Published on
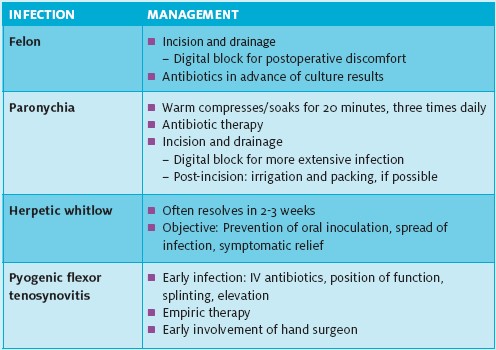
Urgent message: Common superficial hand infections may be managed easily by the urgent care physician. Left untreated or undertreated, however, simple hand infections may progress to disabling conditions requiring urgent sub-specialty management.
Arthur R. Smolensky, MD, Samuel M. Keim, MD, MS, and Peter Rosen, MD
The hand is an intricate and crucial feature of the human body. Yet, with the exception of superficial cellulitis, common hand infections require relatively simple surgical procedures—many of which can be performed in the urgent care setting.
Proper diagnosis and management is essential in preventing significant morbidity related to these infections. Many hand infections do well with early splinting, antibiotics, and pain control,
whereas more advanced infections require incision and drainage.
This article will focus on and distinguish among types of hand infections seen commonly in urgent care.
FELON
Pathophysiology
A felon is an infection of the pulp of the distal finger or thumb. It differs from other subcutaneous abscesses because of the presence of 15 to 20 septa that run along the long axis of the finger that divide the pulp into small superficial compartments.
Abscesses in these small noncompliant spaces can be extremely painful, and swelling in this area can lead to necrosis before any fluctuance can be observed.
Additionally, because the septa attach to the periosteum, spread of the infection can lead to osteomyelitis of the distal phalanx.1
The septa do, however, provide a barrier that protects the joint space and tendon sheath by limiting the proximal spread of the infection. The usual cause is penetrating trauma with secondary bacterial invasion.
Clinical Features
The most commonly affected digits are the thumb and index finger. Common predisposing causes include wood splinters, bits of glass, abrasions, and minor puncture wounds.
Staphylococcus aureus is the most common organism, but Streptococcus species, anaerobes, and gram-negative organisms are also encountered frequently. Therefore, one should always consider a polymicrobial etiology. A Gram’s stain and culture should be obtained, as these infections may be difficult to eradicate and chronic infections may be caused by atypical organisms.2
Clinically, a felon begins as an area of cellulitis and inflammation that progresses rapidly to throbbing, pain, swelling, and pressure in the distal pulp space.
It is important to not confuse a felon with a herpetic whitlow, as incision-and-drainage is not necessary in the latter and may cause additional morbidity. Clues are the presence of herpetic ulcers in the mouth or a past history of canker sores. The location of the infection is also helpful in making the distinction, since the herpetic lesion is usually paronychial rather than in the pulp space.
Management
Traditional management of felons emphasizes early incision and drainage. A common error is to await the appearance of fluctuance before initiating surgical incision. Since the fascial septa prevent fluctuance, this error can lead to necrosis of the distal digit.
Most felons can be drained by a single lateral incision.3 A digital block using a long-acting anesthetic such as 0.25% bupivacaine should be used because postoperative discomfort is considerable. The digital block anesthetizes the entire digit distal to the infiltration site, which is most often placed at the level of the metacarpal-phalangeal joint. In cross-section, the digital nerves lie approximately at 4 and 8 o’ clock. Slow infiltration of 1 ml to 2 ml of local anesthetic on each side of the digit at these locations will typically result in a good block. For thumbs, it is necessary to administer a third subcutaneous injection line across the dorsum of the digit at the same level. Avoid administering anesthetics containing epinephrine.
The incision should be made along the ulnar aspects of the second through fourth digits (index, long, and ring fingers) and the radial aspects of the first and fifth digits (thumb and little finger), avoiding the pincher (palmar) surfaces.
The incision should be made 0.5 cm distal to the DIP joint crease and dorsal to the neurovascular bundle of the fingertip, and go to the free edge of the nail.
Alternatively, a single volar longitudinal incision can be performed.4 The wound should be irrigated and, if possible, loosely packed with gauze. The packing should be removed in two to three days, and allowed to heal without secondary closure.
Most felons are also treated with antibiotics until culture results are obtained. Depending on the local prevalence of methicillin-resistant Staphylococcus aureus, appropriate antibiotics should be given for at least five days.
[Note: A future issue of JUCM will discuss MRSA in detail.]
Incision techniques not recommended include the “fish-mouth” incision, the “hockey stick” (or “J”) incision, and the transverse palmar incision. These incisions are more likely to result in painful, sensitive scars and damage to neurovascular structures.4
Bilateral incisions used to drain felons commonly leave unstable finger pads or may result in painful neuromas or aesthetic fingertips. “Fish-mouth” incisions may destroy blood supply to the fingertip.3 Longitudinal midline incisions on the volar surface may leave scars over an important area for sensation.
