical predictors of acute respiratory acidosis during exacerbation of asthma and chronic obstructive pulmonary disease. Eur J Emerg Med 2002; 9(3):225–32.
- Chey T, Jalaludin B, Hanson R, Leeder S. Validation of a predictive model for asthma admission in children: how accurate is it for predicting admissions? J Clin Epidemiol 1999; 52(12):1157–63.
- Gorelick MH, Stevens MW, Schultz TR, Scribano PV. Performance of a novel clinical score, the Pediatric Asthma Severity Score (PASS), in the evaluation of acute asthma. Acad Emerg Med 2004; 11(1):10–8.
- Karras DJ, Sammon ME, Terregino CA, Lopez BL, Griswold SK, Arnold GK. Clinically meaningful changes in quantitative measures of asthma severity. Acad Emerg Med 2000; 7(4):327–34.
- Kelly AM, Powell C, Kerr D. Patients with a longer duration of symptoms of acute asthma are more likely to require admission to hospital. Emerg Med (Fremantle ) 2002;14(2):142–5.
- Kelly AM, Kerr D, Powell C. Is severity assessment after one hour of treatment better for predicting the need for admission in acute asthma? Respir Med 2004; 98(8):777–81.
- McCarren M, Zalenski RJ, McDermott M, Kaur K. Predicting recovery from acute asthma in an emergency diagnostic and treatment unit. Acad Emerg Med 2000; 7(1):28–35.
- Rodrigo G, Rodrigo C. Assessment of the patient with acute asthma in the emergency department. A factor analytic study. Chest 1993; 104(5):1325–8.
- Rodrigo G, Rodrigo C. Early prediction of poor response in acute asthma patients in the emergency department. Chest 1998c; 114(4):1016–21.
- Smith SR, Baty JD, Hodge D III. Validation of the pulmonary score: an asthma severity score for children. Acad Emerg Med 2002; 9(2):99–104.
- Baren JM, Boudreaux ED, Brenner BE, Cydulka RK, Rowe BH, Clark S, Camargo CA Jr. Randomized controlled trial of emergency department interventions to improve primary care follow-up for patients with acute asthma. Chest 2006; 129(2):257–65.
- Zorc JJ, Scarfone RJ, Li Y, Hong T, Harmelin M, Grunstein L, Andre JB. Scheduled follow-up after a pediatric emergency department visit for asthma: a randomized trial. Pediatrics 2003;111(3):495–502.
- Hardie GE, Gold WM, Janson S, Carrieri-Kohlman V, Boushey HA. Understanding how asthmatics perceive symptom distress during a methacholine challenge. J Asthma 2002; 39(7):611–8.
- Kikuchi Y, Okabe S, Tamura G, Hida W, Homma M, Shirato K, Takishima T. Chemosensitivity and perception of dyspnea in patients with a history of near-fatal asthma. N Engl J Med 1994; 330(19):1329–34.