Any incision that is made too deeply and proximally can injure the flexor tendon sheath and initiate a tenosynovitis.
Felons not responding to treatments outlined above should be referred to a hand specialist for more definitive management and long-term follow-up.
PARONYCHIA
Pathophysiology
A paronychia is a localized superficial infection or abscess involving the lateral nail fold. Overall, it is the most common infection of the hand. Predisposing factors include overzealous manicuring, nail biting, diabetes mellitus, and occupations in which the hands are frequently immersed in water.5 Paronychia in children is often caused by finger sucking and nail biting.
Clinical Features
Swelling and tenderness of the soft tissue along one or both sides of the lateral nail fold are evident and easily recognized. A paronychia begins as cellulitis, but if untreated may progress to an abscess. S aureus is the most common cause of paronychia infection, followed by Streptococci.6
These infections, like all hand infections, may be polymicrobial. Atypical mycobacterium and Candida albicans should be considered as etiologic agents in chronic cases (Figure 1). Chronic cases are often seen in immunocompromised patients.

Management
Treatment for early acute paronychia infection without abscess formation includes warm compresses or soaks to the affected digit for 20 minutes, three times per day and antibiotic therapy.
Once the area becomes fluctuant, drainage is necessary and usually curative. Adequate drainage can often be obtained by elevating the skin off of the nail to allow the pus to drain. This can be performed without anesthesia in some patients.
More extensive infections require a digital block, as described previously. After softening the eponychium by soaking the affected finger in warm water, a scalpel or 18 gauge needle may be advanced parallel to the nail and under the eponychium at the site of maximal swelling.7 If the infection is more extensive, the lateral one-fourth of the nail may be bluntly dissected from the underlying nail bed and germinal matrix and the lateral nail plate.
After incision, the cavity should be irrigated and packing placed if possible. Unlike felon drainage, cultures and antibiotics are not indicated if the drainage is complete, and there is no evidence of cellulitis. Most paronychias resolve in five to 10 days, but all hand infection patients should be given disposition instructions that include follow-up evaluation.
A well-known complication of a paronychia infection is osteomyelitis of the distal phalanx. A patient with chronic paronychia should be referred to a dermatologist or hand surgeon.
HERPETIC WHITLOW
Pathophysiology
Herpetic whitlow is a self-limited herpes simplex (HSV) viral infection of the distal finger. In the United States, HSV infection of the hand occurs in 2.4 cases per 100,000 population per year.8 It is the most common viral infection of the hand.
Infections by HSV 1 or HSV 2 are clinically indistinguishable. Direct inoculation of the virus into a wound is usually the mechanism of infection.9
Herpetic whitlow is often found in adult women with genital herpes and children with coexistent herpetic gingivostomatitis.
Healthcare workers are also at an increased risk due to exposure to orotracheal secretions; however, a review of herpes infections in the hand shows only 14% of adult cases occur in healthcare workers. 8 The risk to healthcare workers is markedly reduced with compliant use of universal precautions.
Clinical Features
The infection usually involves a single finger that is painful, erythematous, and swollen. It is characterized by vesicles early in the disease process. After about two weeks, the vesicles coalesce, and the infection can look similar to common bacterial infections of the hand such as paronychia and felon.
The distinction can be made by taking a careful history, and asking about risk factors. On examination, tenderness is present, but is less severe than that found in bacterial infections.
The distinction is important to make because performing an incision and drainage on a herpetic whitlow can lead to secondary bacterial infection.
Management
The diagnosis of herpetic whitlow is usually made clinically based on the appearance of the lesion and history of recurrence or potential source of inoculation.
A vesicle can be unroofed, and the fluid used in one of two ways: to make a Tzank smear which may reveal multinucleated giant cells, or to obtain a viral culture.
Herpetic whitlow usually resolves spontaneously in two to three weeks.9 The main goals of treatment are to prevent both oral inoculation and spread of the infection, as well as to obtain symptomatic relief.
The involved digit should be kept covered with a dry dressing. Many recommend treatment with oral acyclovir (400 mg TID) for 10 days if the diagnosis is made within 48 hours of symptom onset, although the efficacy of this approach is unproven in controlled trials.10
Stronger evidence exists to recommend oral acyclovir for recurrent infections during the prodromal stage, as well as in immunocompromised patients.11 No convincing evidence exists to recommend topical acyclovir for whitlow treatment.
Patients should be advised that the infection recurs in 30% to 50% of cases, but the initial infection is typically the most severe.
TENDON SHEATH INFECTION (PYOGENIC FLEXOR TENOSYNOVITIS)
Pathophysiology
Acute tenosynovial space infections in the hand tend to involve the flexor tendon sheaths and the radial and ulnar bursa. The synovial sheaths are poorly vascularized, but are rich in nutritious synovial fluid. This combination provides an ideal environment for bacterial growth. Once inoculated, infection spreads rapidly through the sheath.
Infection of the flexor tendon sheath is known as pyogenic flexor tenosynovitis, and is a surgical emergency.
Clinical Features
In 1912, Kanavel described the four clinical features of this infection.12 They are:
- fusiform volar swelling along course of the tendon sheath
- swollen, red, and tender palmar surface
- fixed flexion
- passive DIP joint extension causing pain.
Patients will recall some distant traumatic event or a puncture wound typically on the palmar surface of the hand. The puncture likely occurs at a flexor crease because this is where the flexor tendon sheath is most superficial. Hematogenous spread can occur, but is rare.
Management
Early diagnosis is absolutely critical to reduce the amount of tendon damage, as well as to minimize any long-term sequelae (i.e., disability) that might arise from this infection.
One of the conditions that can mimic pyogenic flexor tenosynovitis is a subcutaneous abscess. An abscess should not have tenderness over the entire sheath, and passive DIP joint extension should not be painful in the uninvolved surfaces.13
Ultrasound examination may show an abnormal effusion or abscess in the tendon sheath.14 Plain radiographs should be ordered to look for possible foreign bodies. Early infections may respond to a combination of intravenous antibiotics, position-of-function splinting, and elevation; operative washout may not be required.
This should, however, be the decision of a subspecialist. Typical causative organisms include common skin flora such as Staphylococcus and Streptococcus. In immunocompromised patients, typical and atypical organisms such as Candida albicans and disseminated Neiserria gonorrhea, both of which have been reported as causes of pyogenic flexor tenosynovitis, should be suspected.15-17
Empiric therapy should be initiated in urgent care as soon as the presumptive diagnosis is made, and includes cefazolin or clindamycin. Alternatively, for immunocompromised patients or those where N gonorrhea is a concern, ampicillin/sulbactam or cefoxitin (or, if allergic to penicillin, clindamycin plus a fluoroquinolone or sulfamethoxazole and trimethoprim) should be started.
Tetanus prophylaxis should be administered if necessary. Further management should be decided upon with or by a hand surgeon. Early involvement of a hand surgeon can facilitate timely and efficient patient management.
18
The surgeon will decide if surgery is indicated, but it is essential that the urgent care clinician provide the information needed to ascertain whether immediate transfer is warranted. These discussions should be documented thoroughly for both optimal patient care, and to reduce medical malpractice liability.
Patients should always be educated regarding the serious potential nature of these infections and the crucial need to be compliant with after-care instructions. Systemically ill and immunocompromised patients should be evaluated the same day, as they are more prone to serious complications from this infection.
Summary
It is common for patients to present to urgent care with symptoms caused by hand infections. Correct identification of their origin followed by aggressive, timely, and appropriate management supports attainment of a good outcome.
References
1. Watson PA, Jebson PJ. The natural history of the neglected felon. Iowa Orthop J.1996;16:164-166.
2. Hausman MR, Lisser SP. Hand infections. Orthop Clin North Am. 1992;23:171-185.
3. Milford L. Infections of the hand. In: Crenshaw AH, ed. Campbell’s Operative Orthopaedics.8th ed. St. Louis, MO: Mosby; 1992.
4. Jebson PJ. Infections of the fingertip. Paronychias and felons. Hand Clin. 1998(14): 547-555.
5. Shroff P, Parikh DA, Fernandez RJ, et al. Clinical and mycological spectrum of cutaneouscandidiasis in Bombay. J Postgrad Med. 1990;(36):83-86.
6. Brook I. Paronychia: A mixed infection. Microbiology and management. J Hand Surg[Br]. 1993;18(3):358-389.
7. Blumstein H. Incision and drainage. In: Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 3rd ed. Philadelphia, PA: WB Saunders; 1998.
8. Gill MJ, Arlette J, Buchan KA. Herpes simplex virus infection of the hand. A profile of 79 cases. Am J Med. 1988;84(1):89-93.
9. Feder HJ, Long SS. Herpetic whitlow. Epidemiology, clinical characteristics, diagnosis,and treatment. Am J Dis Child. 1983;137:861-863.
10. Kesson A. Use of acyclovir in herpes simplex virus infections. J Paediatr Child Health.
1998;34(1):9-13.
11. Laskin O. Acyclovir and suppression of frequently recurring herpetic whitlow. Ann InternMed. 1985;102(4):494-495.
12. Kanavel M. Infections of the Hand. Philadelphia, PA: Lea and Febigel; 1912.
13. Stern P. Selected acute infections. Instr Course Lect. American Academy of OrthopaedicSurgeons. 1990;39:539-546.
14. Cardinal E, Bureau NJ, Aubin B, et al. Role of ultrasound in musculoskeletal infections.Radiol Clin North Am. 2001;39:191-201
15. Gunther SF, Gunther SB. Diabetic hand infections. Hand Clin. 1998;14(4):647-656.
16. Townsend DJ, Singer DI, Doyle JR. Candida tenosynovitis in an AIDS patient: A case report.J Hand Surg [Am]. 1994;19(2):293-294.
17. Krieger LE, Schnall SB, Holtom PD, et al. Acute gonococcal flexor tenosynovitis. Orthopedics.
1997;20(7):649-650.
18. Iserson K. Telephone consultations from the urgent care center: An educational model. J Urgent Care Med. 2007;1(4):17-21.



